 |
As we continue to try to function in a pandemic, it’s important to maintain an awareness of various billing rules to avoid a loss of revenue. If you take a moment to review your claim payments, you might notice less reimbursement than you’d expected on some services. If the claim is otherwise coded correctly, you have likely encountered a Multiple Procedure Payment Reduction (MPPR).
How MPPR came about
The background of the MPPR is found on the Centers for Medicare and Medicaid Services website fact sheet.1 The article explains the Medicare Physician Fee Schedule proposed rule for 2007 includes proposals to implement two provisions of the Deficit Reduction Act of 2005 that affect payment for imaging services.
The first provision addresses payment for certain multiple imaging procedures, with full payment for the first procedure but a 25-percent reduction in payment for additional imaging procedures furnished on contiguous body parts during the same session.
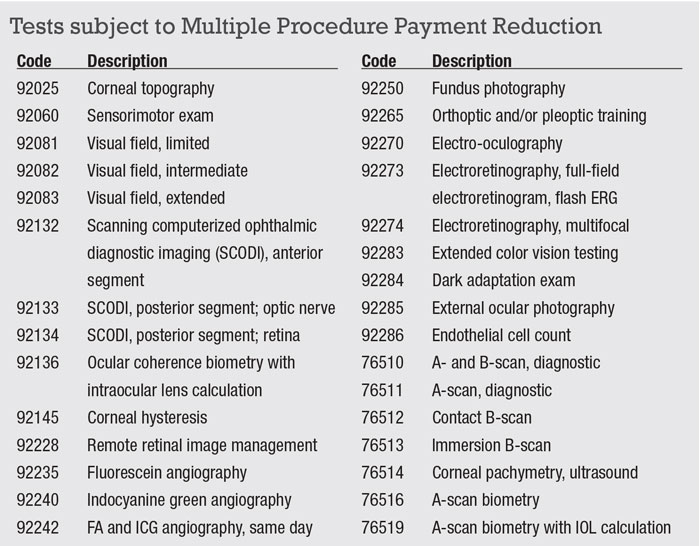
CMS explains that because many services have overlapping components, Medicare is attempting to avoid “duplication of payment” when multiple images of contiguous body parts are taken in a single session. The solution to “duplication of payment” is a reduction in payment for the technical component of the service. The rule doesn’t affect the professional component payment. The list of tests subject to MPPR includes many that are common in a retina clinic (Box): ultrasound, imaging and visual fields.
Where it gets confusing
Since 2013 Medicare has reduced the technical component of second and subsequent ophthalmic tests by 20 percent when more than one eligible diagnostic test is performed on the same day. The professional component of the test is paid in full for each test. Thus, if you perform fundus photography (92250) and fluorescein angiography (92235) on the same day, the technical component of photography will be reduced by 20 percent, or about $4.
Things can become confusing when one test is bilateral and another unilateral, such as a B-scan on one eye (unilateral test payment) and fundus photography both eyes (bilateral payment). One B-scan is paid in full while the second B-scan and the photos are subject to the 20-percent technical component reduction, or about $8 total.
 |
Although you can avoid the reduction by scheduling testing on different dates of service, this is generally not a viable strategy. Costs associated with bringing the patient back another day far exceed the MPPR payment reduction.
The most important point is that you have an understanding of how you are (and are not) getting paid. You (or your billing staff) didn’t make an error; the reduction is built into the Medicare manual. RS
REFERENCE
1. Proposed changes for payment for imaging services under the physician fee schedule required by the Deficit Reduction Act. Centers for Medicare and Medicaid Services website. https://www.cms.gov/newsroom/fact-sheets/proposed-changes-payment-imaging-services-under-physician-fee-schedule-required-deficit-reduction Updated August 8, 2006. Accessed November 10, 2020.



