 |
Bios Dr. Cruz-Pimentel is a Dr. Mandelcorn is an associate professor of ophthalmology at the University of Toronto. Dr. Felfeli is an ophthalmology resident at the University of Toronto. DISCLOSURES: The authors and Dr. Felfeli have no relevant relationships to disclose. |
Patients with endophthalmitis can have a poor outcome after pars plana vitrectomy, particularly when the vitreous cavity has been manipulated significantly. Minimal vitrectomy1 is recommended to prevent further complications, such as surgically induced necrotizing scleritis2,3 and scleral abscess.4
In pseudophakic eyes where the anterior chamber is filled with debris, we recommend using a minimalist two-trocar approach. This technique starts by placing two trocars in the anterior chamber. The first trocar is placed for the infusion line after the infusion that can be opened under direct visualization.
The second trocar cannula is placed in the anterior chamber through which the vitrector is placed to remove the anterior chamber plaque and to collect a first sample for culture and sensitivity (Figure A).
By placing the infusion in the anterior chamber, you can avoid complications from the infusion placement through the pars plana, which include infusion-induced choroidal detachments, particularly given the poor visibility in these cases.
Placing the two trocars
Once the view improves from the anterior chamber washout, two trocars are placed in the superior quadrants to start the posterior vitrectomy in order to collect a second sample from the mid-vitreous cavity.
After this, a core vitrectomy is undertaken. Once there’s a clear view of the posterior pole, the vitrectomy can be stopped (Figure B).
The posterior pole membrane peeling or peripheral vitreous shave is deliberately avoided, given the high risk of retinal tear and detachment in these cases. The infusion line can be removed from the anterior chamber trocar and then placed via the pars plana in the superior temporal quadrant trocar. A partial air-fluid exchange can be done, leaving the vitreous cavity filled with 50 percent air and 50 percent balanced salt solution. Intravitreal antibiotics are then injected in the vitreous cavity.
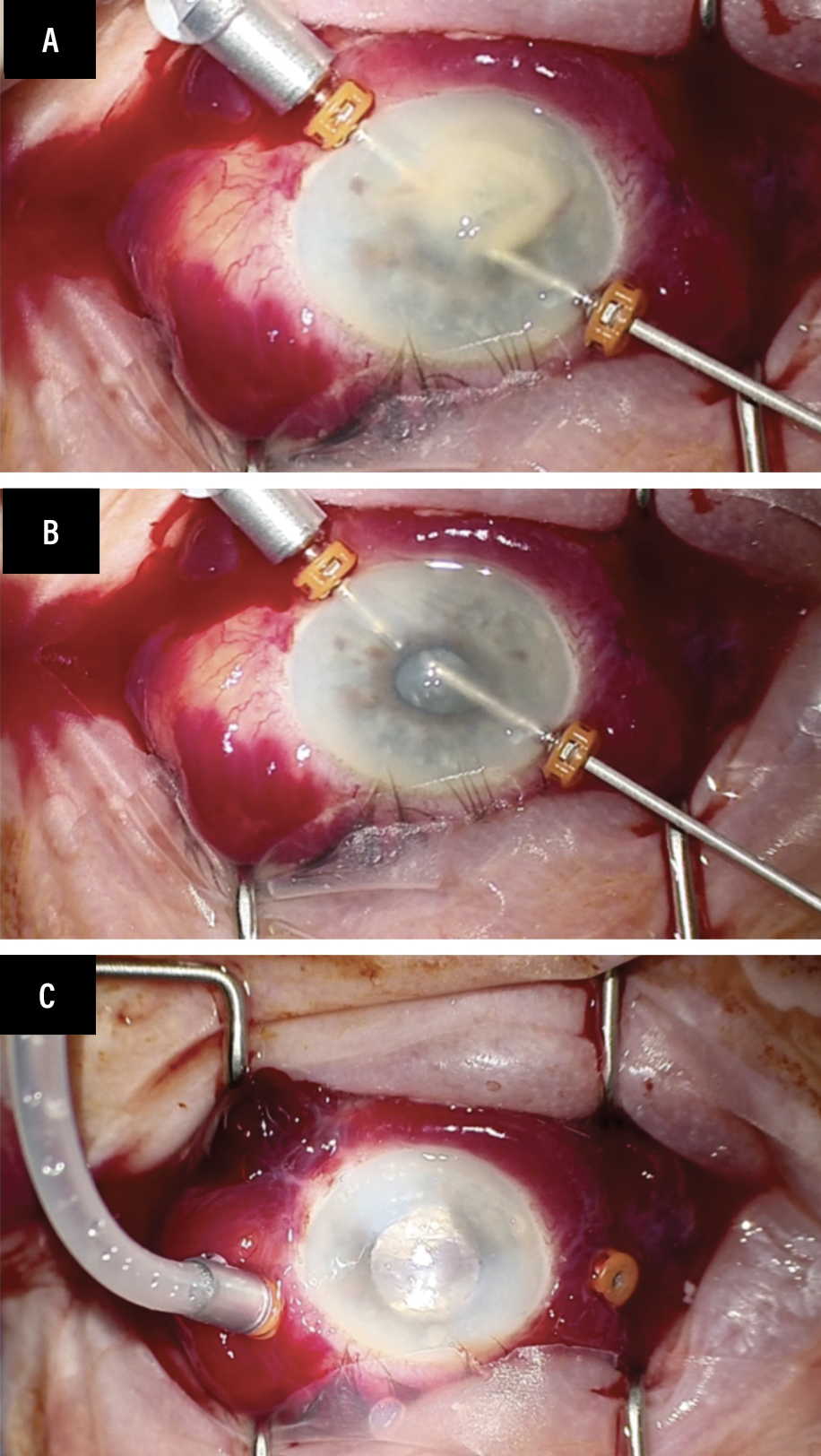 |
| The two-trocar approach. A) The first is used for the infusion line, the second to introduce the vitrector after it’s inserted into the anterior chamber to clean the debris and to collect a first sample for culture and sensitivity. B) Stop the vitrectomy when you get a clear view of the posterior pole. C) Leaving the vitreous cavity filled with 50-50 air and balanced salt solution will ensure the two superior sclerotomies close appropriately and keep the intravitreal antibiotics in the vitreous cavity away from the trocars. |
Leaving the vitreous cavity filled with 50-50 air and BSS will ensure that the two superior sclerotomies close well. At the same time, it will keep the intravitreal antibiotics into the vitreous cavity away from the trocars, preventing any efflux of these medications through the sclerotomies. This step will ensure you administer the full dose and that nothing escapes through the trocars (Figure C).
Bottom line
The minimalist two-trocar approach can avoid complications in pseudophakic eyes with endophthalmitis, such as spreading the infection toward the sclera, causing surgically induced scleritis, scleral abscess and choroidal effusion from placing the infusion into the suprachoroidal space in cases of thick choroid. RS
REFERENCES
1. Davis RM, Rowsey JJ, Jensen HG. An anterior limbal approach to vitrectomy for the surgical management of infectious endophthalmitis. Ophthalmic Surg. 1987;18:683-686.
2. Morley AM, Pavesio C. Surgically induced necrotising scleritis following three-port pars plana vitrectomy without scleral buckling: A series of three cases. Eye (Lond). 2008;22:162-164.
3. Madanagopalan VG, Shivananda N, Krishnan T. Surgically induced necrotizing scleritis after retinal detachment surgery masquerading as scleral abscess. GMS Ophthalmol Cases. 2019;9:Doc18.
4. Saito W, Sakaguchi T, Furudate N, Amino Y, Ohno S. Pseudomonas scleral abscess following pars plana vitrectomy. Jpn J Ophthalmol. 2006;50:564-566.




