 |
 |
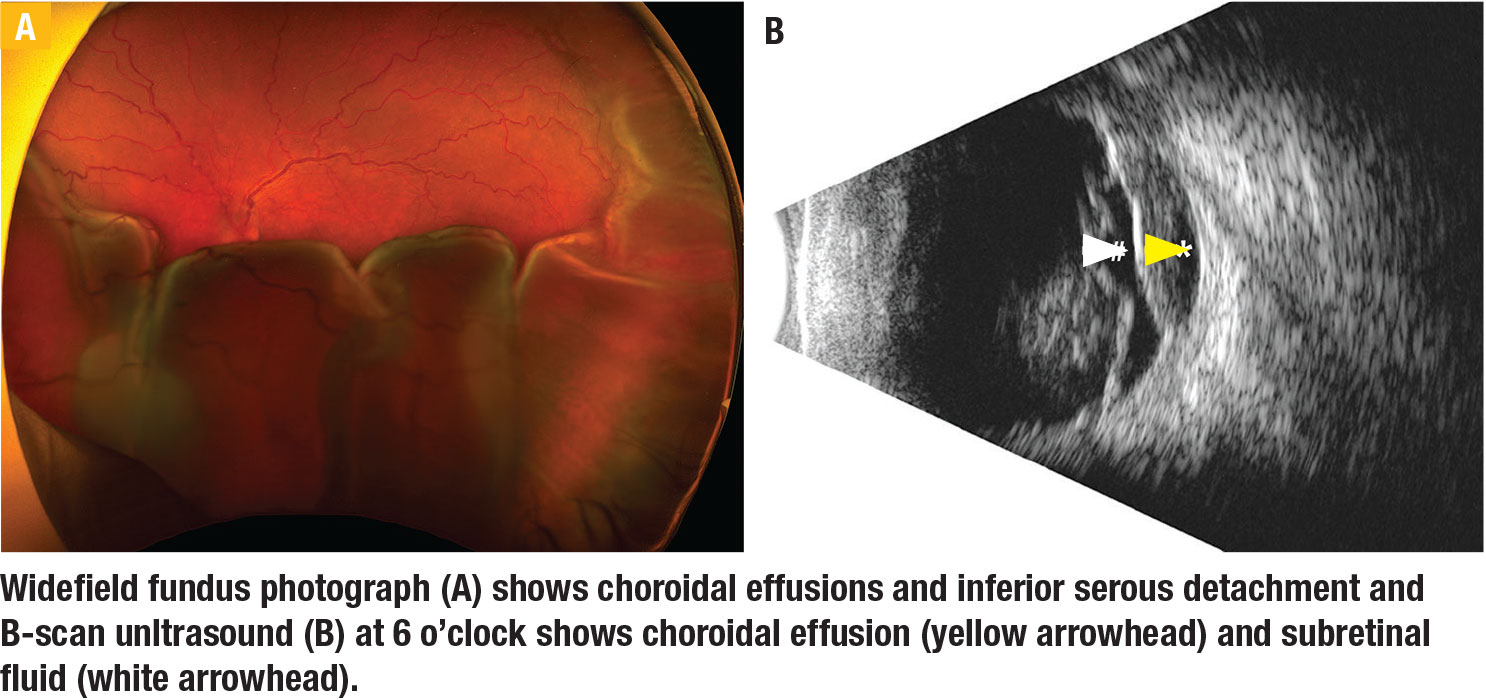
It’s been hypothesized that in a patient with choroidal effusions, especially in the setting of nanophthalmos, the thickened sclera can compress vortex veins and lead to formation and persistence of choroidal effusions and serous retinal detachments. In these cases, scleral windows can increase uveoscleral outflow. For this procedure, careful patient selection with an appropriate discussion of prognosis and expectations is important because the serous retinal detachment usually improves gradually.
Starting the procedure
Exposure is crucial. After a conjunctival peritomy, all four rectus muscles are isolated and tied off with traction sutures. The nanophthalmic eye is notably smaller than what you might expect from scleral buckling.
The key to success is careful dissection of the scleral flap, beginning with an even-depth incision 4 to 5 mm in length parallel to the limbus and approximately 1 to 2 mm posterior to the muscle insertion. A 64- or 75-blade is well suited for this. Meticulous dissection approximately 4 to 5 mm posteriorly with a crescent blade then allows for flap creation.
The sclera is significantly thickened in these cases. You need to establish the appropriate dissection depth. The goal is to see some graying of the remaining sclera, which indicates that it’s appropriately thin. The flap is carried posteriorly and care should be taken not to damage the vortex veins. We prefer to leave the flaps attached posteriorly and amputate at the end of the case to minimize risk of intraoperative hypotony and to help with exposure if sclerotomies need to be enlarged further.
Incising the sclera
We use a 75-blade to incise the sclera radially in the middle of the dissected bed followed by Kelly punch-assisted sclerectomy to allow for drainage of choroidal fluid. We recommend enlarging the sclerotomy by rotating the punch 180 degrees.
 |
It’s important to avoid intraoperative hypotony. Maintain intraocular pressure by pulling on the sutures around the rectus muscles. After each egress of choroidal fluid, adjust the intraocular pressure as needed with balanced salt solution injected into the anterior chamber with a 30-gauge needle.
We typically perform scleral windows in all four quadrants if feasible. Note that with a very thick sclera, the blades can dull; you may need more than one in a case. At the end of the case after careful inspection, the flaps are removed and the conjunctiva is reapproximated at the limbus. RS
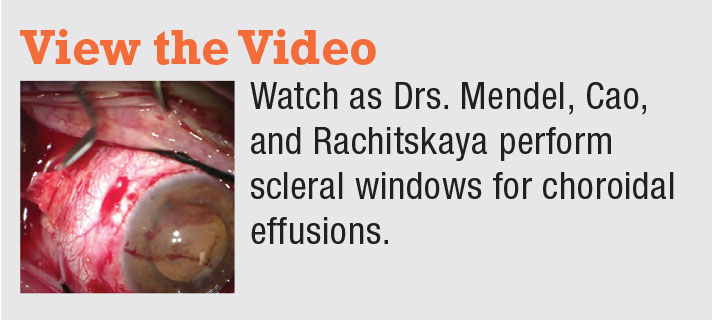 |
Scleral Windows for Choroidal Effusions from Retina Specialist on Vimeo.




