Take-home points
|
 |
|
Bios Dr. Huvard is a clinical assistant professor in the department of ophthalmology and visual sciences, University of Michigan Kellogg Eye, Ann Arbor. DISCLOSURES: Dr. Huvard has no financial disclosures. |
Rhegmatogenous retinal detachment is a major cause of visual loss and one of the most common pathologies retina specialists repair today. Since Prof. Jules Gonin in 1930 first linked retinal breaks to RRD, the fundamental approach to RD repair has remained the same: find the retinal breaks; treat the retinal breaks; and seal the retinal breaks.1
Today, advances in vitreoretinal surgical tools and techniques, particularly microsurgical instrumentation, give retina specialists more tools than ever to treat RRD.
Trends in incisional RRD repair
While the pathogenesis of RRD was recognized in the 1930s, it wasn’t until 20 years later that E. Custodis in Germany developed a polyviol explant and Charles Schepens, MD, and colleagues reported using a polyethylene encircling band to achieve retinal reattachment that established scleral buckling as a surgical technique.2,3
SB remained the primary technique for RRD repair until Robert Machemer, MD, and colleagues introduced pars plana vitrectomy in the 1970s.4 At first, PPV was viewed as a higher-risk surgery and reserved for complicated forms of retinal detachment, such as giant retinal tears or diabetic tractional retinal detachments. But the indications for PPV evolved from complex forms of retinal detachment, often as an adjuvant to SB, to the dominant method for RRD repair today.5 A 2018 survey by the American Society of Retina Specialists showed that SB was used in primary RRD repair in less than 20 percent of cases.6
 |
| Figure 1. Vitreous fluid flows through a retinal tear to cause a partial retinal detachment involving the macula. The optic nerve and nasal retina are normal and uninvolved. Vitrectomy surgery is indicated to restore vision. (Courtesy ASRS Retina Image Bank, contributed by Brandon Busbee, MD). |
Several reasons exist for the rapid adoption of PPV for RRD repair. One is the development of smaller-gauge instrumentation. Compared to SB, growing data show that PPV results in comparatively less pain, surgically induced trauma and morbidity, reduced surgical times and shorter postoperative recovery.7,8 Also, wide-angle viewing systems have enhanced the surgeon’s ability to view vitreoretinal pathology and may improve surgical decision-making.
Aside from RRD repair, the evolution of PPV has been vital in treating a variety of vitreoretinal pathologies, such as full-thickness macular holes, further fueling its adoption.
What the data tell us
As the role of PPV has expanded, much debate has revolved around defining the optimal surgical technique for retinal reattachment. While PPV alone is best for RRD repair in many cases, PPV/SB and primary SB remain widely employed (Figure 1).6 Potential drivers of technique preference are patient age, lens status, presence of a posterior vitreous detachment, extent of the retinal detachment, macular status, location of retinal breaks (below the horizontal meridian), the presence of media opacity (e.g., vitreous hemorrhage) and presence of proliferative vitreoretinopathy.
The most recent large, prospective randomized clinical trial to assess this question was the Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment (SPR) study in 2007.8 This study enrolled more than 500 eyes with medium-complexity RRD—defined as RRD with retinal breaks 1 to 2 clock hours in size—marked vitreous traction, multiple breaks, central extension of the break or superior bullous detachment.9 The study found that single-surgery anatomic success (SSAS) was the same in phakic eyes treated with PPV (63.8 percent) or SB (63.6 percent), but visual outcomes were superior in the SB group. Pseudophakic or aphakic eyes fared better with PPV than with SB (SSAS of 72 vs. 53.4 percent). No difference in best-corrected visual acuity was found.9
 |
While the SPR study provided a wealth of data and contributed to our surgical decision-making, its findings may not be generalizable to the current landscape of modern microincisional vitrectomy. The study data were gathered between 1998 and 2003, which predated small-gauge vitrectomy.
In addition, the trial design allowed surgeons to place a supplemental SB in combination with PPV at their discretion. About 50 percent of the cases of primary PPV had a SB placed, which makes it difficult to interpret the true outcomes of PPV vs. PPV/SB or SB. Finally, because the SPR study only considered moderate-complexity cases, non-complex RRD—cases with a single break in a young myopic patient with attached hyaloid, which would overwhelmingly be treated with SB—aren’t included.
More recent evidence
Several large, retrospective interventional case series have sought to answer similar questions in the context of modern surgical practices. The Primary Retinal Detachment Outcomes Study (PROS) is a multi-institutional effort that evaluated surgical outcomes in noncomplex RRD repair based on cases performed at five sites in 2015.10 The distribution of surgical procedures used to treat primary RRD was in line with current trends: 51.7 percent used PPV, 34.8 percent PPV/SB and 13.5 percent primary SB, with a strong preference for performing primary SB in patients younger than 40 years.
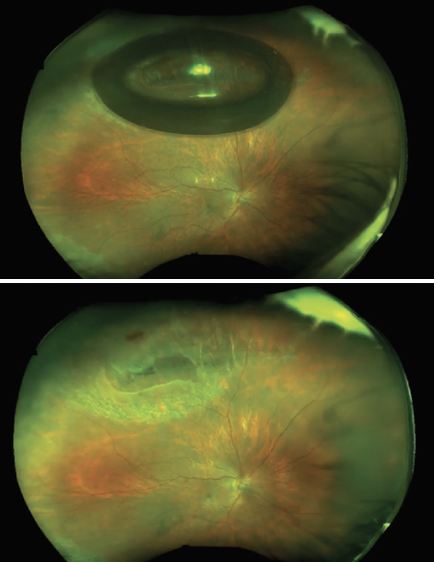 |
| Figure 2. Widefield imaging of a superior macula-off retinal detachment after pneumatic retinopexy shows the retina fully attached, the superior break lasered after 48 hours (top) and the gas bubble fully resorbed. (Courtesy Efrem D. Mandelcorn, MD, FRCSC) |
The investigators report high rates of SSAS in patients managed with SB (91.2 percent) or PPV/SB (90.2 percent), but notably report a lower SSAS (84.2 percent)in patients managed with PPV alone. Subgroup analysis showed that PPV/SB and SB offered better SSAS than PPV in phakic eyes: 91.2 and 91.7 vs. 83.1 percent.
Pseudophakic eyes similarly fared better with PPV/SB compared to PPV (92 vs. 84 percent), but mean BCVA wasn’t significantly different. Eyes with inferior retinal breaks also had higher SSAS after combined PPV/SB compared to PPV (87.4 vs. 76.8 percent).
These data are similar to a recent report by Jose J. Echegaray, MD, and colleagues that reviewed primary RRD outcomes of 488 eyes from a single institution between 2014 and 2017.11 They reported SSAS of 81.1 percent with PPV vs. 92.2 percent with PPV/SB for all detachments. A subgroup analysis showed superior SSAS with PPV/SB in phakic patients, but not pseudophakic patients.11
Excellent results of PPV alone
However, other large interventional case series have reported SSAS of 90 percent or better with PPV alone.12 A recent single-institution study by Omar Moinuddin, MD, and colleagues reported primary RRD outcomes of 751 cases from 2011 to 2019, showing high SSAS with PPV, PPV/SB or SB (91.2, 84.3 and 93.8 percent, respectively).13
In a subgroup analysis of patients with inferior retinal breaks, they reported a high SSAS (88.9 percent) and final anatomic success (FAS) (96.2 percent) of primary RRD with inferior breaks managed by PPV alone.
Similarly, lens status wasn’t found to be significant in predicting SSAS or FAS with comparable outcomes between all surgical modalities. Patients managed with combined PPV/SB or PPV or SB alone demonstrated excellent and comparable BCVA outcomes, suggesting that supplementing PPV with SB didn’t improve anatomic or visual outcomes.
Others have also published excellent outcomes of treating RRD with inferior retinal breaks with small-gauge PPV alone.14 Among the studies previously discussed, many surgeons opted to use PPV/SB (PROS 34.8 percent, Dr. Echegaray 67 percent) rather than primary PPV. This may suggest these surgeons are more comfortable with PPV/SB as they achieved superior results with this approach. Dr. Moinuddin and colleagues, who only utilized PPV/SB in 6.8 percent of their reported cases, opted for PPV alone (89 percent of cases) with excellent and comparable results to PROS and Dr. Echegaray.
The literature for incisional treatment of RRD is extensive even with the lack of high-quality evidence supporting one practice over another. Indeed, a Cochrane review in 2019 found nothing more than “low-certainty” evidence supporting use of PPV over SB for simple RRD.15 Another meta-analysis of 10 studies from 2003 to 2014 with 1,704 patients concluded that SSAS of PPV/SB was superior to PPV. However, these authors also included patients with complex forms of RRD (e.g., advanced PVR and giant retinal tears) and those in whom 20-gauge instruments were used. Thus, the findings may not be generalizable to modern, small-gauge uncomplicated RRD repair.
In the recent Pneumatic Retinopexy Versus Vitrectomy for the Management of Primary Rhegmatogenous Retinal Detachment Outcomes Randomized Trial (PIVOT), the SSAS of PPV was 93 percent.16 RRD are heterogenous and hence difficult to compare. Surgeons should opt for retinal reattachment techniques that draw on their training, preferences and experience individualized to each patient to achieve the greatest chance of success.
Nonincisional alternatives
Pneumatic retinopexy (PnR) is an office-based procedure that may be an excellent alternative to incisional repair for non-complex retinal detachments. Most agree the standard criteria that define a good candidate for PnR include an RRD with a single or clustered retinal breaks (usually in the superior clock hours), phakic lens status and the absence of other high-risk pathology such as lattice degeneration. PnR (Figure 2) offers a number of potential advantages over incisional techniques, including faster VA recovery and avoiding the operating room and its associated risks.16
PIVOT, a 2019 randomized clinical trial, compared outcomes of PnR vs. PPV for the management of non-complex RRD.16 The authors reported SSAS of 81 and 93 percent for PnR and PPV, respectively. Their findings underscore that PnR can be an excellent technique with strict patient selection criteria and good surgeon skill.
However, since 2004, PnR procedures have declined and fewer physicians are as comfortable with the technique.5 To this end, Nicholas Yannuzzi, MD, and colleagues reviewed American Academy of Ophthalmology IRIS Registry outcomes of 9,553 patients who had PnR.17 They reported an overall SSAS of 68.5 percent, perhaps more in line with real-world results.
One interesting finding from PIVOT was that PnR-treated eyes had better BCVA and less metamorphopsia than PPV-treated eyes. However, a growing body of literature suggests that visual acuity alone is an insufficient proxy for vision and vision-related quality of life after RRD.18 We need more research to better understand what metrics may best capture vision-related changes after RRD.
Finally, it’s prudent to remember that some patients may be excellent candidates for laser demarcation.19,20 Ideal candidates include those with asymptomatic, peripheral RRDs that spare the macula or who are unable or unwilling to undergo more invasive procedures.
Bottom line
RRD remains a significant cause of visual morbidity and vision loss. With advances in surgical technique and improved instrumentation, SSAS greater than 90 percent is possible with a variety of incisional techniques.
Nonincisional techniques remain an important alternative in select patients. Surgeons should feel confident in selecting a technique reflective of their training; one that works best in their hands. Factors such as patient age or lens status, in combination with surgeon experience and judgment, should help guide individualized treatment recommendations for each patient. RS
REFERENCES
1. Gonin J. The treatment of detached retina by searing the retinal tears. Arch Ophthalmol. 1930;4:621-625.
2. Custodis E. Die Behandlung der netzhautablösung durch umschriebene diathermiekoagulation und einer mittels plombenaufnähung erzeugten eindellung der sklera im bereich des risses. [Treatment of retinal detachment by circumscribed diatheramal coagulation and by scleral depression in the ara of tear caused by imbedding of a plastic implant] Klin Monbl Augenheilkd Augenarztl Fortbild. 1956;129:476-495.
3. Schepens CL, Okamura ID, Brockhurst RJ. The scleral buckling procedures. I. Surgical techniques and management. AMA Arch Ophthalmol. 1957;58:797-811.
4. Machemer R, Buettner H, Norton EW, Parel JM. Vitrectomy: A pars plana approach. Trans - Am Acad Ophthalmol Otolaryngol Am Acad Ophthalmol Otolaryngol. 1971;75:813-820.
5. McLaughlin MD, Hwang JC. Trends in vitreoretinal procedures for Medicare beneficiaries, 2000 to 2014. Ophthalmology. 2017;124:667-673.
6. Singh RP, Stone TW, eds. 2018 Global Trends in Retina; Chicago, IL. American Society of Retina Specialists; 2018.
7. Lakhanpal RR, Humayun MS, de Juan E, et al. Outcomes of 140 consecutive cases of 25-gauge transconjunctival surgery for posterior segment disease. Ophthalmology. 2005;112:817-824.
8. Thompson JT. Advantages and limitations of small gauge vitrectomy. Surv Ophthalmol. 2011;56:162-172.
9. Heimann H, Bartz-Schmidt KU, Bornfeld N, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: A prospective randomized multicenter clinical study. Ophthalmology. 2007;114:2142-2154.
10. Ryan EH, Joseph DP, Ryan CM, et al. Primary Retinal Detachment Outcomes Study: Methodology and overall outcomes–Primary Retinal Detachment Outcomes Study Report Number 1. Ophthalmol Retina. 2020;4:814-822.
11. Echegaray JJ, Vanner EA, Zhang L, et al. Outcomes of pars plana vitrectomy alone versus combined scleral buckling plus pars plana vitrectomy for primary retinal detachment. Ophthalmol Retina. 2021;5:169-175.
12. Schneider EW, Geraets RL, Johnson MW. Pars plana vitrectomy without adjuvant procedures for repair of primary rhegmatogenous retinal detachment. Retina. 2012;32:213-219.
13. Moinuddin O, Abuzaitoun RO, Hwang MW, et al. Surgical repair of primary non-complex rhegmatogenous retinal detachment in the modern era of small-gauge vitrectomy. BMJ Open Ophthalmol. 2021;6:e000651.
14. Martínez-Castillo V, Boixadera A, Verdugo A, García-Arumí J. Pars plana vitrectomy alone for the management of inferior breaks in pseudophakic retinal detachment without facedown position. Ophthalmology. 2005;112:1222-1226.
15. Znaor L, Medic A, Binder S, Vucinovic A, Marin Lovric J, Puljak L. Pars plana vitrectomy versus scleral buckling for repairing simple rhegmatogenous retinal detachments. Cochrane Database Syst Rev. 2019;3:CD009562. doi:10.1002/14651858.CD009562.pub2
16. Hillier RJ, Felfeli T, Berger AR, et al. The Pneumatic Retinopexy versus Vitrectomy for the Management of Primary Rhegmatogenous Retinal Detachment Outcomes Randomized Trial (PIVOT). Ophthalmology. 2019;126:531-539.
17. Yannuzzi NA, Li C, Fujino D, et al. Clinical outcomes of rhegmatogenous retinal detachment treated with pneumatic retinopexy. JAMA Ophthalmol. 2021;139:848-853.
18. Ng H, Vermeer KA, van Meurs JC, La Heij EC. Visual acuity inadequately reflects vision-related quality of life in patients after macula-off retinal detachment surgery. Invest Ophthalmol Vis Sci. 2020;61:34.
19. Greenberg PB, Baumal CR. Laser therapy for rhegmatogenous retinal detachment. Curr Opin Ophthalmol. 2001;12:171-174.
20. Shukla D, Maheshwari R, Kim R. Barrage laser photocoagulation for macula-sparing asymptomatic clinical rhegmatogenous retinal detachments. Eye Lond Engl. 2007;21:742-745.



