 |
 |
While there is no established standard of care for postoperative drops, a common regimen is an antibiotic drop four times a day for a week, a cycloplegic drop twice a day for a week and a steroid drop starting four times a day and tapering off over a period of four to six weeks. The rationale is that antibiotics lower the risk of infection, cycloplegics lower the risk of posterior synechiae and pain, and steroids reduce the risk of inflammatory sequelae such as pain, photophobia, fibrin and synechiae.
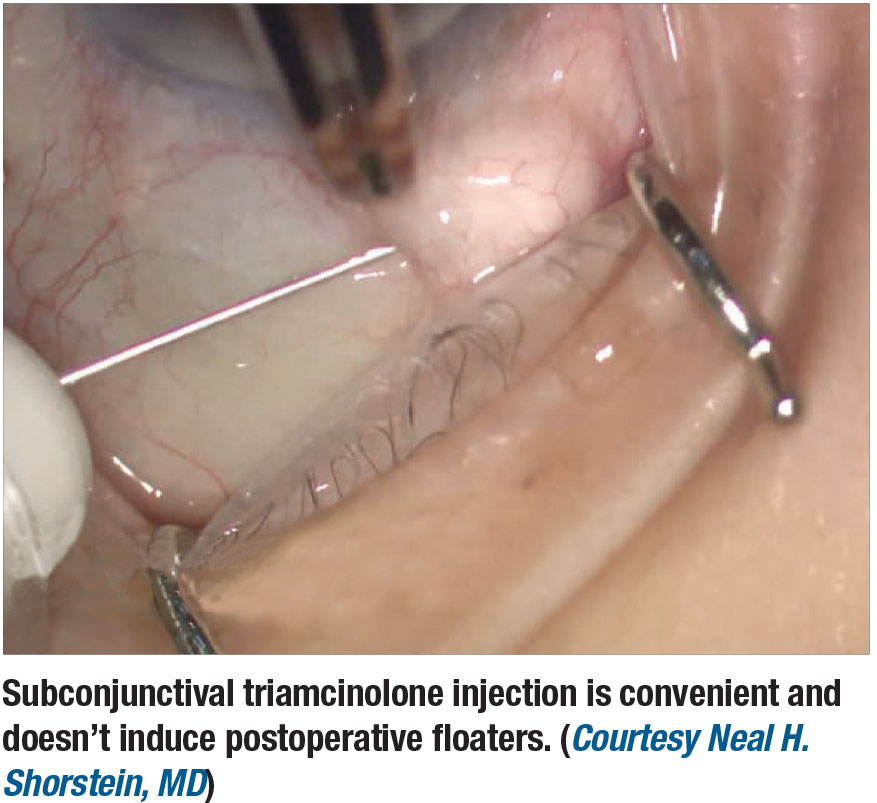
However, the literature lacks support for the clinical efficacy of this approach, and some cataract surgeons have started moving away from routine use of postoperative drops with good results. A similar approach may succeed in vitreoretinal surgery. Here, we discuss our own work that has shown the potential benefits of a subconjunctival triamcinolone injection after vitreoretinal surgery.
The burden of postoperative drops
An informal survey of 41 U.S. retinal specialists queried on their routine peri- and postoperative use of ocular steroids found that all respondents (41 of 41) prophylactically treat postoperative inflammation with some form of steroid after surgery (J. Pollack, personal communication June 2018). Ninety-eight percent (40 of 41) reported using postoperative steroid drops, with 68 percent (28 of 41) supplementing steroid drops with a subconjunctival steroid injection at the end of surgery.
Most (83 percent, 33 of 40) stated that they place patients on a prolonged steroid taper starting at four times a day and tapering over a four to six weeks. The single surgeon who didn’t use drops was using a single subconjunctival injection of 4 mg triamcinolone acetonide at the end of each case, regardless of case complexity, without subsequent steroid drops.
Postoperative drops are a known burden for patients. In addition to their expense, many patients lack the visual acuity and/or dexterity to reliably get drops in their eye, requiring another person to help them. Studies in the cataract literature have found a compliance rate lower than 10 percent for those having surgery for the first time, with the most common errors being missing the eye, contamination of the bottle tip and using an incorrect number of drops.1
Design of our study
 |
Recently, some cataract surgeons have started seeking an alternative to the routine use of postoperative drops, with good clinical outcomes and excellent patient acceptance.2 In our retrospective case review study, we examined whether vitreoretinal surgeons may also be able to lessen the postoperative eye drop burden by eliminating the traditional postoperative steroid drop taper. This would decrease the time patients are on drops by 75 to 83 percent, and decrease the total number of drops after surgery by over 60 percent compared with the traditional drop regimen.3
In this study, we compared all patients of two surgeons undergoing vitreoretinal surgery during the study period. One surgeon routinely used a single subconjunctival injection of 4-mg triamcinolone acetonide at the end of the case (intervention group), while the other used 1 mg subconjunctival injection of dexamethasone at the end of the case plus a traditional one-month topical steroid drop taper (control group). Patients who were on steroids within a week before surgery or who lacked at least 90 days of follow-up were excluded. Patients in both groups were also prescribed 1% atropine eyedrops b.i.d. and antibiotic drops (moxifloxacin unless contraindicated by allergy) q.i.d. Other eye drops were prescribed if indicated by individual patient course at the surgeon’s discretion.
The control group consisted of 163 surgeries in 146 patients, the intervention group 161 surgeries in 135 patients. Demographics between the two groups were similar in terms of gender, age, or preoperative diagnosis of glaucoma or steroid responsive ocular hypertension.
The most common types of retinal surgery were vitrectomy (37 percent of controls and 29 percent of intervention group cases) and vitrectomy plus C3F8 gas (23 percent and 30 percent, respectively). Scleral buckles, vitrectomy/buckles and vitrectomy with oil comprised 12 and 15 percent of the respective totals. There were no statistically significant differences in the types of surgery between the control and intervention groups (p-values between 0.1 and 0.84).
 |
No difference in IOP
There was also no statistically significant difference in intraocular pressure-related outcomes between the intervention and control groups, with 12 and 16 percent in the respective groups requiring additional IOP-lowering drops postoperatively (p=0.08). Twelve percent of controls and 16 percent in the intervention group developed IOP >29 mmHg during the postoperative period (p=0.31), and 14 and 20 percent, respectively, had an IOP increase ≥10 mmHg postoperatively (p=0.12).
New posterior synechiae and anterior chamber cell at one week were rare in both groups at less than 1 percent. Five percent of patients in the intervention group received supplemental postoperative steroid drops due to anterior chamber cell.
In both groups, IOP-related complications were more common in those with a history of glaucoma or steroid response before surgery, with 21 percent of the former and 44 percent of steroid responders developing IOP > 29 mmHg postoperatively vs. 12 percent without such a history. Similarly, 42 percent of those with a history of glaucoma and 44 percent with a history of steroid response had an IOP increase of ≥ 10 mmHg during the postoperative period compared with 12 percent without such a history.
 |
What this study adds to our knowledge
The results of this study suggest that a single subconjunctival injection of 4 mg triamcinolone acetonide at the end of retina surgery cases may be equal in effectiveness and safety to 1 mg subconjunctival dexamethasone plus a one-month topical steroid taper. There was no evidence of increased risks of IOP-related complications or inflammatory complications associated with the single injection. Regardless of the type of steroid used, patients with a history of glaucoma or IOP response were at higher risk of elevated IOP after vitreoretinal surgery.
Limitations
Because this was a case-review study, systemic differences in the patient populations may exist between the two surgeons, despite them operating out of the same offices. There was no protocol for when IOP drops were added after surgery and the surgeons may have differed in their thresholds for starting such drops. Similarly, there was no criteria for which patients received supplemental steroid drops after surgery in the intervention group.
Other surgeons may have higher or lower rates of supplemental drop use depending on their individual threshold. Both surgeons operated in sites that routinely added 10 mg of dexamethasone to the vitrectomy infusion solution, which may alter the rates of inflammatory complications compared to surgeons who do not routinely add steroid to the infusion.
Bottom line
A single subconjunctival of 4 mg triamcinolone acetonide at the end of retina surgery cases is a reasonable alternative to subconjunctival injection of 1 mg dexamethasone at the end of the case plus a traditional steroid drop taper. RS
REFERENCES
1. An JA, Kasner O, Samek DA, Levesque V. Evaluation of eyedrop administration by inexperienced patients after cataract surgery. J Cataract Refract Surg. 2014;40:1857-1861.
2. Lindstrom RL, Galloway MS, Grzybowski A, Liegner JT. Dropless cataract surgery: An overview. Curr Pharm Des. 2017;23: 558-564.
3. Atchison EA, Gilca M, Civantos JM, Pollack JS. Elimination of steroid drops after vitreoretinal surgery. journal of vitreoretinal diseases. In press 2019.



