 |
Bios |
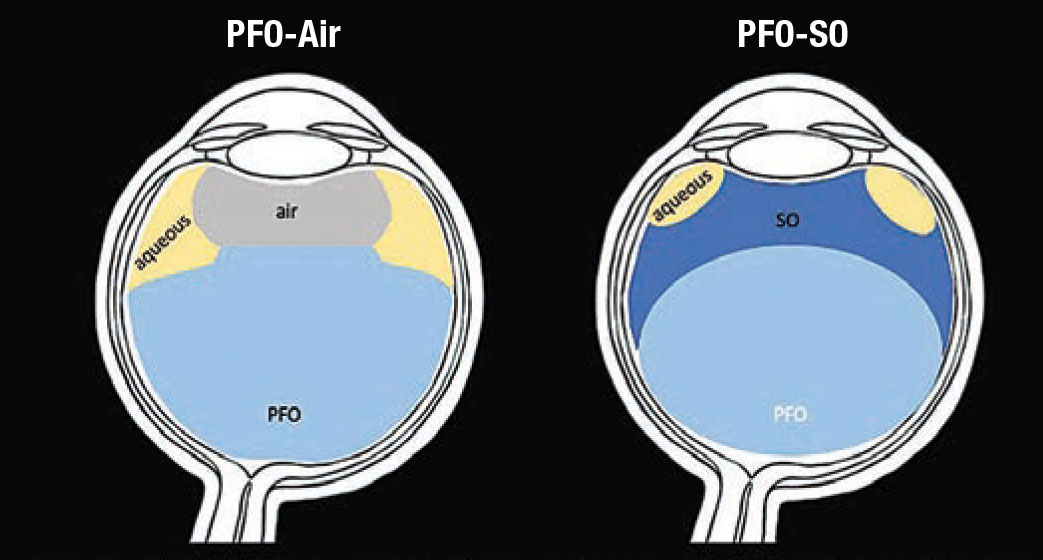
Perfluorocarbon-silicone oil exchange is an important technique for minimizing the retinal slippage that can occur with PFO-air exchange during, for example, the repair of giant retinal tears, or after a relaxing retinectomy. When air comes in contact with PFO, it forms a relatively flat interface, displacing aqueous laterally and posteriorly (Figure 1).1 Aqueous is able to dissect the retinal break and flow posteriorly in the subretinal space. Conversely, as SO is instilled, it’s pulled down and spread out over the PFO bubble, displacing aqueous superiorly (and laterally), preventing retinal slippage (Figure 1).1
 |
|
Figure 1. An air bubble has a fairly flat base when it comes in contact with perfluorocarbon, displacing aqueous laterally and posteriorly. In PFO-air exchange, this posterior trajectory of aqueous can dissect the retinal break and flow in the subretinal space. In PFO-silicone oil exchange, SO is pulled down and spread out over the PFO bubble, forming an interface that expels aqueous laterally and superiorly, thus minimizing retinal slippage. (Concept adapted from Wong D, et al. Graefe’s Arch Clin Exp Ophthalmol. 1998;236:234-237. Illustrations by Tahsin Khundkar, MD) |
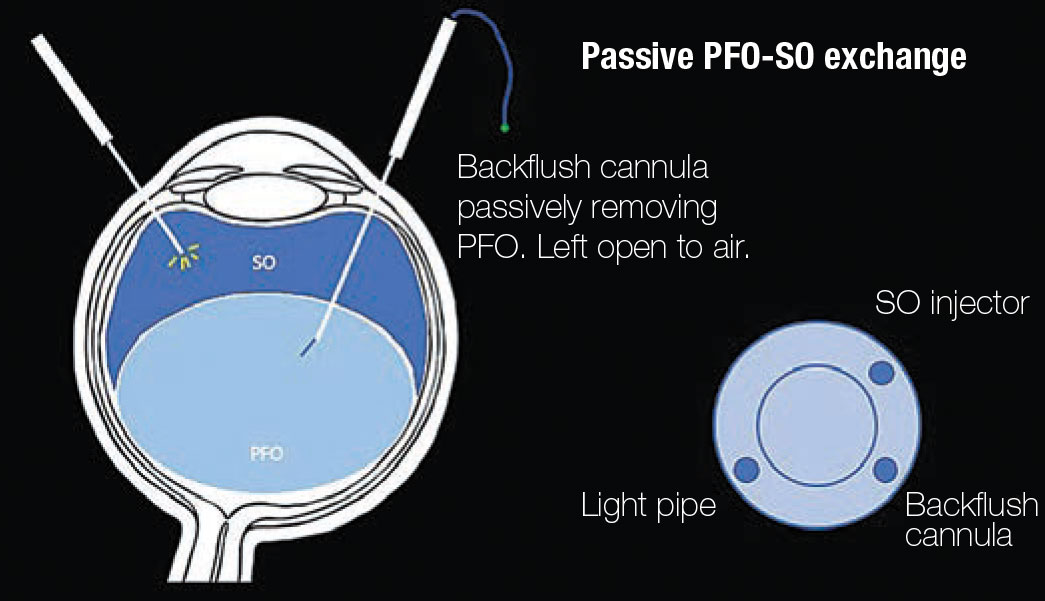 |
| Figure 2. Schematic of the perfluorocarbon-silicone oil exchange. The surgeon holds a light source and a soft-tip backflush cannula that’s left open to air. As SO is injected, the backflush cannula is maintained in the PFO meniscus and PFO is passively expelled. |
PFO-SO exchange can be achieved using a dual-active injection/extrusion mode in the vitrectomy machine.2 Here, we highlight our preferred method of passive PFO-SO exchange, which involves actively injecting SO while passively extruding PFO with a backflush cannula (Figure 2).
Surgical Technique
Three-port vitrectomy and any necessary steps are performed to flatten the retina. With the vitreous cavity filled with PFO, the infusion line is removed and the SO injector is held in the empty cannula by an assistant. The surgeon actively injects SO with a foot-
pedal-controlled viscous fluid injection while holding the light source in one hand and a soft-tip backflush cannula that’s left open to air in the other.
Alternatively, a chandelier illuminator can be used to free up the surgeon’s hand to hold the SO injector. Active injection of SO is titrated by slowing down, or stopping and waiting, based on the optic nerve perfusion or a tactile estimation of the intraocular pressure.
Initially, the backflush cannula is placed just posterior to the floating SO in order to remove the middle aqueous layer. Next, if there is residual aqueous, the cannula is directed to the edge of the retinal break. Finally, once the SO meniscus passes the posterior edge of the retinal break, the backflush cannula is redirected to the optic nerve to remove the remaining PFO.
Why use passive aspiration?
An advantage of passive aspiration is that the surgeon doesn’t have to change any parameters in the vitrectomy machine or prime infusion tubing. While this is particularly useful in certain cases, such as when trying to prevent dislodgement of a retinal free-flap during closure of a refractory macular hole,3 this technique can be used in any case in which SO is planned.
We encourage you to practice this technique regularly to become familiar with it. RS
REFERENCES
1. Wong D, Williams RL, German MJ. Exchange of perfluorodecalin for gas or oil: A model for avoiding slippage. Graefe’s Arch Clin Exp Ophthalmol. 1998;236:234-237.
2. Ahmad KT, Sallam AB, Saad AA, Ellabban AA. Fully automated direct perfluorocarbon liquid-silicone oil exchange. Clin Ophthalmol. 2020;14:4355-4358.
3. Grewal DS, Mahmoud TH. Autologous neurosensory retinal free flap for closure of refractory myopic macular holes. JAMA Ophthalmol. 2016;134:229-230.




