| Retina Standouts from ASRS 2020 |
 |
 |
 |
For the first time in its history, the annual meeting of the American Society of Retina Specialists occurred virtually due to the ongoing COVID-19 pandemic. Leading retina specialists from around the world came together online to demonstrate how rapidly the field of retina is advancing.
Here, we present five intriguing presentations: management of proliferative vitreoretinopathy (PVR) using intravitreal methotrexate; optogenetics for retinitis pigmentosa; and three novel techniques to close persistent and/or large macular holes.
PVR management using treat-and-extend methotrexate
PVR continues to be every retina surgeon’s worst nightmare. Previous studies in animal models and humans have shown efficacy of PVR prevention with the use of intravitreal methotrexate. Scott D. Walter, MD, MSc, presented a study that looked at a more manageable treat-and-extend protocol for the use of intravitreal methotrexate (400 μg/0.1 mL) in these patients.1
Initial loading doses were administered every one to two weeks after surgery until the lasered edge of the retinectomy had matured and stabilized. Then the treatment interval was extended into the three- to six-week range until silicone oil removal.
Previous protocol recommendations included approximately 12 injections before silicone oil removal, but most patients in this study received six or fewer injections, with a median of three during the loading phase and a median of two during the extension phase. An additional injection was given at the time of silicone oil removal.
The updated series included 50 eyes of 50 patients with severe grade B or grade C PVR. The final reattachment rate was 96 percent, and the single-operation success rate 88 percent; 78 percent achieved ambulatory vision at last follow-up. Notably, nearly 40 percent developed keratopathy.
PVR remains one of the greatest challenges in vitreoretinal surgery. Intravitreal methotrexate appears to be effective at mitigating the risk of PVR formation. Previous protocols, however, were quite burdensome. This study suggests that similar outcomes may be achieved with a less onerous treat-and-extend injection protocol. That may convince more surgeons to adopt this treatment for high-risk patients.
Dr. Walter, of Hartford Hospital and the University of Connecticut School of Medicine, disclosed financial relationships with Allergan/AbbVie, Castle Biosciences and Genentech/Roche.
 |
Optogenetics as an option for nonsyndromic RP
More than 100 different genetic mutations can cause RP. Targeting each mutation with gene therapy would be a costly and extremely difficult task for our scientific community. Optogenetics is a technique in which genetic modification of a neuron encodes a light-sensitive opsin protein, allowing neuronal cells to respond to light stimulation. In the retina, this therapy involves genetic modification of ganglion cells with a channel rhodopsin that makes retinal ganglion cells photosensitive.
In retinal diseases like RP that result in photoreceptor loss, conferring photosensitivity in retinal ganglion cells may potentially restore vision. Optogenetic gene therapy is “gene agnostic,” meaning that it could theoretically be utilized for any of the mutations causing RP.
PIONEER is a first in-human dose-escalation trial of patients with end-stage nonsyndromic RP (light perception or worse vision) regardless of the underlying genetic defect.2 The treatment combines the simultaneous action of a gene therapy with a light-stimulating medical device.
A single intravitreal injection delivers viral vectors carrying the gene encoding ChrimsonR, a light-sensitive opsin derived from green algae. It targets the retinal ganglion cells to make them photosensitive upon gene transfer. After the injection, the patient wears photostimulating goggles with an event-based camera and a projection amplifying light source. These goggles amplify light onto the retina to overcome the low light sensitivity of the ChrimsonR channel rhodopsin. Low-vision and vision training sessions after treatment teach the patient how to use the device.
Joseph Martel, MD, reported no serious adverse events in seven patients in the trial. All patients tolerated the light-stimulating goggles well. The most common ocular adverse event was mild intraocular inflammation, which responded to topical corticosteroids.
Optogenetic gene therapy is an exciting new approach to treatment for inherited retinal diseases that could also be applied to other retinal diseases causing photoreceptor loss. Long-term visual outcomes for the patients in the PIONEER trial will be highly anticipated by the retina community.
Dr. Martel of the University of Pittsburgh has no relevant financial disclosures.
Novel surgical techniques for large or persistent macular holes
In recent years, several novel techniques for closing large and/or persistent full-thickness macular holes have emerged with varying degrees of success. Complications include inverted internal limiting membrane flaps, lens capsular flap transplantation and macular hole hydrodissection. Each technique has advantages and disadvantages, and surgeon preference can vary. These three presentations described positive outcomes of novel techniques.
Multilayered inverted ILM flap
This technique is useful in eyes with large macular holes (>700 μm) without a previous ILM peel. It involves a vitrectomy followed by creation of a multilayered inverted ILM flap. Srinavas Joshi, MD, reported on the technique of creating multiple ILM flaps in a “petaloid” fashion using ILM forceps and starting 1 to 2 disc diameters from the macular hole.3
The ILM “petals” were placed one over the other in the macular hole under perfluorocarbon liquid (PFCL). Intraoperative OCT confirmed the position of the stacked ILM flaps. All cases used C3F8 gas and required one week of postoperative prone positioning.
Dr. Joshi reviewed 103 eyes of 99 patients. Mean minimum macular hole diameter was 711.96 μm, and mean basal diameter 1,390.14 μm. At three months postop, 92.2 percent achieved type 1 closure, 5.8 percent type 2 closure and 1.9 percent type 3 closure. Mean preoperative best-corrected visual acuity was around 20/320 and improved to 20/125 at three months.
A conventional inverted ILM flap carries a risk of dislodging from the hole during fluid-air exchange (FAX). The rate of spontaneous detachment of the flap was 14 percent in the original published case series. With the multilayered technique, even if one flap petal becomes dislodged, multiple additional ILM flaps remain to promote closure. In this series, none of the 103 eyes had flap dislodgement during FAX.
One distinct disadvantage of this technique is the high cost of using PFCL for the ILM peel. Furthermore, peeling ILM under PFCL can be technically challenging.
Dr. Joshi of the M.M. Joshi Eye Institute, Hubli, India, has no relevant disclosures.
Amniotic membrane transplant
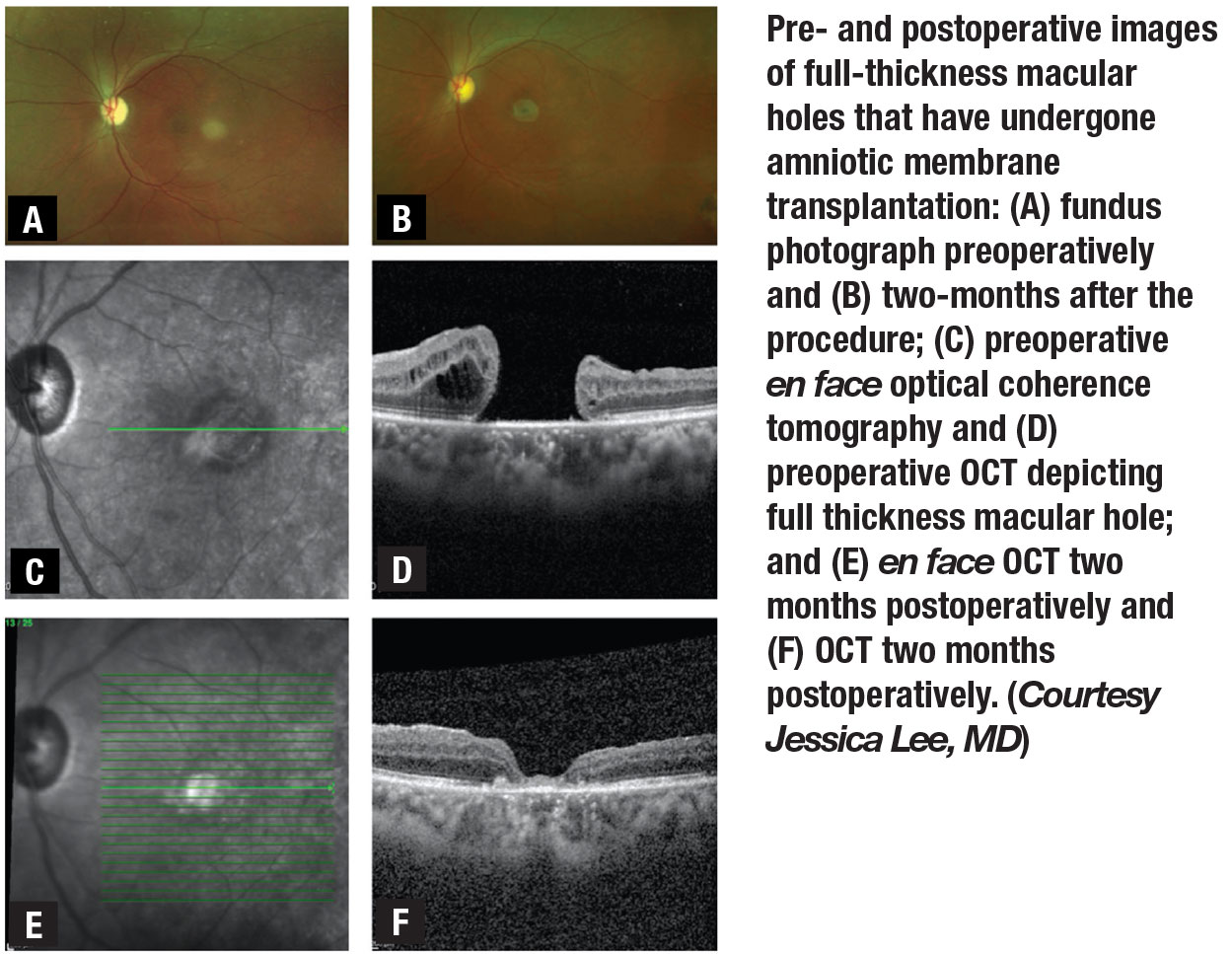 |
This technique uses forceps to insert a folded, circularly-punched patch of amniotic membrane through a valved trocar and into the macular hole (Figure). Jessica Lee, MD, described the outcomes of amniotic membrane transplantation in eight patients with persistently open large macular holes after vitrectomy with ILM peeling.4 Six patients had tamponade with gas and two with silicone oil. All holes were closed at the one-week postop visit. Mean BCVA improved from 20/1,000 to 20/320 at three months for five holes.
One advantage of this technique is that it eliminates the need to harvest an ILM flap outside the macula center, which can be tedious and difficult in eyes with previous large-diameter ILM peels. It also provides a safer substrate to “bridge” large holes than autologous retinal transplantation, which has a higher risk of retinal detachment.
Disadvantages include the additional cost of using an amniotic membrane and the degree of difficulty associated with preparation and appropriate insertion of the amniotic membrane into the hole.
Dr. Lee of New York Eye and Ear has no relevant financial disclosures.
Paracentral retinotomy
This relatively simple yet effective technique involves a relaxing parafoveal nasal retinotomy after ILM peeling in large or refractory macular holes. Theoretically, this further reduces tangential traction around the hole to facilitate closure. After ILM peeling, endodiathermy is applied to create a small retinotomy at the midpoint between the fovea and optic disc. Slow suction then at the retinotomy site uses a soft-tip cannula. Additional suction at the retinotomy occurs during FAX. The hole diameter narrows as the suction brings the edges together. Either SF6 or C3F8 gas is used. Seven to 10 days of prone positioning is recommended.
Michael S. Tsipursky, MD, reported on a series of 15 eyes.5 Mean basal diameter of the holes was 1,300 μm, and 13 of 15 eyes had refractory macular holes following one or more vitrectomies with ILM peeling.
Macular hole closure was achieved in 13 of 15 eyes (86.7 percent); 11 of 15 (73.3 percent) achieved BCVA improvement during postop follow-up. Mean BCVA improved from 20/400 at baseline to 20/160 at last follow-up.
This is a simple and inexpensive way to close large or refractory macular holes. One disadvantage is that the retinotomy may create a paracentral scotoma, but the authors believe that for most patients the functional vision gains outweigh that risk. RS
Dr. Tsipursky of the University of Illinois, Urbana, has no relevant financial disclosures.
REFERENCES
1. Walter S. Management of proliferative vitreoretinopathy with intravitreal methotrexate using a treat-and-extend protocol. Paper presented at American Society of Retina Specialists 2020 Virtual annual meeting; July 25, 2020.
2. Martel JN, Esposti S, Boulanger-Scemama E, et al. Optogenetics in the clinic: PIONEER, a Phase I/II gene therapy program for non-syndromic retinitis pigmentosa. Poster presented at ASRS 2020 Virtual annual meeting; July 25, 2020.
3. Joshi S, Yadav N, Ayachit AF, Ayachit GS. Multilayered inverted internal limiting membrane flap—a unique technique for closure of large macular holes. Paper presented at ASRS 2020 Virtual annual meeting; July 25, 2020.
4. Lee J, Chua M, Jansen JE, et al. Amniotic membrane subretinal transplantation to promote closure of persistent full-thickness macular holes. Paper presented at ASRS 2020 Virtual annual meeting; July 24, 2020.
5. Tsipursky MS, Byun MJ, Sheth VS, Jager RD. Update on paracentral retinotomy for resistant macular hole. Paper presented at ASRS 2020 Virtual annual meeting; July 25, 2020.



