 |
While we were struggling to cope with the pandemic, the American Medical Association continued to work toward finalizing the revisions to the Evaluation and Management (E/M) codes.
When we learned what the new documentation requirements entailed, most of us were relieved. It was refreshing to see the elimination of history and exam box checking that had been required to meet the E/M documentation rules.
By now, hopefully, you’ve learned how to code an E/M service based on medical decision-making—or, less commonly, time. It was a challenging but not overwhelming task to grasp E/M 2021. Presumably you now have a working understanding of the E/M requirements.
Where we’ve been
Have you figured out what to do with that knowledge? How will you document and code to mitigate fee schedule changes? Do you need to rethink the history and exam you document? Historically, ophthalmologists coded new patient exams with the colloquially named “eye codes” 57 percent of the time, and established patient exams with eye codes nearly 78 percent of the time.1
The reason for this coding pattern was because comprehensive eye (920x4) and intermediate eye (920x2) documentation requirements closely match an ophthalmology exam, and traditionally reimbursement for eye codes has been reasonable.
We (reluctantly) used E/M codes to fill a vital role in ophthalmology despite the advantages of eye codes. In particular, the new patient level 4 (99204) and level 5 (99205) codes have a higher reimbursement and were often appropriate for surgical evaluations and very complex cases. The established patient level 3 (99213) code filled a key role for chronic, stable patient exams.
We know where we’ve been. How have the fee schedule and new documentation guidelines changed recommended coding patterns? To learn the answer, we must first review the 2021 physician fee schedule payment rates.
Where we’re going
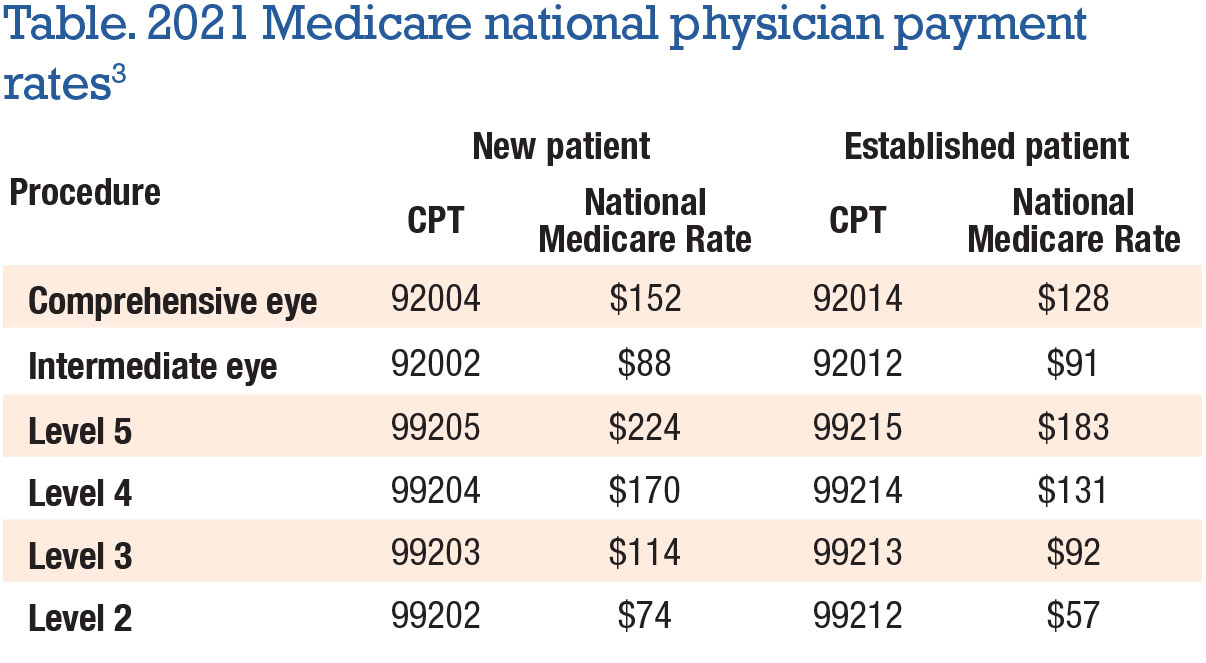
Fortunately, the proposed rates for eye codes, originally slated to suffer significant cuts, were saved from the chopping block. The final national payment rates from the Centers for Medicare and Medicaid Services showed a slight increase for eye codes and some increases for E/M codes (Table).
As you can see from the 2021 rates, payment for new patient exams follows the scale most of us are familiar with: new patient E/M level 4 and 5 (99204 and 99205) pay higher than comprehensive eye (92004). It’s important to also note that E/M new patient level 3 (99203) reimburses higher than new intermediate eye (92002). On the established side, comprehensive eye (92014) reimburses close to E/M level 4 (99214), while E/M level 3 (99213) pays about the same as intermediate eye (92012).
Planning your coding strategy
Having the documentation requirements and reimbursement rates in hand, you can plan your strategy for coding exams. Importantly, the lessened E/M documentation requirements offer an opportunity for you and your technician team to do an exam that’s relevant, clear and concise while eliminating redundant, excessive and otherwise useless but time-consuming documentation from the chart.
 |
Another consideration is that the eye code documentation requirements persist, so you want to be sure your team captures exam elements required for the eye codes when you use them. With simpler documentation requirements for E/M, there may be capacity to add one or two patients per clinic day if you can use the time you save in documentation.
A deeper dive into specific strategies is next. Kevin Corcoran of our firm recently performed an analysis of various coding patterns.2 He looked at four new patient coding scenarios:
- The current national code selection patterns of about 57 percent of new patients coded with eye codes.
- Using eye codes exclusively.
- Using E/M exclusively.
- Shifting to a higher utilization of E/M with the same level of service.
Illustrating the conundrum
 |
Although the outcome of the study indicated the highest revenue benefit from using only E/M codes, that strategy is problematic from a practical standpoint. Some insurance companies prefer eye codes; some E/M exams, especially in retina, won’t meet the criteria for reasonable reimbursement. A few examples help illustrate this conundrum.
• Example 1. A new patient is referred for an eye exam due to longstanding diabetes. A comprehensive exam and optical coherence tomography show the patient has background diabetic retinopathy without macular edema. Treatment includes counseling regarding blood-sugar control. The appropriate E/M code for this exam is 99203; the eye code is 92004.
• Example 2. An established patient comes in for an annual follow-up exam of dry age-related macular degeneration. A comprehensive exam and OCT are performed. Treatment includes counseling and education regarding the signs of conversion to wet AMD as well as instructions to use an Amsler grid daily. The appropriate E/M code will be 99213; the eye code is 92014.
As you can see, abandoning eye codes may result in some missed opportunities. That being said, Mr. Corcoran noted that if an ophthalmologist shifts from the historic utilization of 57 percent eye codes for new patients to a higher utilization of E/M codes (85 percent), the provider will enjoy an increase in annual revenue of about 6 percent.
However, even if no changes are made in coding patterns and a provider continues to utilize eye codes 57 percent of the time for new patients, the provider will see a slight increase in revenue of about 3 percent due to fee schedule adjustments.
Crafting your own strategy
Your own strategy should take into account your ability to document an exam appropriately for the level of service you bill, as well as your overall understanding of the new E/M code requirements. And even if you make no changes in your exam code utilization, you should be sure you’re capturing the required elements for the exams you submit with eye codes.
To assume you can use the E/M documentation rules for exams for which eye codes are used would be a significant problem. As with all aspects of correct coding, understanding the documentation rules will allow you to code confidently and with the most favorable economic outcome. RS
REFERENCES
1. Centers for Medicare & Medicaid Services. Physician and other supplier data CY 2018. https://www.cms.gov/research-statistics-data-systems/medicare-provider-utilization-and-payment-data/medicare-provider-utilization-and-payment-data-physician-and-other-supplier/physician-and-other-supplier-data-cy-2018. Updated December 3, 2020. Accessed March 11, 2021.
2. Corcoran KJ. Economic Impact of 2021 Changes on Eye Exams. Corcoran Consulting Group. 2021.
3. Centers for Medicare & Medicaid Services. Medicare Physician Fee Schedule, National Rates, 2021. https://www.cms.gov/medicare/physician-fee-schedule/search?Y=0&T=4&HT=1&CT=0&H1=92004&H2=92014&H3=92002&H4=92012&M=5. Updated January 20, 2021. Accessed March 11, 2021.



