 |
 |
Rhegmatogenous retinal detachment secondary to giant retinal tear is associated with a relatively high rate of retinal redetachment.1-3 The rate of recurrent retinal detachment secondary to proliferative vitreoretinopathy and/or slippage has been reported to be as high as 40 to 50 percent after the first surgery with small-gauge vitrectomy and long-term gas or silicone oil tamponade.2,3
Proliferative vitreoretinopathy (PVR) has been proposed to be more common with GRTs due to the extent of retinal break, extensive retinal pigment epithelium exposure as well as the younger average age of affected patients. Slippage, which may be due to incomplete drainage of subretinal fluid, occurs when re-attached retina and GRT slip posteriorly, leading to retinal folds or redetachment.
Pioneering PFCL in RRD with GRT repair
Intraoperative use of perfluorocarbon liquid (PFCL), first described in 1987 by Stanley Chang, MD,4 has helped increase intraoperative reattachment in RRD with GRT in the presence or absence of PVR.2 Perfluoro-n-octane (PFO), the most commonly used PFCL today, has a very high specific gravity (1.76), viscosity and low surface tension, which makes it an ideal agent in flattening retinal folds and preventing slippage. Direct intraoperative PFO-silicone oil exchange is one option to mitigate slippage, as we have reviewed here previously (June 2017 Retina Specialist, page 41).
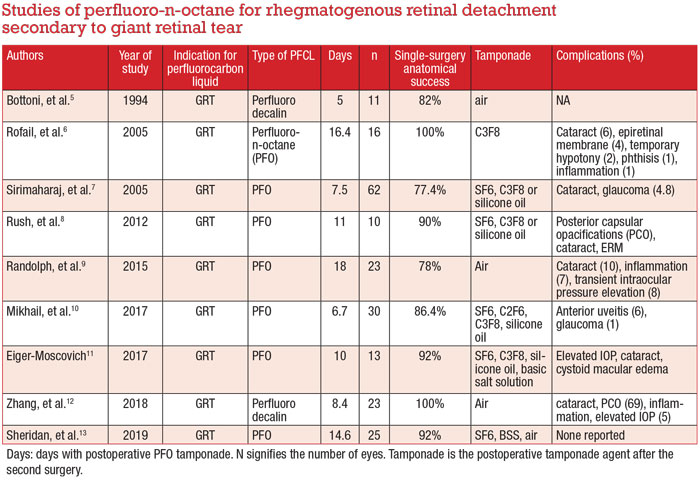
Ferdinando Bottoni, MD, and colleagues at the University of Milan first described the use of PFO as a postoperative tamponade in 1994.5 They demonstrated a
single-surgery anatomical success (SSAS) rate of 82 percent until at least three months of follow-up.
Since then, many authors have retrospectively reported their outcomes with the postoperative use of PFO from an average of five to 18 days (Table, page 11).5-13 The SSAS rate with short- to medium-term postoperative PFO has been reported between 77.4 to 100 percent at three-month follow-up, notwithstanding the immediate second surgery to remove PFO.
 |
Surgical technique
Preservative-free triamcinolone acetate (Triesence, Alcon) is used to visualize the vitreous to ensure a complete PVD and vitrectomy. In GRT, the vitreous base should be meticulously shaved anteriorly 360
degrees with scleral depression. The anterior part of the GRT flap can be trimmed to prevent anterior traction, PVR and possible peripheral ischemia. The video demonstrates these key steps in the technique.
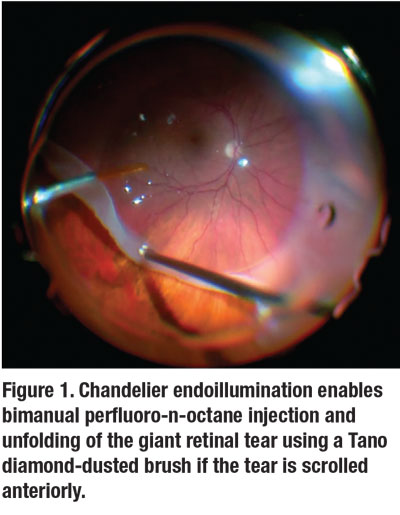
Next, PFO is gradually injected as a single bubble over the optic disc, taking care to ensure the dual bore cannula remains within the bubble as it expands. We sometimes use chandelier endoillumination to allow for bimanual PFO injection and unfolding of the GRT using a Tano diamond-dusted brush if the tear is scrolled at its anterior edge (Figure 1, page 9).
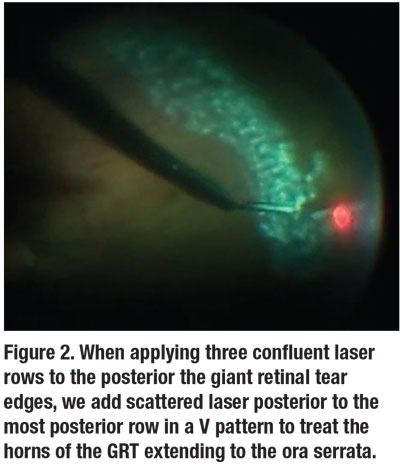
Next, we apply three confluent rows of laser to the posterior edges of the GRT. We like to also add scattered laser posterior to the most posterior row in a V pattern to treat the horns of the GRT extending to the ora serrata (Figure 2). Doing so prevents guttering of subretinal fluid and recurrent RRD. We often also add two rows of laser 360 degrees close to the ora serrata.
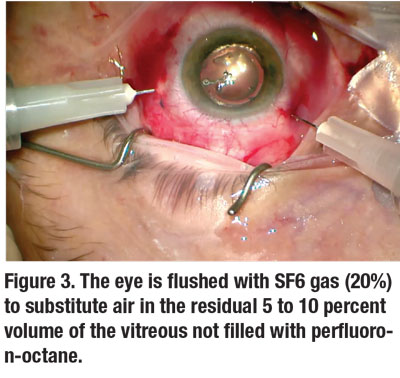
Following this, the eye is topped off with a full fill of PFO (usually around 90 percent) until it reaches the trocars. Any residual vitreous fluid that remains behind the lens is exchanged for air in a minimal fluid-air exchange.
The eye is then flushed with SF6 gas (20%) to substitute air in the residual 5 to 10 percent volume of the vitreous not filled with PFO (Figure 3). We routinely close the sclerotomies with sutures to prevent any subconjunctival migration of PFO that would result in an underfill.
 |
Postoperative management
We instruct the patient to lie supine 90 percent of the time postoperatively. Approximately seven to 10 days later, we take the patient back to the operating room to remove the PFO. Using a soft-tipped cannula, a fluid-air exchange is performed, with meticulous removal of any and all PFO bubbles in the posterior pole.
If the patient is pseudophakic, an anterior chamber washout may also be required to ensure no PFO bubbles remain in the anterior segment.
Next, we perform scleral depression to release any PFO bubble from the pars plana. This is a very important step as PFO bubbles may easily get trapped in the pars plana/plicata, much as emulsified silicone oil particles do. A fluid-air exchange is then completed with 100 percent air fill. The eye is then flushed with gas, either SF6 or C3F8.
 |
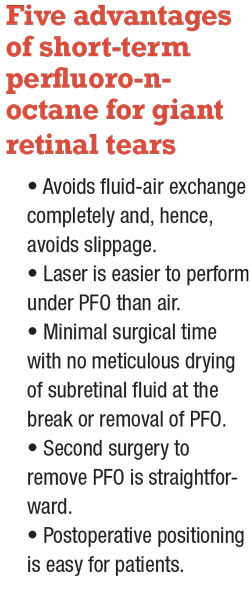 |
The PFO advantage
Using PFO as a short-term tamponade for GRT has huge advantages. The most difficult step of GRT surgery is avoiding slippage, which occurs during removal of PFO in the fluid-air exchange.
Injecting PFO, lasering under the PFO and closing the eye completely avoids this most difficult step of FAX since there’s no removal of PFO. Consequently, there’s no chance of slippage.
Moreover, laser can be applied to the GRT under very good visualization with PFO in situ. Surgical time is also minimized by removing the riskiest and time-consuming step of PFO removal, including the meticulous drying of the edge of the break to ensure no subretinal fluid or PFO
remains at the end of the case.
Even a direct PFO-silicone oil exchange still carries an opportunity for slippage because removal of PFO can result in some change in the position of the GRT and subsequent slippage. A short-term PFO tamponade avoids this risk completely and is our preferred technique.
Postoperative positioning is also quite easy for patients because they’re often more compliant positioning supine rather than staying face-down or on their side.
 |
The second operation
For the second operation, around seven to 10 days after insertion of PFO, its removal is quite straightforward aside from needing to take time to find all the small bubbles that continue to emerge. We find using a high-magnification contact lens and a soft-tipped backflush cannula to passively remove these bubbles from the macular surface helps keep the process relatively straightforward.
In our experience, postoperative inflammation is minimal during the seven-day period with PFO in situ. We have, however, noticed that phakic patients often have some worsening of cataract within the seven days, so it’s probably a good idea to consider cataract removal during the second surgery of PFO removal or soon afterward. All phakic patients in our series opted to undergo cataract extraction and intraocular lens implantation at the time of the second operation to remove the PFO.
Duration of postoperative PFO
In a literature review,5–13 postoperative PFO was removed on average at day 10.84. Most authors compared the advantage of longer-term tamponade with the possibility of PFO retinal toxicity in the form of outer plexiform changes, retinal compression, and cited complications such as elevated IOP and inflammation.
The rationale for keeping PFO for a minimum of six to seven days is that’s how long it takes to achieve the complete effect with laser retinopexy.
In our experience, an average of seven days with PFO was adequate to achieve long-term anatomical success. SSAS was 100 percent at three months’ follow-up in our series, a rate comparable to other small case-series of short-term postop PFO with RRD secondary to GRT with a similar follow-up length.6,11–13
 |
Choice of long-term tamponade after PFO removal
We opted to use long-acting gas (C3F8) in all of our cases based on previous reports of slightly worse outcomes after PFO removal with SF-6.6-8,10,11 Nevertheless, short term tamponade with, air, balanced salt solution or short-term gas (SF6) has been done routinely after short- to medium-
term PFO removal with comparable
anatomical success rates.7,8,10-13
We didn’t deem silicone oil necessary as all patients remained attached under PFO and for up to three months following PFO removal with long-term gas. As well, none of our cases were complicated by residual or recurrent PVR following PFO removal.
Bottom line
PFO as a short-term postoperative tamponade agent in management of RRD secondary to GRT is safe and effective. The anatomical success rates with postop PFO (short to medium-term) are excellent. In our series the success rate was 100 percent, which is favorable compared to the reported success rates of 60 to 75 percent with gas or oil.
Phakic patients are candidates for early cataract surgery, perhaps at the time of PFO removal. Following PFO removal, long-term gas provides excellent tamponade and long-term anatomical success. RS
Watch as Drs. Arjmand and Mandelcorn demonstrate their technique for using a perfluoro-n-octane short-term tamponade for repair of a rhegmatogeous retinal detachment with a giant retinal tear.
REFERENCES
1. Kertes PJ, Wafapoor H, Peyman GA, Calixto N, Thompson H. The management of giant retinal tears using perfluoroperhydrophenanthrene. A multicenter case series. Vitreon Collaborative Study Group. Ophthalmology. 1997;104:1159-1165.
2. Scott IU, Murray TG, Flynn HW, and the Perfluoron Study Group, et al. Outcomes and complications associated with giant retinal tear management using perfluoro-n-octane. Ophthalmology 2002;109:1828–1833
3. Barthelmes D, Chandra J. Perfluoro-n-octane as a temporary intraocular tamponade in a staged approach to manage complex retinal detachments. Clin Ophthalmol. 2015;9:413-418.
4. Chang S. Low viscosity liquid fluorochemicals in vitreous surgery. Am J Ophthalmol. 1987;103:38–43
5. Bottoni F, Bailo G, Arpa P, Prussiani A, Monticelli M, de Molfetta V. Management of giant retinal tears using perfluorodecalin as a postoperative short-term vitreoretinal tamponade: A long-term follow-up study. Ophthalmic Surg. 1994;25:365–373.
6. Rofail M, Lee LR. Perfluoro-n-octane as a postoperative vitreoretinal tamponade in the management of giant retinal tears. Retina. 2005;25:897-901.
7. Sirimaharaj M, Balachandran C, Chan WC, et al. Vitrectomy with short term postoperative tamponade using perfluorocarbon liquid for giant retinal tears. Br J Ophthalmol 2005;89:1176–1179.
8. Rush R, Sheth S, Surka S, Ho I, Gregory-roberts J. Postoperative perfluoro-N-octane tamponade for primary retinal detachment repair. Retina. 2012;32:1114-1120.
9. Randolph JC, Diaz RI, Sigler EJ, Calzada JI, Charles S. 25-gauge pars plana vitrectomy with medium-term postoperative perfluoro-n-octane for the repair of giant retinal tears. Graefes Arch Clin Exp Ophthalmol. 2016;254:253-257.
10. Mikhail MA, Mangioris G, Best RM, Mcgimpsey S, Chan WC. Management of giant retinal tears with vitrectomy and perfluorocarbon liquid postoperatively as a short-term tamponade. Eye (Lond). 2017;31:1290-1295.
11. Eiger-Moscovich M, Gershoni A, Axer-Siegel R, Weinberger D, Ehrlich R. Short-term vitreoretinal tamponade with heavy liquid following surgery for giant retinal tear. Curr Eye Res. 2017;42:1074–1078
12. Zhang Z, Wei Y, Jiang X, Zhang S. Surgical outcomes of 27-gauge pars plana vitrectomy with short-term postoperative tamponade of perfluorocarbon liquid for repair of giant retinal tears. Int Ophthalmol. 2018;38:1505-1513.
13. Sheridan AM, Essex RW, Yeoh J, Allen P, Campbell WG, Edwards TL. Is post-operative perfluorocarbon liquid tamponade for macula-on giant retinal tear safer than silicone oil? Eye (Lond). 2019;33:689-691.
14. Yu Q, Liu K, Su L, Xia X, Xu X. Perfluorocarbon liquid: Its application in vitreoretinal surgery and related ocular inflammation. Biomed Res Int. 2014;2014:250323.




