He noticed the scotoma just nasal to fixation in the right eye starting about one hour after the eclipse. He noted no progressive enlargement of the scotoma or new scotomas in the subsequent days and found that the “blind spot” had grown less noticeable over time. His ocular history was unremarkable.
Examination Findings
Best-corrected visual acuity was 20/20 in both eyes and intraocular pressures were normal. No afferent pupillary defect was detected. Visual fields were full upon confrontation bilaterally. However, on Amsler grid testing he localized a small area of metamorphopsia just nasal to fixation in the right eye.
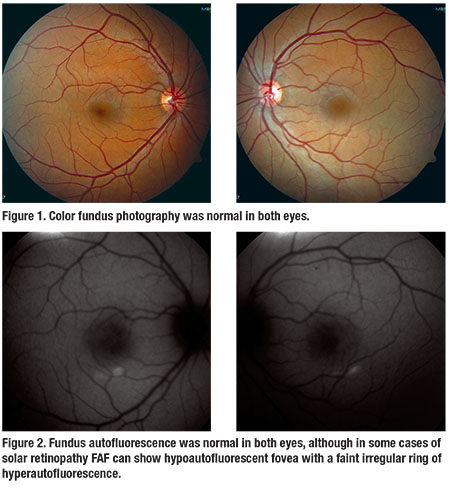
The anterior segment exam was normal in both eyes. Fundus examination was unremarkable in both eyes with no corresponding macular findings in the right eye to explain his symptoms (Figure 1).
Workup
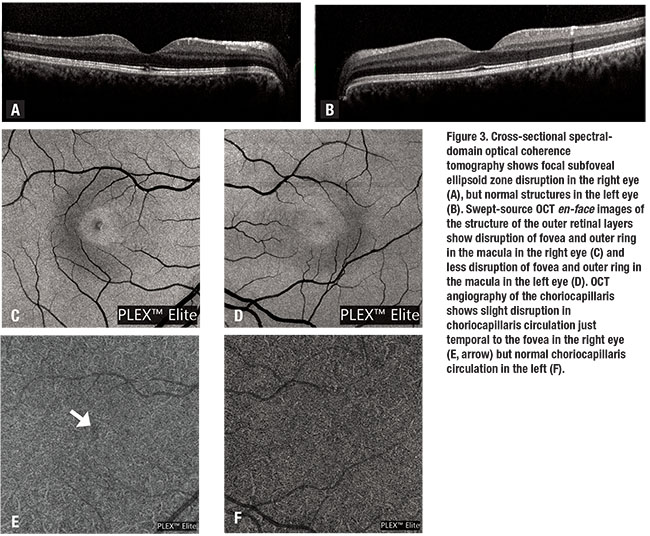
Fundus autofluorescence (FAF) was normal in both eyes (Figure 2). Spectral-domain optical coherence tomography (SD-OCT) of the right eye showed normal foveal contour with a focal area of subfoveal ellipsoid zone loss measuring approximately 150 µm (Figure 3A). SD-OCT of the left eye was normal (Figure 3B). The RPE was intact in both eyes.
Swept-source OCT en-face images of the outer retinal layers showed disruption of the fovea and an outer perifoveolar ring of disruption in the right eye (Figure 3C), and less-prominent disruption of the perifoveolar macula in the left eye (Figure 3D).
SS-OCT angiography of the right eye showed focal irregularity of the choriocapillaris circulation corresponding with the areas of overlying outer retinal loss (Figure 3E). SS-OCT-A of the left eye showed normal choriocapillaris circulation that appeared asymmetric compared to the affected right eye (Figure 3F).
Diagnosis and Management
Based on this patient’s history of viewing the eclipse without eye protection and the focal subfoveal ellipsoid zone loss, our diagnosis was solar retinopathy. No evidence-based therapy is available for treatment of solar retinopathy, but we advised the patient to start on AREDS2 vitamins and arranged for follow-up in one month.
Discussion
Solar retinopathy is retinal insult caused by
 |
Symptoms typically include blurred vision with a central or paracentral scotoma, sometimes with chromotopsia, metamorphopsia, photophobia and headache. Typically both eyes are affected, but the condition can be asymmetric. Visual acuity at presentation typically ranges from 20/20 to 20/60, but has been reported to be as poor as 20/200.2 As little as one-minute fixation on the sun can cause solar retinopathy, though increased intensity and duration of exposure can lead to more severe pathology.3
The cornea, anterior chamber, and adult lens absorb light in the visible spectrum, UV-C, UV-B and part of the UV-A spectrum. However, certain wavelengths of visible and UV light still pass through to the retina, causing the generation of reactive oxygen species, resulting in oxidative damage to retinal pigment epithelium cells and surrounding photoreceptors. Lipofuscin in the RPE is highly photoreactive, and shorter wavelength light causes induction of reactive oxygen species in lipofuscin that in turn causes subsequent damage to the RPE.3 With injury to the supportive RPE layer, photoreceptor segments may also undergo secondary damage.
Fundus examination may appear normal; however, classically described changes include a yellowish-white foveal spot with surrounding dark granular pigmentation occurring one to three days post-injury.3 This can evolve into a well-circumscribed red spot after 10 to 14 days. Transient macular edema can also occur. In the chronic phase, the macular lesion may take on a yellowish color with irregular borders of RPE mottling.4
The most sensitive diagnostic imaging technique is OCT, which typically exhibits reduced reflectivity from the RPE with disruption of the inner and outer photoreceptor segments.3,4 OCT structural changes are not consistent among cases, but acute changes predominantly include disruption of the RPE and outer photoreceptor segments.2 Acute changes may resolve, but patients with chronic vision loss often have OCT findings of inner and outer photoreceptor segment damage, demonstrating permanent disruption of photoreceptors.2
FAF can show a hypoautofluorescent fovea with a faint irregular ring of hyperautofluorescence.5 Hypoautofluorescence is due to a deficiency of lipofuscin from loss of RPE and photoreceptors. Fluorescein angiography may show punctate window defects or parafoveal leaks correlating with damage to the RPE and photoreceptors, but is frequently within normal limits.4,6 OCT angiography can detect subtle microvascular abnormalities and provide extensive detail of retinal vasculature. There is no published work regarding OCT-A in patients with solar retinopathy, but it may be helpful in future studies of this disease.3
Decreased visual acuity in solar retinopathy is often self-resolving, and prognosis is correlated with initial visual acuity and photoreceptor damage on OCT.3,7 A study from Nepal found that more than 80 percent of 319 patients with solar retinopathy had final visual acuity of 20/40 or better.8 In a case series of 36 patients with solar retinopathy from a 1995 solar eclipse in Pakistan, 72 percent of patients had full recovery of vision and another 19 percent had partial recovery, with maximum recovery occurring between two weeks and six months.9
Another case series showed most patients recovered vision within two to four weeks, and pre-exposure acuity of 20/50 or better had earlier and more favorable visual recovery.10 However, there are patients from all of these studies that experienced persistent central or paracentral scotomas,8-10 and patients experienced no further improvement in visual acuity after six to 18 months.9,10
 |
No evidence-based treatment of solar retinopathy is available. Steroids have been proposed as treatment for acute solar retinopathy because of their anti-inflammatory effects and for treatment of associated macular edema. However, the macular edema associated with solar retinopathy has been shown to improve on its own and prognosis is variable with steroid administration. The use of steroids also places the patient at risk for other complications, such as cataract formation, intraocular pressure elevation or central serous chorioretinopathy.3
Because the mechanism of damage in solar retinopathy is thought to be free radicals, antioxidants have also been proposed to protect against UV damage from solar retinopathy. In the Age Related Eye Disease Study, antioxidant vitamins were shown to reduce the risk of progression of age-related macular degeneration,11 but there is no certainty regarding whether administration of antioxidants after UV exposure could aid visual recovery in cases of solar retinopathy.
Because no proven therapies for solar retinopathy exist, the retina specialist has a responsibility to participate in preventative care and patient education. Community outreach at times of significant events such as a solar eclipse is important in educating patients regarding safe viewing practices. RS
References
1. Mainster MA, Turner PL. Ultraviolet-B phototoxicity and hypothetical photomelanomagenesis: Intraocular and crystalline lens photoprotection. Am J Ophthalmol. 2010;149:543-549.
2. Chen KC, Jung JJ, Aizman A. High definition spectral domain optical coherence tomography findings in three patients with solar retinopathy and review of the literature. Open Ophthalmol J. 2012;6:29. https://www-ncbi-nlm-nih-gov.offcampus.lib.washington.edu/pmc/articles/PMC3394112/. Accessed September 28, 2017.
3. Begaj T, Schaal S. Sunlight and ultraviolet radiation-pertinent retinal implications and current management. Surv Ophthalmol. 2017 September 18. Epub ahead of print.
4. Jain A, Desai RU, Charalel RA, Quiram P, Yannuzzi L, Sarraf D. Solar retinopathy: Comparison of optical coherence tomography (OCT) and fluorescein angiography (FA). Retina. 2009;29:1340-1345.
5. Bruè C, Mariotti C, Franco ED, Fisher Y, Guidotti JM, Giovannini A. Solar retinopathy: A multimodal analysis. Case Rep Ophthalmol Med. 2013;2013:906920 Epub 2013 February 12.
6. Dhir SP, Gupta A, Jain IS. Eclipse retinopathy. Br J Ophthalmol. 1981;65:42-45.
7. Klemencic S, McMahon J, Upadhyay S, Messner L. Spectral domain optical coherence tomography as a predictor of visual function in chronic solar maculopathy. Optom Vis Sci. 2011;88:1014-1019.
8. Rai N, Thuladar L, Brandt F, Arden GB, Berninger TA. Solar retinopathy. A study from Nepal and from Germany. Doc Ophthalmol. 1998;95:99-108.
9. Awan AA, Khan T, Mohammad S, Arif AS. Eclipse retinopathy: Follow up of 36 cases after April 1995 solar eclipse in Pakistan. J Ayub Med Coll Abbottabad. 2002;14:8-10.
10. MacFaul PA. Visual prognosis after solar retinopathy. Br J Ophthalmol. 1969;53:534-541.
11. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: The Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA. 2013;309:2005-2015.



