 |
|
Have a question for “Coding Commentary”? Tweet it to us at | |
|
Bio |
By now you should be comfortable with the new Evaluation and Management (E/M) coding rules. If you’re using the E/M codes correctly, your revenue compared to previous years should be about level. (Of course, if it is level, that means your effective revenue has declined.)
A savvy retina specialist will perform, document and bill all services performed on a given date of service. For example, a commonly missed charge is extended ophthalmoscopy. As a vitreoretinal specialist, a part of your stock in trade is doing EO. Let’s look at what you need to do and document in order to bill for this service that you perform regularly.
In previous versions of CPT, EO was billed as “initial” or “subsequent.” Importantly, in January last year the CPT for EO was overhauled to allow charges for a macular/optic nerve exam or a peripheral retinal exam. The initial or subsequent definition was dropped entirely.
Macular exam
CPT defines the macular exam as: “Ophthalmoscopy, extended, with drawing of optic nerve or macula (e.g., for glaucoma, macular pathology, tumor) with interpretation and report, unilateral or bilateral.” The CPT code is 92202. There’s no defined limitation of services for this code.
However, payment is only appropriate if there’s serious disease and a documented change in appearance to support the charge. Your documentation should, of course, include an exam note that supports the macular EO.
You must have a scaled, labeled, separate drawing above and beyond your usual macular documentation. Payers differ on the required size of the drawing and whether the drawing should be in color, so check your local payer policies to be sure you meet any specific size and color requirements. Those payers that have policies usually specify that drawings be 3 to 4 inches or larger; in any case, they must be large enough to show significant detail.
Peripheral retinal exam
 |
|
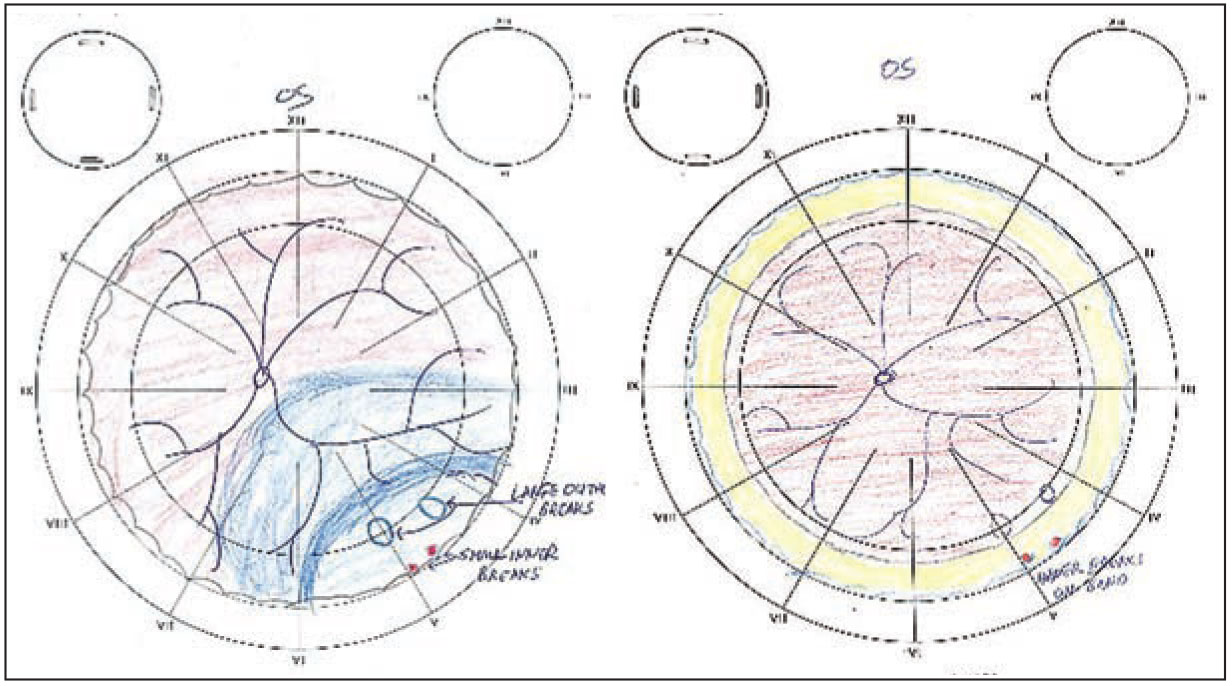
Scaled, labeled drawings such as these, depicting retinal detachment secondary to retinoschisis detachment in the left eye, are key components of the documentation for extended ophthalmoscopy. (Courtesy William H. Ross, MD, FRCSC) |
The definition for the peripheral retinal exam is more specific: “Ophthalmoscopy, extended, with retinal drawing and scleral depression of peripheral retinal disease (e.g., for retinal tear, retinal detachment, retinal tumor) with interpretation and report, unilateral or bilateral” [emphasis added]. The CPT code for this service is 92201. As with macular EO, there’s no defined limitation, but again, payment is appropriate only if the disease has changed in appearance. The specifications are also more clearly defined:
- Retinal drawings must be maintained in the patient’s record.
- Drawings should include sufficient detail, standard colors and appropriate labels.
- Individual drawings should be made for each eye.
- The drawing must be separate and distinct from the comprehensive eye exam.
- An assessment of the change from prior exams when performing follow-up services is required.
Payer requirements vary, and they may also include scaling the drawing to depict relative size, coloring it using classical representations (that is, red for hemorrhage, blue for detachment, etc.), and notating that the eye was dilated and the dilating agent used. Again, review your Medicare carrier policies for specific requirements.
Documentation requirements
 |
For either code, the documentation must be legible. It’s important that you indicate the type of exam performed, such as whether it was done with a 90-D lens with the slit lamp (for 92202), or with a 20-D lens with the patient supine and that scleral depression was performed (for 92201). Also, the documentation should note whether any anesthesia was needed and, although rare, if any complications were encountered or if the test was uncomplicated.
An important point to reiterate is that this charge is appropriate when you’re performing the test to document serious retinal pathology. You shouldn’t bill either EO charge when the exam is normal.
Many electronic medical records systems allow you to “carry forward” a macula or peripheral drawing. However, you must avoid duplicative documentation, and only bill for EO when you’ve created a new and clearly unique drawing.
The 2021 national Medicare payment rate for macular EO is $25.12; the peripheral EO rate is $16.05. Commercial payments may be higher. And before you discount the value of billing a properly documented EO, consider how often you currently perform this service without billing for your time and expertise.
A word about bundling EO
In a previous article we discussed national correct coding initiative (NCCI) edits, colloquially called “bundles,” which impact ophthalmology services. These bundles will result in claim denial when disallowed services are billed on the same date of service.
Like many ophthalmic tests, EO has edits that you should keep in mind. First and foremost, EO is bundled with fundus photography (92250). However, EO isn’t bundled with fluorescein angiography or scanning computerized ophthalmic diagnostic imaging (SCODI), but carriers specify that EO performed on the same date of service as FA or SCODI should provide information that the other tests didn’t.
EO is also bundled with all retinal surgeries. However, some insurance carriers will deny payment for EO during the postoperative period of a retinal procedure. Again, check your local Medicare policies to avoid billing statutorily denied charges.
EO is a valuable and often-performed procedure in the retinal clinic. When it’s warranted and you do it, you should bill for it. RS
REFERENCES
1. 92201, 92202 Extended Ophthalmoscopy. CPT Professional 2020. 1st ed. Chicago, IL: American Medical Association; 2019.
2. Centers for Medicare and Medicaid Services. Medicare Physician Fee Schedule Look Up Tool. Updated July 1, 2021. Available at: https://www.cms.gov/medicare/physician-fee-schedule/search?Y=0&T=4&HT=1&CT=0&H1=92201&H2=92202&M=5




