Take-home Points
|
 |
|
Bio Dr. Cunningham is also a vitreoretinal surgeon and partner as well as research director at Florida Retina Institute. DISCLOSURES: Dr. Kumar disclosed being a consultant for Alimera Sciences. Dr. Cunningham disclosed acting as a consultant for Alimera, Allergan/AbbVie and Novartis. |
While vitreous opacities in some patients can be a mere nuisance, in others they can be visually significant and interfere with daily activities. The traditional teaching has been to simply educate patients that vitreous floaters are a benign condition with no long-term sequelae and observe them.
However, we’ve all had patients whose symptoms significantly impair their quality of life. As vitreoretinal surgeons, we need to be prepared to discuss treatment options with symptomatic patients. In this article, we review various exam and imaging tools that can help with the assessment of VO and educating patients about their clinical findings.
Exam findings of consequence
While examining a patient at the slit lamp, there are several findings to pay particular attention to. They include lenticular status, presence of a Weiss ring, absence of vitreous cells and peripheral retinal findings such as retinal tears or lattice degeneration.
If a patient hasn’t had cataract surgery, the vitreous just posterior to the lens can’t be completely removed during the operation, which could lead to incomplete resolution of the patient’s symptoms. Inducing a posterior vitreous detachment, if a Weiss ring isn’t present on exam, can lead to an increased risk of iatrogenic breaks during surgery.
Conversely, if no Weiss ring is present on exam and the hyaloid isn’t separated during surgery, patients may become symptomatic in the future when the PVD naturally occurs.
Finally, it’s critical to rule out mimickers such as ocular amyloidosis, lymphoma and uveitic conditions such as birdshot chorioretinopathy.
Role of multimodal imaging
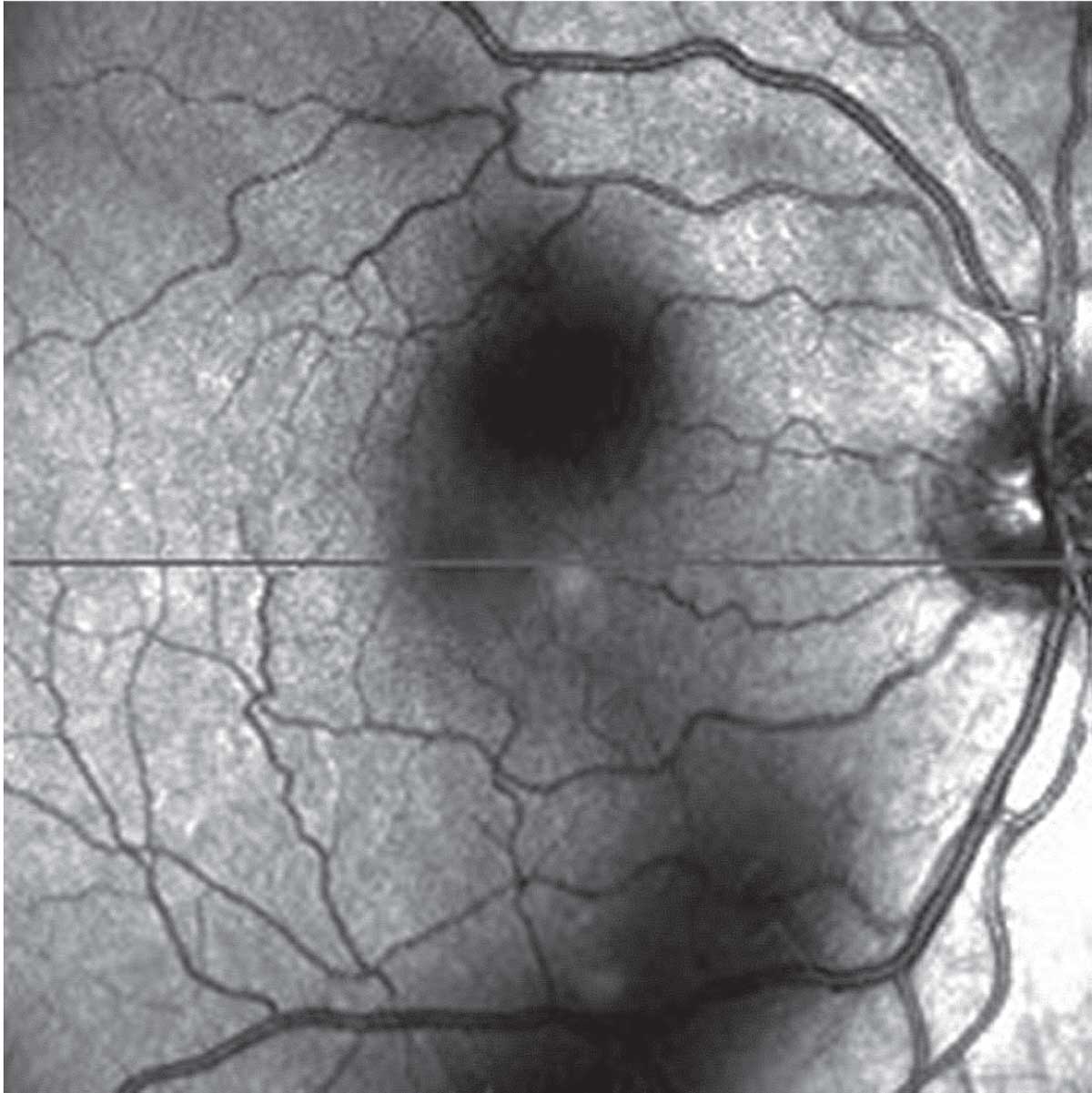 |
| Scanning laser ophthalmoscopy demonstrates vision-disturbing vitreous opacities. (Source: Huang L, et al. Vitreous floaters and vision: Current concepts and management paradigms. In Sebag J, ed. Vitreous – in Health & Disease. New York, NY; Springer; 2014:771-788. Used with permission) |
Multimodal imaging is a helpful tool for the clinical assessment of VOs. Several imaging tests can aid in our evaluation of the vitreous and help to educate the patient about how their symptoms correlate with their anatomical findings.
The first test is scanning laser ophthalmoscopy imaging on optical coherence tomography to assess the shadowing of the vitreous (Figure). On the main OCT image, the hyaloid face separation from (or adherence to) the retina can be visualized.
Widefield fundus photography and
autofluorescence can help to educate the patient about the anatomy of the vitreous and retina, and to highlight any peripheral pathology. Although it’s not used routinely in our clinical practice, ultrasound can also be helpful to quantify vitreous opacities and correlate them with disease severity.1
Current treatment options for VO
Typically, when facing a patient with symptomatic VO, the management options include observation, YAG-laser vitreolysis and pars plana vitrectomy. YAG-laser vitreolysis has gained popularity for addressing visually significant floaters, because it’s a relatively fast and non-invasive procedure.
The first report of YAG laser vitreolysis for floaters was published in 1993.2 However, various reports since then have questioned the safety of YAG laser vitreolysis, with sequelae that range from refractory glaucoma to posterior capsule rupture and rapid cataract progression after the procedure.3-6
Because of the potential complications associated with YAG laser vitreolysis, the American Society of Retina Specialists Research and Safety in Therapeutics (ReST) committee recommended further investigation.7
In addition to the potential safety issues, another downside of YAG vitreolysis is that the VOs don’t actually go away. The laser may displace the large floater from the central vision, but patients often have persistent symptoms. Vitrectomy surgery is the only procedure that eliminates the opacities.
 |
PPV safety profile improves
PPV for visually significant floaters was initially reported more than 20 years ago.8 In the past 20 years, however, the safety profile of small-gauge vitrectomy has improved dramatically. Many studies have shown reduced complications with 23- and 25-gauge PPV compared to 20-gauge vitrectomy, including fewer cases of vitreous incarceration at the sclerotomy site, fewer iatrogenic breaks, and less dialysis at the vitreous base.9-14
Moreover, smaller probes allow for more precise and controlled surgical movements, resulting in safer removal of the vitreous and less traction on the retina. From a patient comfort perspective, the transconjunctival sutureless approach leads to less discomfort and ocular inflammation.
Despite the improved safety profile, vitreoretinal surgeons still remain hesitant to perform vitrectomies for VO. A 2015 survey assessing the management of symptomatic floaters found that only 25 percent of vitreoretinal surgeons would perform vitrectomy to address symptomatic floaters.15 So the question is: Should we be more open to considering PPV for symptomatic VO?
A qualified yes for PPV
The short answer is yes—in the correct patient. The majority of patients who present with an acute PVD describe bothersome floaters or photopsias. Symptoms in most patients will improve with time, typically in three to six months, and will be tolerable. However, a small percentage of patients may have significant VOs that impair their quality of life and ability to work. In these symptomatic patients with specific exam criteria, it’s not unreasonable to discuss PPV for VO.
 |
A detailed discussion with these patients about expectations and the risks and benefits of PPV is essential. An important intraoperative complication to discuss is the potential for intraoperative retinal breaks. In most series, the reported rates of intraoperative or iatrogenic breaks are less than 5 percent.16 Other important potential postoperative complications to include in the discussion with the patient include hypotony, vitreous hemorrhage (7 to 9 percent), macular edema (10 percent) and retinal detachment (0 to 17 percent).16
Criteria for PPV for VO
So, what are the specific criteria that we consider when signing a patient up for PPV for VO?
Our group evaluated the safety profile and surgical outcomes of PPV for VO in our retina-only private practice over a four-year period. A total of 104 eyes of 81 patients underwent either 23- or 25-gauge vitrectomy. All patients were required to be pseudophakic, symptomatic for more than six months, and have a Weiss ring present on exam.
Mean preoperative VA of 0.16 ±0.17 logMar units (~20/29 SE) improved to 0.12 ± 0.15 logMar units (~20/26 SE, Wilcoxon test, p=0.0083) at the last known follow-up after PPV. There were no cases of retinal tears or retinal detachments in our series. One patient developed a vitreous hemorrhage that spontaneously resolved.
We’ve had excellent surgical outcomes and believe the key was patient selection that met the three aforementioned criteria. Subjectively, patients were overall satisfied with the surgical outcome. Although we didn’t perform a preoperative or postoperative VFQ-25 survey for our patients, 43 percent of them elected to have surgery in the fellow eye.17
For the patient without PVD
In our discussion with a patient who hasn’t yet had cataract surgery or doesn’t yet have a PVD, we find it important to counsel them about the safety of performing PPV for floaters in the ideal setting. For example, in patients without a PVD, the risk of an intraoperative retinal tear increases by a factor of almost five. The risk of retinal tears reported with induction of a PVD for PPV, whether for floaters, macular hole or epiretinal membrane, is approximately 5 percent compared with 1 percent without induction of a PVD.16-20 We find it important to tell patients about these risks.
In phakic patients, the surgeon isn’t able to clear some of the most visually disturbing floaters located just posterior to the lens. Therefore, the patient’s symptoms could persist after surgery.
Despite having cutting-edge technology and imaging platforms to enhance visualization of the vitreoretinal interface, we still lack objective data to quantify VO. Current objective data is limited to visual acuity alone, and most retina surgeons are reluctant to operate on an eye with a visual acuity of 20/20.
 |
We need better, readily available metrics that evaluate contrast sensitivity and even quality of life measures. Some have proposed a VO severity grading scale that could provide additional objective data to retina surgeons and also serve as a helpful VO monitoring tool for referring doctors.
Bottom line
Vitreoretinal surgery has traditionally been viewed as anatomically repairing defects in the retina of symptomatic patients. With improved safety profiles of small-gauge vitrectomy and excellent patient outcomes, it’s time to accept and expand the scope of vitreoretinal surgery to include PPV for VO.
Cataract surgery is routinely performed on patients with objectively “good vision,” because subjectively functional vision loss can affect their quality of life. Patients with VO may similarly have a functional loss of vision with difficulty driving, reading or working. We really don’t think twice about a symptomatic patient undergoing a cataract evaluation. Similarly, we shouldn’t have to think twice about discussing surgery as an option for a patient with visually significant floaters that are impacting their functionality.
We must stress that although PPV for VO is generally a safe and effective procedure, complications may still occur, as they may with any surgical intervention. For that reason, we advise careful consideration of patient selection and a detailed informed consent process. RS
REFERENCES
1. Mamou J, Wa CA, Yee KMP, et al. Ultrasound-based quantification of vitreous floaters correlates with contrast sensitivity and quality of life. Invest Ophthalmol Vis Sci. 2015;56:1611-1617.
2. Tsai WF, Chen YC, Su CY. Treatment of vitreous floaters with neodymium YAG laser. Br J Ophthalmol. 1993;77:485–488.
3. Huang K-H, Weng T-H, Chen Y-J, Chang Y-H. Iatrogenic posterior lens capsule rupture and subsequent complications due to Nd:YAG laser vitreolysis for vitreous floaters: A case report. Ophthalmic Surg Lasers Imaging Retina. 2018;49:e214–e217.
4. Cowan LA, Khine KT, Chopra V, Fazio DT, Francis BA. Refractory open-angle glaucoma after neodymium-yttrium-aluminum-garnet laser lysis of vitreous floaters. Am J Ophthalmol. 2015;159:138–143.
5. Koo EH, Haddock LJ, Bhardwaj N, Fortun JA. Cataracts induced by neodymium-yttrium-aluminum-garnet laser lysis of vitreous floaters. Br J Ophthalmol. 2017;101:709–711.
6. Sun I-T, Lee T-H, Chen C-H. Rapid cataract progression after Nd:YAG vitreolysis for vitreous floaters: A case report and literature review. Case Rep Ophthalmol. 2017;8:321–325.
7. Hahn P, Schneider EW, Tabandeh H, Wong RW, Emerson GG, American Society of Retina Specialists Research and Safety in Therapeutics (ASRS ReST) Committee. Reported complications following laser vitreolysis. JAMA Ophthalmol. 2017;135:973–976.
8. Schiff WM, Chang S, Mandava N, Barile GR. Pars plana vitrectomy for persistent, visually significant vitreous opacities. Retina. 2000; 20:591-596.
9. Chung SE, Kim KH, Kang SW. Retinal breaks associated with the induction of posterior vitreous detachment. Am J Ophthalmol. 2009;147:1012-1016.
10. Wa C, Sebag J. Safety of vitrectomy for floaters. Am J Ophthalmol. 2011;152:1077.
11. Lakhanpal RR, Humayun MS, de Juan E Jr, et al. Outcomes of 140 consecutive cases of 25-gauge transconjunctival surgery for posterior disease. Ophthalmology. 2005;112:817-824.
12. Ibarra MS, Hermel M, Prenner JL, Hassan TS. Long term outcomes of transconjunctival sutureless 25-gauge vitrectomy. Am J Ophthalmol. 2005;139:831-836.
13. Fine HF, Iranmanesh R, Iturralde D, Spaide RF. Outcomes of 77 consecutive cases of 23-gauge transconjunctival vitrectomy surgery for posterior segment disease. Ophthalmology. 2007;114:1197-1200.
14. Fujii GY, de Juan E Jr, Humayun MS, et al. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology. 2002;109:1807-1812; discussion 1813. Erratum in: Ophthalmology. 2003;110:9.
15. Cohen MN, Rahimy E, Ho AC, Garg SJ. Management of symptomatic floaters: Current attitudes, beliefs, and practices among vitreoretinal surgeons. Ophthalmic Surg Lasers Imaging Retina. 2015;46:859-865.
16. Recchia FM, Scott IU, Brown GC, Brown MM, Ho AC, Ip MS. Small-gauge pars plana vitrectomy: A report by the American Academy of Ophthalmology. Ophthalmology. 2010;117:1851-1857.
17. Fink S, Kumar JB, Cunningham MA. Small-gauge pars plana vitrectomy for visually significant vitreous floaters. J VitRet Dis. 2020;5:247-250.
18. Chung SE, Kim KH, Kang SW. Retinal breaks associated with the induction of posterior vitreous detachment. Am J Ophthalmol. 2009;147:1012-1016.
19. Sebag J, Yee KMP, Wa CA, Huang LC, Sadun AA. Vitrectomy for floaters: Prospective efficacy analyses and retrospective safety profile. Retina. 2014;34:1062-1068.
20.Mason JO 3rd, Neimkin MG, Mason JO 4th, et al. Safety, efficacy, and quality of life following sutureless vitrectomy for symptomatic vitreous floaters. Retina. 2014;34:1055-1061.



