Take-home Points
|
 |
|
Bios Dr. Seddon is a professor of ophthalmology and visual sciences, director of retina and director of the Macular Degeneration Center of Excellence at the University of Massachusetts Medical School, Worcester. Disclosures: Dr. Seddon |
It’s been well established that a number of factors play a role in progression from non-advanced to advanced age-related macular degeneration.1 These factors include, but are not limited to, age, smoking history,2 diet and nutrition,3-5 environmental influences and a number of genetic variants.6-11 However, little research has been done to investigate factors associated with drusen size progression, even though drusen in early and intermediate AMD increase the risk of developing more advanced disease.
Our group evaluated the relationship between drusen size progression, common and rare AMD genetic variants, and diet12 to gain a better understanding of the biology of drusen growth that could lead to preventive measures and thwart the development of vision-disabling forms of AMD. We reported for the first time that a healthy diet—specifically, higher adherence to the Mediterranean diet—was linked with a lower risk of drusen growth.
To investigate this nexus of genetics, diet and drusen growth, we evaluated 1,838 patients (3,023 eyes) at risk for drusen progression based on fundus photographs graded at a reading center. These patients had an average follow-up time of 10.2 years in the Age-Related Eye Disease database.
Evaluating the role of diet
We calculated an alternate Mediterranean diet (aMeDi) score based on the food frequency questionnaire, an instrument that’s been used to estimate the prevalence of the Mediterranean diet in the United States. Our group published the first report that demonstrated the aMeDi score was linked to progression to advanced AMD.5 These findings were later confirmed in a European cohort.13 The aMeDi score includes these nine components
 |
|
Figure 1. The Mediterranean diet emphasizes plant-based foods and fish over poultry, dairy and meat. |
(Figure 1):
- vegetables (excluding potatoes);
- fruits;
- legumes;
- whole grains;
- nuts;
- fish;
- red and processed meats;
- alcohol consumption; and
- the ratio of monounsaturated to saturated fatty acid (MUFA:SFA).
Scores of 1 or 0 were assigned depending on intake of these components. A score of 9 represents perfect adherence; 0 represents complete non-adherence. For our purposes, we categorized aMeDi scores in two categories: low (0 to 3); and medium-high (4 to 9).
Genotype data
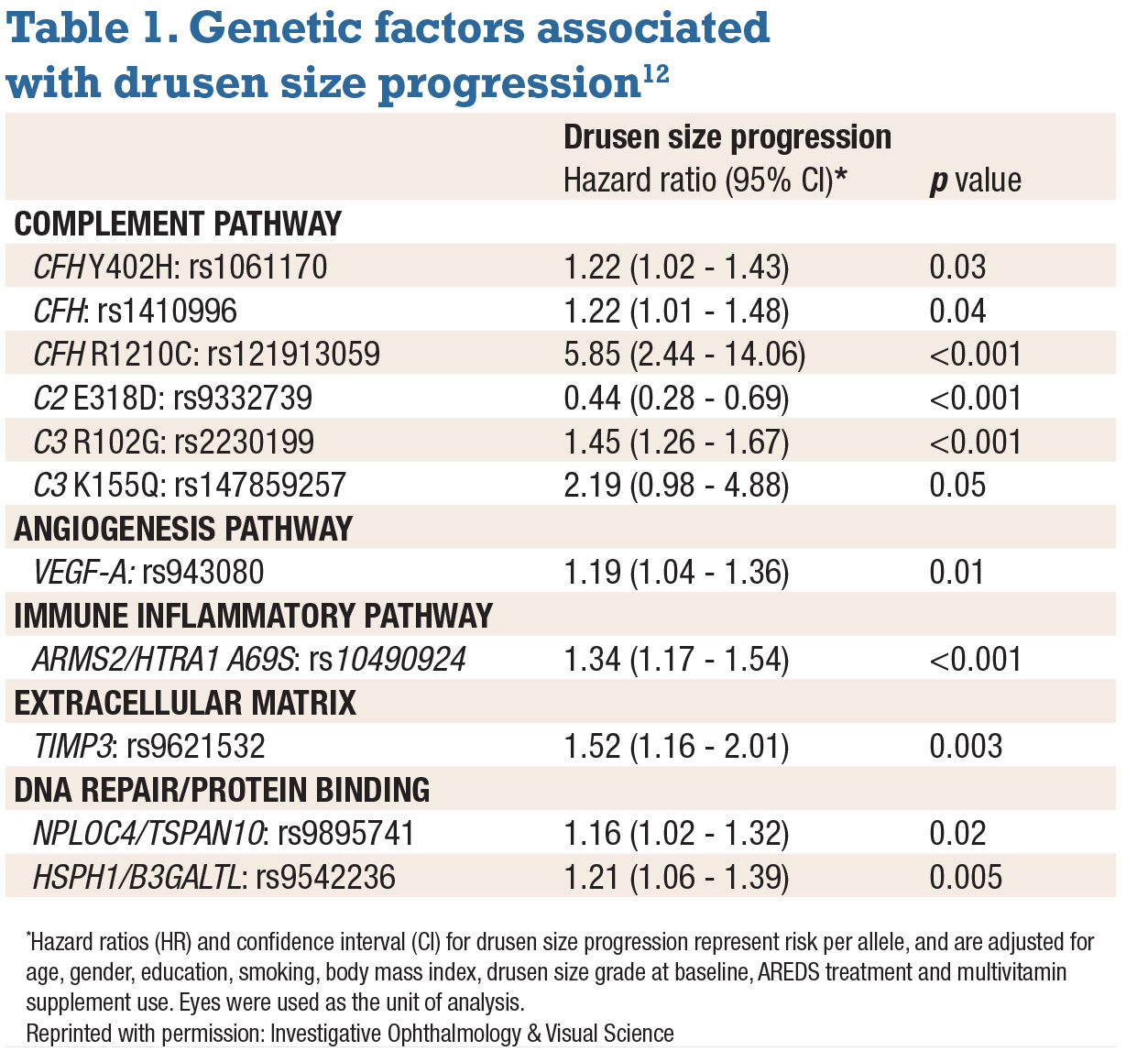
We found that the following genetic variants in the complement pathway were significantly associated with a two-step progression in drusen size, adjusting for other covariates:
- CFH Y402H;
- CFH rs1410996;
- CFH R1210C;
- C2 E318D;
- C3 R102G; and
- C3 K155Q.
Variants in the following genes were also significantly associated with a two-step progression in drusen size:
- ARMS2/HTRA1;
- VEGF-A;
- TIMP3;
- NPLOC4; and
- HSPH.
The C2 E318D protective allele conferred decreased risk, adjusting for other covariates.
Drusen size drivers
 |
| Click table to enlarge. |
Drusen size increased twofold in 8 percent of eyes at five years, and 19 percent had drusen growth at 10 years. Non-genetic factors associated with higher risk of drusen progression were older age, smoking and larger drusen size at baseline.
A number of factors didn’t differ between patients with and without drusen progression: gender, education level, body-mass index, history of AREDS treatment and multivitamin use.
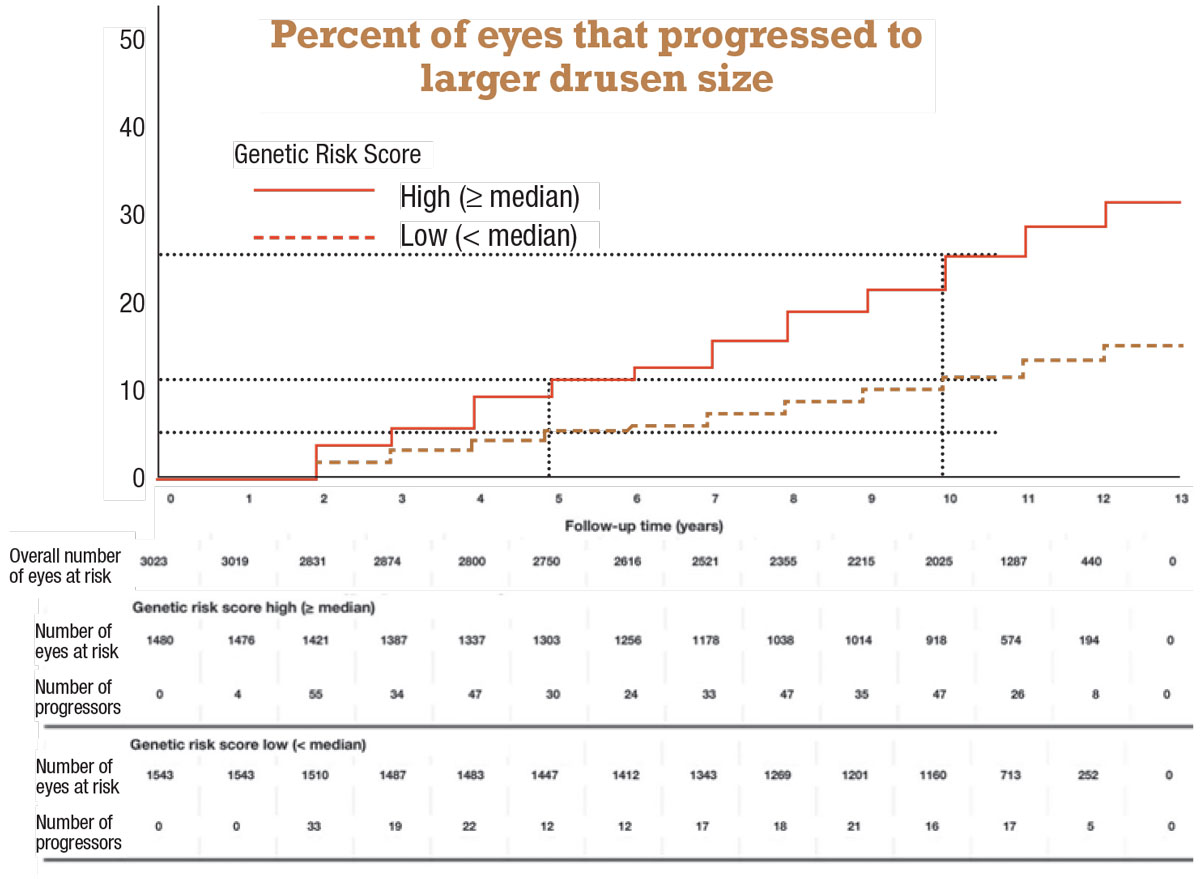
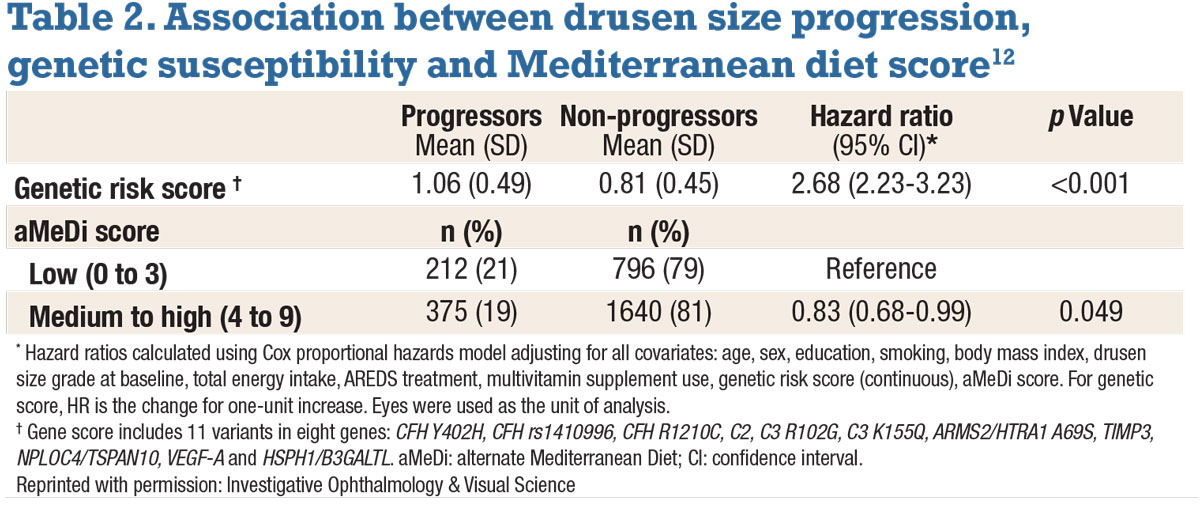
We calculated a genetic risk score based on the 11 genetic variants in eight genes that were related to drusen growth (Table 1), and determined the association between drusen size growth, gene variants and adherence to the Mediterranean diet using the aMeDi score.
A higher genetic risk score was associated with drusen size progression—specifically a hazard ratio of 2.68 for each one-unit increase in score (p<0.001) (Table 2). Likewise, adherence to the Mediterranean diet yielded a 17-percent lower risk of progression in patients with medium to high aMeDi scores.
A Kaplan-Meier analysis depicts the association with genetic risk score more clearly (Figure 2). Among patients with lower genetic risk scores—that is, below the median—the rates of drusen progression were 6 percent at five years, doubling to 12 percent at 10 years. However, in eyes with higher-than-median genetic risk scores, those rates were doubled or more: 12 percent at five years and 26 percent at 10 years.
Risk alleles linked to drusen growth
 |
|
Figure 2. Kaplan-Meier curves for the probability of eyes progressing to larger drusen size (two steps) by follow-up time according to high or low Genetic Risk Score. (Reprinted with permission: Investigative Ophthalmology & Visual Science). Click image to enlarge. |
Our study findings elucidate the role of specific gene variants and a genetic risk score in the earlier stages of AMD. They provide further evidence that the following genes have a role in drusen progression:
• High-impact, rare CFH R1210C mutation. This mutation has been shown to compromise C-terminal factor H function. Our group has published studies showing the association of this variant with higher drusen burden, earlier age of AMD onset and progression to advanced disease, and also earlier age of progression to advanced stages of AMD.10,14-17 Our most recent study found an almost sixfold greater risk (HR 5.85, p<0.001) for drusen growth among carriers of this mutation.
• Common C3 R102G and rare C3 K155Q variants. These variants impact C3 protein regulation, an implicating factor in AMD.18,19 Ours is the first study to explore the role these variants have on drusen size progression.
• Common variant in the gene locus ARMS2/HTRA1. The role of this variant isn’t understood as well as the complement pathway in AMD pathogenesis, but it has been implicated in non-advanced AMD.8,9,11 Our previous study using optical coherence tomography found a link between this variant, along with CFH and larger drusen area and volume.16
• VEGF-A. Implicated in advanced AMD, the role of this gene in the angiogenesis pathway has been specifically linked to cell growth and vascular permeability.20 However, its role in drusen progression is still unclear.
• TIMP3. TIMP3 is a tissue inhibitor of metalloproteinase-3, an extracellular matrix protein. A mutation in this gene has been reported to disrupt the retinal pigment epithelial membrane.21
Dietary factors
Prospective studies in the United States and Europe have documented the protective effects of the Mediterranean diet against AMD.5,13 The elements of the Mediterranean diet have been well documented: fish rich in omega-3 fatty acids, fruits, vegetables, legumes, olive oil and nuts. These foods contain vitamins and minerals such as vitamins B, C and E, zinc, lutein and zeaxanthin, as well as healthy fats that nourish vision, act as antioxidants and have anti-inflammatory properties.1,3,4,22,23
 |
| Click image to enlarge. |
We found lower levels of systemic inflammatory biomarker C-reactive protein in patients who consumed higher concentrations of lutein and zeaxanthin, vitamin C and fish, also supporting the anti-inflammatory role of this type of diet.24
Bottom line
We’ve closed some of the knowledge gaps surrounding factors associated with drusen growth, and we’ve provided more information on genetic variants that may influence drusen growth that can lead to progression from early to advanced AMD. Recent study results underscore the role a healthy diet may have in the pathogenesis of this disease, even in the earlier stages.12,25 These findings can help us develop strategies to better manage AMD progression in the most vulnerable patients. RS
REFERENCES
1. Seddon JM. Macular Degeneration Epidemiology: Nature-Nurture, Lifestyle Factors, Genetic Risk, and Gene-Environment Interactions – The Weisenfeld Award Lecture. Invest Ophthalmol Vis Sci. 2017;58:6513-6528.
2. Seddon JM, Willett WC, Speizer FE, Hankinson SE. A prospective study of cigarette smoking and age-related macular degeneration in women. JAMA. 1996;276:1141-1146.
3. Seddon JM, Ajani UA, Sperduto RD, et al. Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration. Eye Disease Case-Control Study Group. JAMA. 1994;272:1413-1420.
4. Seddon JM, Cote J, Rosner B. Progression of age-related macular degeneration: Association with dietary fat, transunsaturated fat, nuts, and fish intake. Arch Ophthalmol. 2003;121:1728-1737.
5. Merle BMJ, Silver RE, Rosner B, Seddon JM. Adherence to a Mediterranean diet, genetic susceptibility, and progression to advanced macular degeneration: A prospective cohort study. Am J Clin Nutr. 2015;102:1196-1206.
6. Yu Y, Wagner EK, Souied EH, et al. Protective coding variants in CFH and PELI3 and a variant near CTRB1 are associated with age-related macular degeneration. Hum Mol Genet. 2016;25:5276-5285.
7. Fritsche LG, Igl W, Bailey JNC, et al. A large genome-wide association study of age-related macular degeneration highlights contributions of rare and common variants. Nat Genet. 2016;48:134-143.
8. Seddon JM, Rosner B. Validated prediction models for macular degeneration progression and predictors of visual acuity loss identify high-risk individuals. Am J Ophthalmol. 2019;198:223-261.
9. Yu Y, Reynolds R, Rosner B, Daly MJ, Seddon JM. Prospective assessment of genetic effects on progression to different stages of age-related macular degeneration using multistate Markov models. Invest Ophthalmol Vis Sci. 2012;53:1548-1556.
10. Seddon JM, Reynolds R, Yu Y, Rosner B. Three new genetic loci (R1210C in CFH, variants in COL8A1 and RAD51B) are independently related to progression to advanced macular degeneration. PloS One. 2014;9:e87047.
11. Seddon JM, Silver RE, Kwong M, Rosner B. Risk Prediction for Progression of Macular Degeneration: 10 Common and Rare Genetic Variants, Demographic, Environmental, and Macular Covariates. Invest Ophthalmol Vis Sci. 2015;56:2192-2202.
12. Merle BMJ, Rosner B, Seddon JM. Genetic susceptibility, diet quality, and two-step progression in drusen size. Invest Ophthalmol Vis Sci. 2020:61:17.
13. Merle BMJ, Colijn JM, Cougnard-Grégoire A, et al. Mediterranean diet and incidence of advanced age-related macular degeneration: The EYE-RISK Consortium. Ophthalmology. 2019;126:381-390.
14. Raychaudhuri S, Iartchouk O, Chin K, et al. A rare penetrant mutation in CFH confers high risk of age-related macular degeneration. Nat Genet. 2011;43:1232-1236.
15. Ferrara D, Seddon JM. Phenotypic Characterization of Complement Factor H R1210C Rare Genetic Variant in Age-Related Macular Degeneration. JAMA Ophthalmol. 2015;133:785-791.
16. Seddon JM, Dossett JP, Widjajahakim R, Rosner B. Association between perifoveal drusen burden determined by OCT and genetic risk in early and intermediate age-related macular degeneration. Invest Ophthalmol Vis Sci. 2019;60:4469-4478.
17. Seddon JM, Widjajahakim R, Rosner B. Rare and common genetic variants, smoking, and body mass index: Progression and earlier age of developing advanced age-related macular degeneration. Invest Ophthalmol Vis Sci. 2020; 61:32.
18. Seddon JM, Yu Y, Miller EC, et al. Rare variants in CFI, C3 and C9 are associated with high risk of advanced age-related macular degeneration. Nat Genet. 2013;45:1366-1370.
19. Maller JB, Fagerness JA, Reynolds RC, Neale BM, Daly MJ, Seddon JM. Variation in complement factor 3 is associated with risk of age-related macular degeneration. Nat Genet. 2007;39:1200-1201.
20. Yu Y, Bhangale TR, Fagerness J, et al. Common variants near FRK/COL10A1 and VEGFA are associated with advanced age-related macular degeneration. Hum Mol Genet. 2011;20:3699-3709.
21. Jacobson SG, Cideciyan AV, Bennett J, Kingsley RM, Sheffield VC, Stone EM. Novel mutation in the TIMP3 gene causes Sorsby fundus dystrophy. Arch Ophthalmol. 2002;120:376-379.
22. Reynolds R, Rosner B, Seddon JM. Dietary omega-3 fatty acids, other fat intake, genetic susceptibility, and progression to incident geographic atrophy. Ophthalmology. 2013;120:1020-1028.
23. Merle BMJ, Silver RE, Rosner B, Seddon JM. Dietary folate, B vitamins, genetic susceptibility and progression to advanced nonexudative age-related macular degeneration with geographic atrophy: A prospective cohort study. Am J Clin Nutr. 2016;103:1135-1144.
24. Seddon JM, Gensler G, Klein ML, Milton RC. C-reactive protein and homocysteine are associated with dietary and behavioral risk factors for age-related macular degeneration. Nutrition. 2006;22:441-443.
25. Thompson JT, Seddon JM. Eat Right For Your Sight: Simple, Tasty Recipes That Help Reduce the Risk of Vision Loss from Macular Degeneration. American Macular Degeneration Foundation. New York, NY; The Experiment, LLC; 2015.



