 |
|
Have a question for “Coding Commentary”? Tweet it to us at | |
|
Bio |
It’s been just over a year since the American Medical Association released significant changes to evaluation and management (E/M) coding.1 In many ways, the documentation requirements under E/M 2021 are less onerous than the previous versions: Element counting, box checking and few relevant case examples made using E/M difficult.
The 2021 revisions don’t require any specific history, review of systems or exam element documentation. The encounter is coded based on medical decision making (MDM). Though you continue to document the patient’s relevant history and exam, under E/M the purpose of your exam documentation is for supporting your care and mitigating risk, not for selecting an exam code.
Straightforward approach to coding
Coding based on MDM is relatively straightforward. As with the previous versions of E/M and its more obscure grid, you must meet or exceed two of the three boxes in a code level to score an exam. For example, a patient with acute retinal detachment with a high chance of vision loss who requires urgent surgery slots nicely into the E/M rules as an E/M Level 5 (992x5), as you can see in Table 1.
For most of your exams, you’ll rely on the third column, “Number and complexity of problems addressed,” and the fifth column, “Risk of complications and/or morbidity or mortality of patient management.”
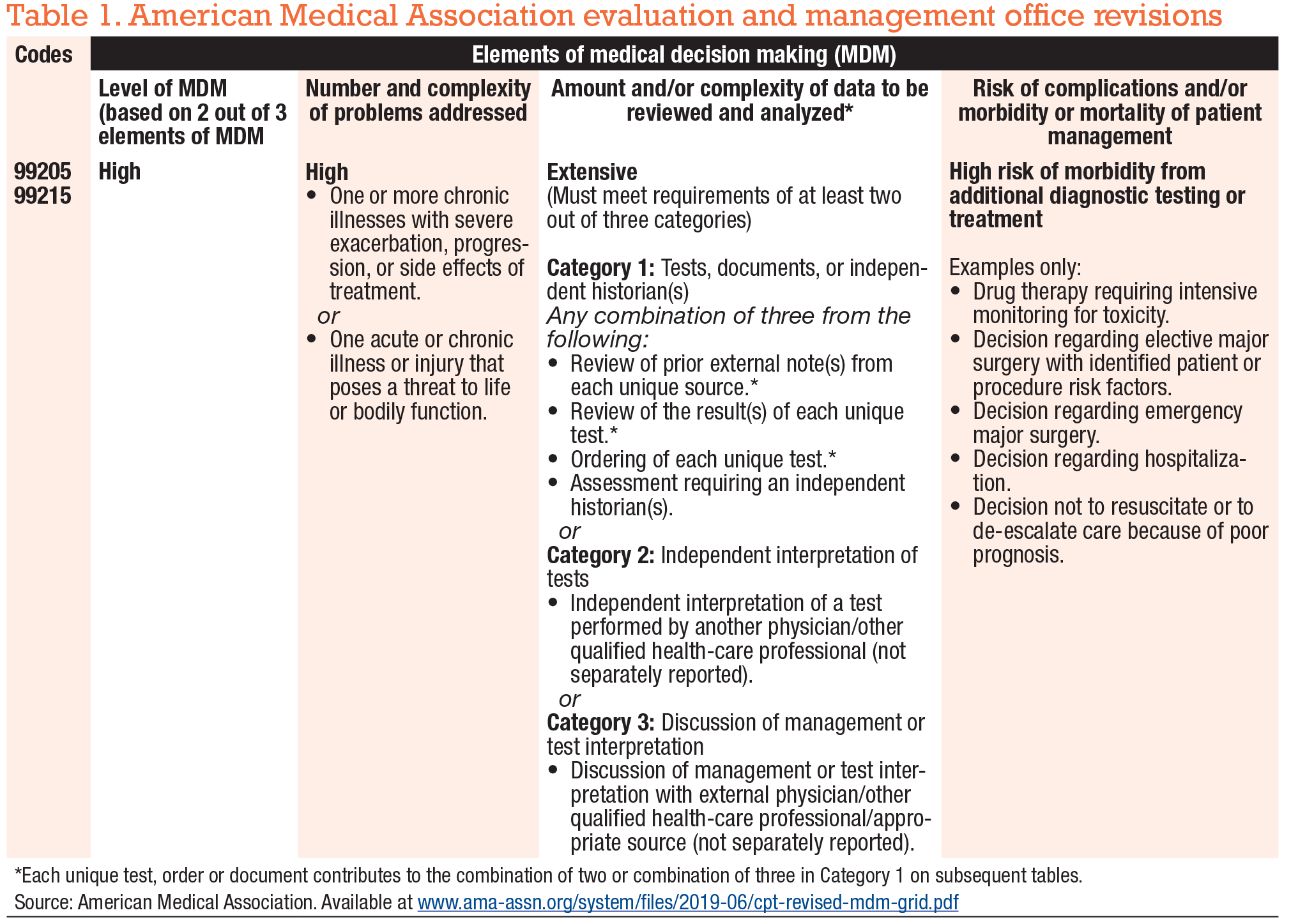 |
However, at this point, you’re no doubt wondering what that big, text-heavy fourth column is all about. What is “Amount and/or complexity of data to be reviewed and analyzed”? Can that column help code a complex exam? Ophthalmologists often dismiss the column, colloquially referred to as “Data,” as irrelevant. In truth, it’s of little use on a daily basis. But with a year’s experience, we’ve learned this column has some usefulness. Let’s explore this further so you have another coding tool in your toolbox.
 |
Understanding the ‘Data’ column
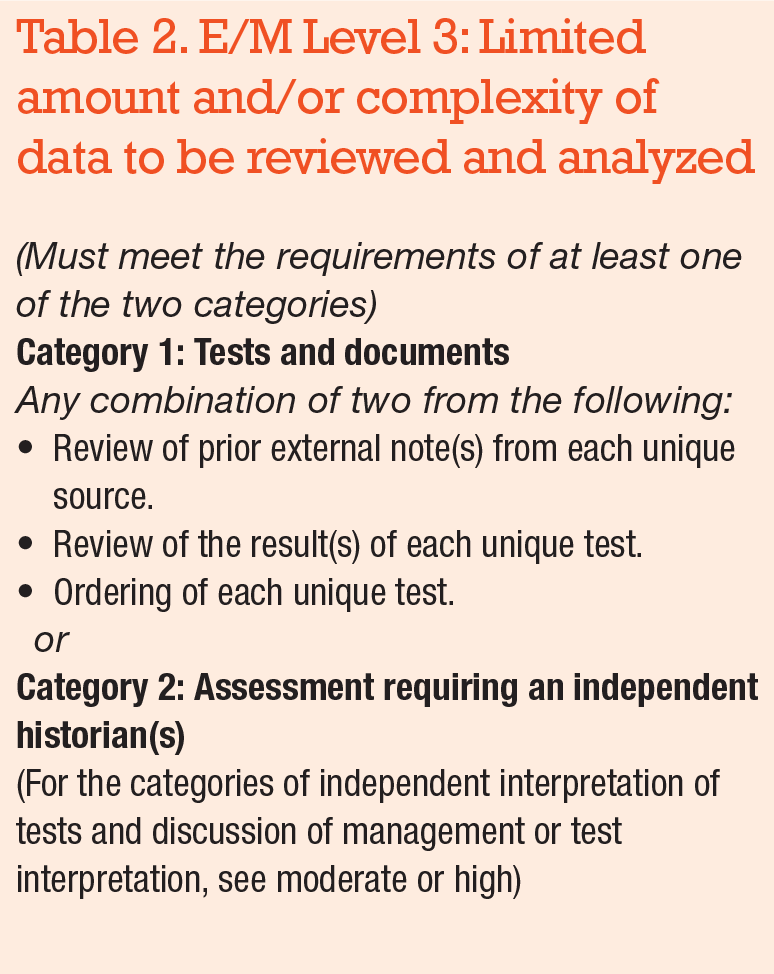
The data column is easiest to explain by starting with E/M Level 3, 992x3 (Table 2). First, keep in mind that a Level 3 exam is for a stable, low-risk condition with a low risk from treatment. Setting aside the Eye Codes for this discussion (920x4 and 920x2), a Level 3 exam might be a three-month, background diabetic retinopathy patient with relatively stable disease, requiring continuation of intravitreal injection in one eye. But if your patient doesn’t require any treatment at all, could you still code a Level 3 exam? In Table 2 note that, if you meet the requirements of only one of two categories of data, you might be able to code the exam as a Level 3 even absent of any treatment on the date of service.
For example, in Table 2 , Category 1, reviews of a referring physician’s clinic note and of a fluorescein angiography done outside your practice would constitute two tests or documents to meet the data requirement.
Alternatively, if your patient is unable to communicate their history because of cognitive issues and a health-care proxy is available to provide that information, you meet the Category 2 requirement of “Assessment requiring an independent historian.”
Some important points to remember at this stage of your data education:
- A review of external note(s) from each unique source means all of the exam notes from one outside provider. Four exams from Dr. Icee is considered one review point.
- Although the AMA doesn’t clarify it, the review of each unique test doesn’t specify who provided the test to you. A fluorescein angiogram and an optical coherence tomography from Dr. Icee are considered two tests.
- Ordering a unique test doesn’t include tests for which you receive reimbursement, such as an OCT that you order, interpret and bill to insurance. No double-dipping by getting data credit and test reimbursement.
- An independent historian doesn’t include American Sign Language or English translators.
 |
More complex Level 4 data
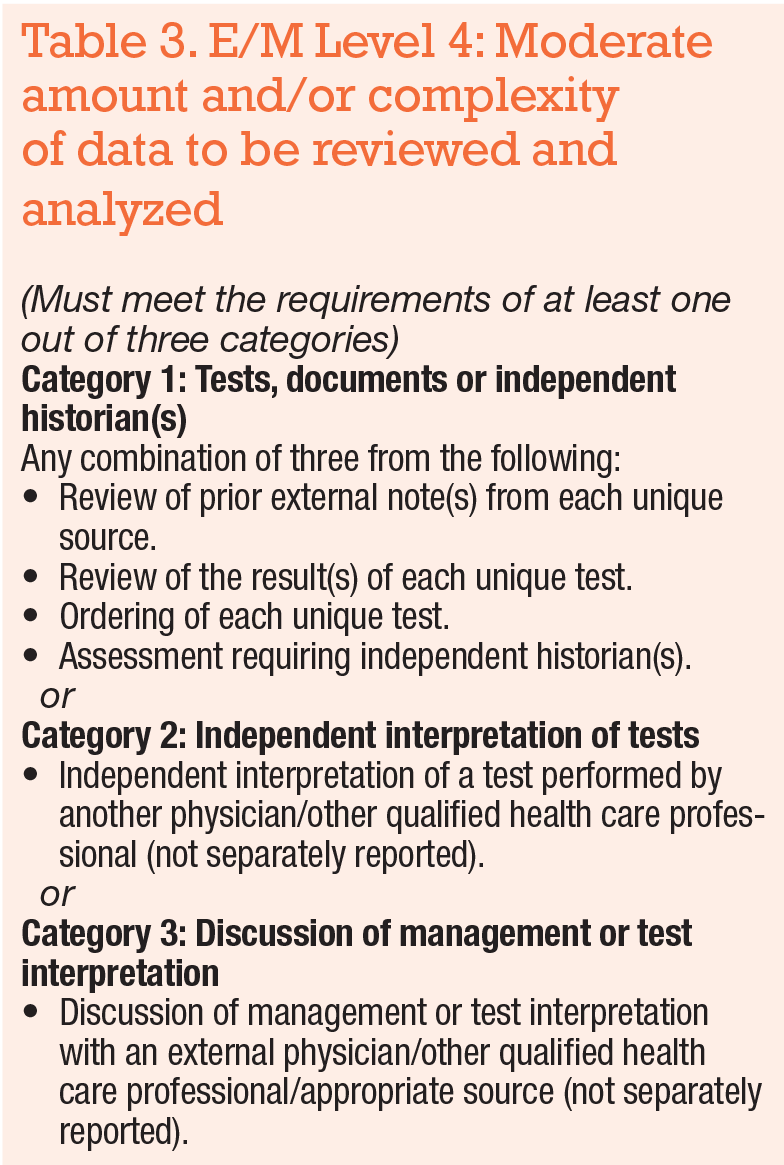
With an understanding of Level 3 data, let’s move to the more complex Level 4 (Table 3, page 36).
The first important point is that you must meet one of three categories. Note that the independent historian is in Category 1 in this table. The other Category 1 requirements are the same as the previous table. Also note you need three of the Category 1 tests, documents, or independent historian items, whereas in the Level 3 table you only need two.
Points to remember:
- Category 2, “Independent interpretation of tests.” As with the “ordering of each unique test” in Category 1, the Category 2 tests can’t be those for which you receive reimbursement. Thus interpreting an OCT done elsewhere would qualify, but your documentation must be meticulous if you plan to use Category 2 test interpretation. Your chart note must include the name of the test, the date, reliability, and your independently drawn conclusion.
- Category 3, “Discussion of management or test interpretation,” is just as it sounds. You must have a conversation with a provider outside your organization; text messages or emails don’t count as a discussion. As with Category 2, you need to carefully document who you spoke with as well as the issues discussed and the outcome of the discussion.
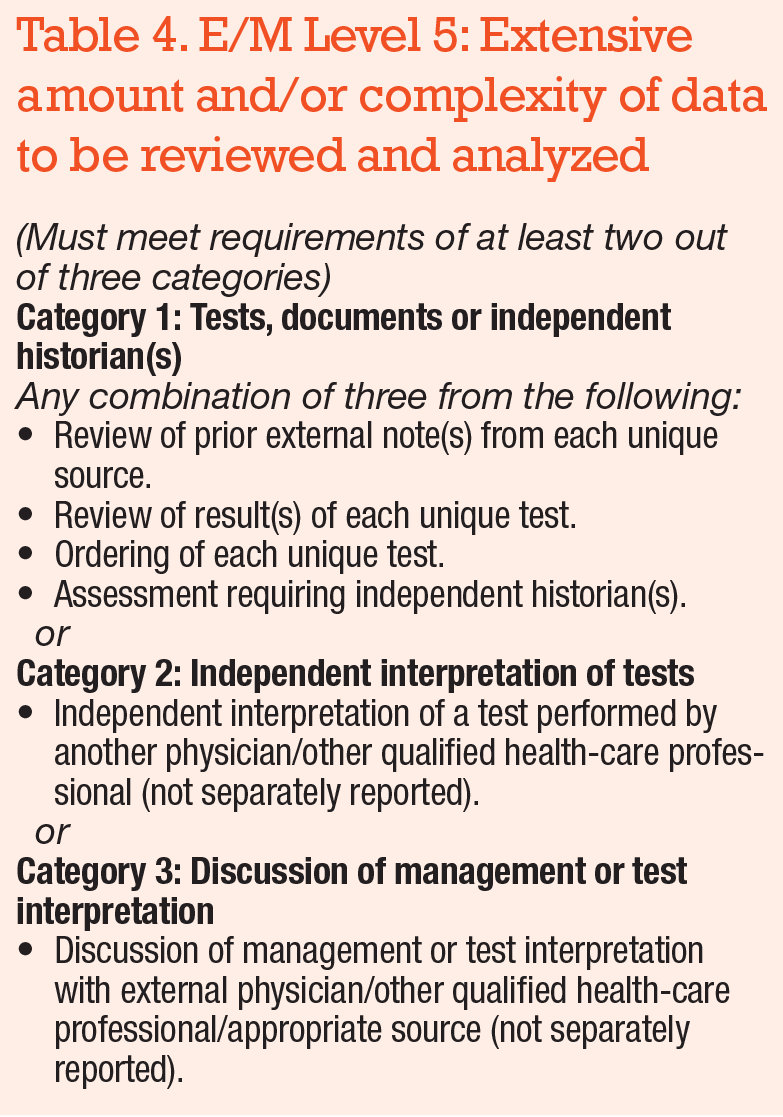 |
Level 5: A higher bar
Let’s move to Level 5 data. In Table 4, you’ll notice the bar has gotten quite a bit higher. You must meet or exceed the requirement, so you must fulfill two of the three Categories. The Categories are the same as in Level 4 data; you just need to do more work. Careful documentation is a must if you plan to apply data to a Level 5 encounter.
Now that you have an understanding of what “data” means, you may think you’ll never use this option, but consider this: You’ll occasionally see patients who take time to determine appropriate treatment, but not enough to bill based on time; or who are complex or have potentially vision-threatening disease, but whom you won’t be treating, perhaps because the patient has non-retinal pathology and you refer them elsewhere for treatment.
“Data” is the category that can allow you to be reimbursed appropriately for these cases. For example, you may have a young patient with optic neuropathy. Your suspicion is previously undiagnosed multiple sclerosis; you order an MRI (one Category 1 test, inadequate to qualify for Category 1) and call a neurologist to assure a consultation is arranged; the neurologist is aware of the MRI and will interpret it (Category 3 fulfilled). In this case, you would meet the billing requirements for E/M Level 4 for this unfortunate situation.
Admittedly, using “data” to code your exams will be an unusual event. When you have a difficult case but you won’t ultimately be the treating physician, consider documenting data to be paid appropriately for the expertise you applied to triage the patient. As with any coding challenge, having additional tools at hand will help you do it correctly. RS
REFERENCE
1.American Medical Association. CPT Evaluation and Management E/M Revisions. Updated March 9, 2021. Accessed February 28, 2022. Available at: https://www.ama-assn.org/practice-management/cpt/cpt-evaluation-and-management




