 |
COVID-19 has tangled our world into a web of disruption at every turn. For many clinics, testing has been deferred to minimize patient-clinician contact and patient time in the clinic. But now it’s important to get back up to speed on testing rules to avoid costly errors. Denied claims are especially painful as we try to recover from the toll of COVID-19.
‘Bundled’ services
You may recall from previous articles that Medicare has a program called the National Correct Coding Initiative (NCCI). NCCI rules create “bundles” of services that aren’t permitted to be billed together when performed on the same date of service. Even when we were running our practices in what was our prior state, bundles caused confusion for our most commonly performed retina testing: optical coherence tomography, fundus photography and extended ophthalmoscopy.
OCT of the retina (92134) has been mutually exclusive with fundus photography (92250) since 2011, when CPT 92134 was implemented. It’s important to note that FA (92235) and ICG angiography (92240) are not bundled with OCT. Interestingly, OCT isn’t bundled with extended ophthalmoscopy (92201 and 92202), although many payer policies discourage the combination.
Although extended ophthalmoscopy (92201 or 92202) isn’t bundled with OCT, it is bundled with fundus photography. You may encounter circumstances where a photograph of a glaucomatous optic nerve (92250) is appropriate on the same date of service as an extended ophthalmoscopy of a peripheral nevus (92201).
Because 92250 and 92201 are bundled, if you submit a claim for both services you will most likely be reimbursed for the lower-
paying code (92201). A more logical strategy is to submit the claim for only the higher-
paying photography code and not bill the extended ophthalmoscopy. Alternatively, if either test is nonurgent, you could consider performing them on separate days. It wouldn’t be wise to attempt to “break the bundle” on the NCCI edit just to get paid.
Untangling the bundles
One significant consideration is submitting a claim for the higher-paying test when you perform bundled services that have the same level of medical necessity on the same date. This is critical.
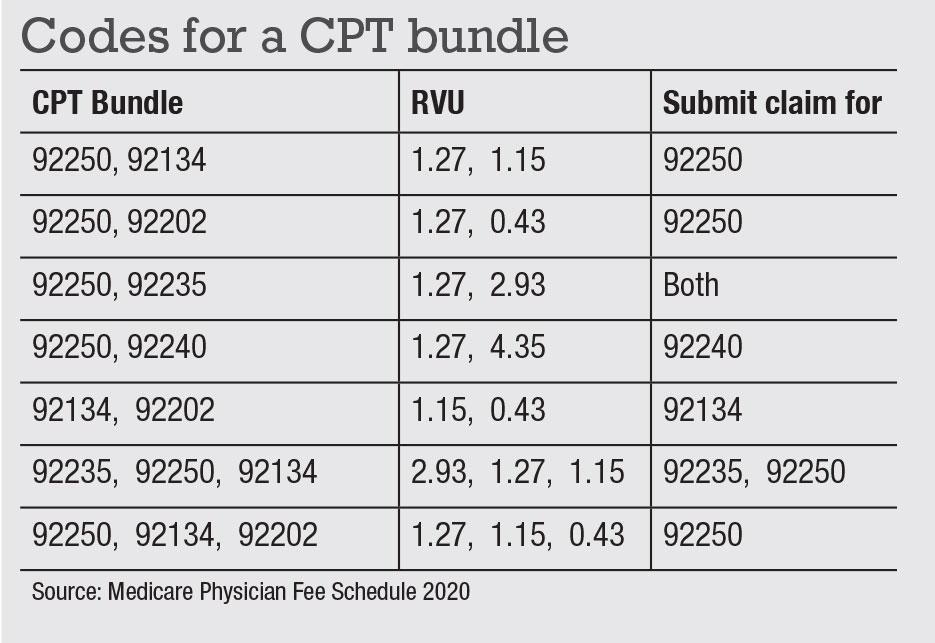
Assuming all testing carries the same weight of medical necessity, the accompanying table will help you untangle the bundles by reimbursement levels. Note that when billing more than two tests, Medicare’s multiple procedure payment rules will change the reimbursement for some tests with a lesser-valued technical component.
 |
Recovery mode
We hope you’re able to recover from the pandemic and use the crisis as a learning experience to improve clinical procedures. It may be that your need to move patients through the clinic more efficiently leads to a strain on your ability to document, select appropriate codes and in general pay attention to the minutiae of billing. We hope this will get your thought processes re-engaged, allowing you to optimize your revenue during recovery.
Stay safe. RS



