 |
 |
Whether it is the ancient Greek legend of Amphiaraus or the blockbuster film “Minority Report,” people have always been fascinated by the idea of predicting the future—a fascination that has been deeply entrenched within medicine for generations.
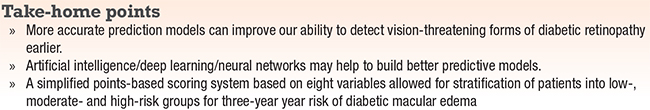
Improvements in data collection and processing, including the utilization of large databases and the evolving field of machine learning/artificial intelligence, have refocused medicine’s interest in predictive analytics. Developing prediction models that can rapidly and accurately assess patients’ risk of future morbidity may help revolutionize patient care.
Diabetes is one area that could benefit tremendously from better prediction models. Early detection is the cornerstone of the management of the ocular manifestations of diabetes. Detecting vision-threatening forms of diabetic retinopathy (VTDR) is important because they can have catastrophic consequences to individual patients while also carrying a high societal cost.
 |
This article reviews the state of the science of using predictive models in medicine and how “big data” has the potential to help physicians identify patients at greatest risk of progressing onto severe disease. We will also explore our institution’s work in developing a predictive model for diabetic macular edema.
Risk calculators in medicine
Risk calculators have been a mainstay in medicine for decades, most notably in cardiology, where medical management decisions rely heavily on risk-stratification algorithms derived from robust clinical data. Clinical questions such as a patient’s optimal blood pressure, cholesterol or anticoagulation status are based on one’s 10-year risk of cardiovascular events, which can be readily calculated using several key variables
Although Michael Klein, MD, and colleagues provided a popular tool for predicting the 10-year risk of advanced age-related macular degeneration,1 ophthalmology has lagged behind other specialties in developing risk-stratification tools and clinical prediction analysis. This is partly because of the complexity of assessing the risk of ophthalmic disease, which requires incorporating not only ophthalmic factors but also their interaction with systemic factors to create an overall risk estimate. Further compounding this difficulty is the abundance of possible data points; it remains unclear which ones are worthy of inclusion into any model.
 |
Role of AI and neural networks
This is one area where artificial intelligence/deep learning/neural networks may help expand our capacity to build better predictive mod- els. Whereas previous attempts to build models required the use of multiple regression analyses and user-defined inputs, AI could detect a number of variables that a user might not even realize need to be considered.
The ability to examine a database with AI may help solve some of our current limitations, because AI can analyze data “in bulk,” allowing machine learning algorithms to work their way through multiple threads of data to isolate the factors that have the most value.
Similarly, our ability to incorporate features from fundus photography into prediction analysis is limited by current methods for manual interpretation and the finite number of macroscopic details that can be defined.
 |
Role of neural networks
Neural networks, on the other hand, have the capacity to rapidly assess quantifiable metrics such as capillary density or vascular diameter, and they can search for yet undefined clues within fundus photographs to build a predictive model. That would be impractical for a human grader to do on a large scale.
Significant work remains on how to optimally utilize AI to build the best models. For example, an AI-based model may examine every piece of data in a patient’s medical history—laboratory values, home address, family history and hospital bed, and conclude that patients admitted to the fifth floor of the hospital have higher risk of perioperative mortality.
That might seem like a fascinating insight at first, which would compel further investigation into whether there are breakdowns in clinical care on the fifth floor or if some previously unaccounted for factor (like bad fung shui) was responsible for this heightened mortality. However, upon further inspection, you might learn that the fifth floor is where the surgical intensive care unit is located, explaining why there is greater mortality there compared to non-intensive care unit floors.
Stratifying risk for VTDR
As retina specialists know too well, DME is an important cause of visual morbidity and the leading cause of new onset blindness among adults in the United States.
In addition to its direct visual consequences, DME is associated with a loss of work productivity and a high treatment burden with frequent clinic visits and costly interventions.2 Broadly speaking, the care of diabetic patients constitutes 10 percent of U.S. health-care costs,3 and caring for patients with DME is almost 30 percent more expensive than the treatment of their peers.4
Earlier detection and treatment of diabetic macular edema is associated with better visual outcomes and reduced injection burden, thus benefiting patients as well as reducing the cost to the health-care system.5
 |
Few patients drive cost burden
Although the individual and societal costs of diabetic retinopathy are considerable, these costs are largely driven by a minority of patients. Most studies estimate that 10 percent of diabetes patients have VTDR, which is consistent with our experience within Kaiser Permanente.
The challenge in diabetes care is that we spend a significant amount of time and effort screening all patients to identify the relatively few that require more intensive evaluation and management. More accurately stratifying patient risk for VTDR would have substantial benefits.
We could initiate more aggressive systemic management of diabetes when the opportunity to prevent worsening retinopathy is greatest. We could screen patients more closely to detect and treat pathology earlier, allowing for a better prognosis. And we could use our resources more judiciously on the highest risk patients while letting lower-risk patients “pass through” with less frequent screening.
Although the duration of diabetes and long-term glycemic control are well established as important risk factors for VTDR, investigations into secondary risk factors have produced mixed results.
Isolating individual risk factors
Further, most studies examine the role of individual risk factors in isolation and if they are independently associated with the risk of VTDR. It remains unclear how various risk factors interact to create a global risk for VTDR. It’s not uncommon to see a patient with a remarkably elevated hemoglobin A1c but no significant morbidity, while other patients can have significant retinal pathology.
 |
Intuitively, we can tell there is more to retinopathy risk than just the hemoglobin A1c and disease duration. Genetics appears to play a role in the risk of retinopathy,6 although accounting for individual genetic variations on a wide-scale clinically is not presently practical. If we could determine how various ocular and systemic risk factors interact to create a global individualized risk for patients, we could provide improved and more personalized care.
Ideally, a model would predict the risk of DME several years in advance to allow for sufficient time for aggressive systemic treatment to modify the disease course to prevent worsening retinopathy. Such a model may also help identify the specific targets for various systemic risk factors. Perhaps a patient’s A1c should be adjusted based on one’s degree of retinopathy and other risk factors, such as renal status.
Efforts to predict progression
Marco Dutra Medeiros, MD, and colleagues in Portugal performed a longitudinal epidemiologic study that found that duration of diabetes, age at diagnosis, and insulin use were associated with an increased risk of incidence as well as progression of diabetic retinopathy.7
They suggested these findings could serve as the foundation for personalized screening schedule. However, the ability to generalize their results is unclear for non-Portuguese populations because race likely plays a role in the risk of DR progression.
Rajeev Pappuru, MD, and colleagues reported on an image-based approach to predict diabetic retinopathy progression using analyses of fundus photography.8 They examined the outcomes of 205 patients over the course of two years and found that microaneurysm turnover was a good predictor of retinopathy worsening (based on Early Treatment Diabetic Retinopathy Study grading step changes and development of macular edema).8
Bottom line
Bringing together both ocular and systemic variables to predict the risk of VTDR would likely lead to superior prediction models since diabetes is fundamentally a systemic disease. We recently started doing our own work in this area (sidebar, page 36).
Although much work needs to be done before prediction models are ready for “prime time,” we continue to inch closer to a reality once only en- visioned by science fiction writers.
REFERENCES
1. Klein ML, Francis PJ, Ferris FL 3rd, Hamon SC, Clemons TE. Risk assessment model for development of advanced age-related macular degeneration. Arch Ophthalmol. 2011;129:1543-1550.
2. Pershing S, Enns EA, Matesic B, Owens DK, Goldhaber- Fiebert JD. Cost-effectiveness of treatment of diabetic macular edema. Ann Intern Med. 2014;160:18-29.
3. Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Centers for Disease Control and Prevention; Atlanta, GA: Dec 8, 2011. Accessed at www.cdc.gov/diabetes/pubs/ pdf/ndfs_2011.pdf. 2011.
4. Shea AM, Curtis LH, Hammill BG, et al. Resource use and costs associated with diabetic macular edema in elderly persons. Arch Ophthalmol. 2008;126:1748-1754.
5. Wykoff CC, Elman MJ, Regillo CD, Ding B, Lu N, Stoilov I. Predictors of diabetic macular edema treatment frequency with ranibizumab during the open-label extension of the RIDE and RISE trials. Ophthalmology. 2016;123:1716-1721.
6. Graham PS, Kaidonis G, Abhary S, et al. Genome- wide association studies for diabetic macular edema and proliferative diabetic retinopathy. BMC Med Genet. 2018;19:71.
7. Dutra Medeiros M, Mesquita E, Gardete-Correia L, et al. First incidence and progression study for diabetic retinopathy in Portugal, the RETINODIAB study: evaluation of the screening program for Lisbon Region. Ophthalmology. 2015;122:2473-81.
8. Microaneurysm turnover is a predictor of diabetic retinopathy progression. Pappuru RKR, Ribeiro L, Lobo C, Alves D, Cunha- Vaz J. Br J Ophthalmol. 2019;103:222-226.
9. Modjtahedi BS, Wang Y, Luong TQ, Fong DS. Development of a points-based risk score to predict the three-year risk of DME. Paper presented at American Academy of Ophthalmology Annual Meeting; October 27, 2018: Chicago, IL.



