Ionis Pharmaceuticals describes FB-LRX as a second-plus generation ligand-conjugated antisense drug designed to reduce production of complement factor B (FB), a key protein that has been implicated in a number of complement-mediated diseases, among them dry age-related macular degeneration. FB is produced mostly in the liver and circulates in high levels throughout the vascular system, including the retinal vasculature.
Ionis has partnered with Genentech/Roche to develop the geographic atrophy/dry AMD program for FB-LRX. It’s not the only program the two are partnering on. There’s a separate program for FB-LRX for immunoglobulin A nephropathy, along with an investigational antisense therapy for Huntington’s disease that’s in Phase III trials.
 |
At the Angiogenesis, Exudation and Degeneration 2020 meeting in Miami, Sunil Patel, MD, PhD, presented Phase I results of the GOLDEN trial of 52 healthy volunteers exposed to either single or multiple doses of FB-LRX or placebo.1 The trial reported that the drug produced significant dose-dependent reductions in plasma FB levels along with other key mediators in the systemic complement. Other than moderate adverse events, which were comparable between both the treatment and placebo groups, the study reported no significant safety or tolerability findings.
Now development of FB-LRX is moving into Phase II in patients with GA. Here, David S. Boyer, MD, senior partner with Retina-Vitreous Associates Medical Group in Los Angeles, and an investigator of the trial, answers questions about FB-LRX. Dr. Boyer is a consultant to Genentech/Roche and Apellis Pharmaceuticals.
Describe the mechanism of action in your own words.
FB-LRX is an antisense oligonucleotide (ASO). These are short, single-strand DNA molecules that interact with the messenger RNA that prevent translation of a positive gene. In this case, they downregulate the production of FB, which is a novel gene regulator of the alternative complement pathway.
Some genetic-association studies have shown involvement of the alternative complement pathway in GA. By targeting this pathway, the thinking is that the agent won’t encounter the interference of the normal complement system. Studies have shown that reducing FB reduces the instance of GA and upregulation of FB appears to increase GA. There’s an underlying rationale behind it.
Because most of these factors are produced in the liver, this is where FB-LRX works. It binds to messenger RNA FB, recruiting enzymes to degrade messenger RNA as well as the amount of FB in the systemic circulation.
 |
How does FB-LRX differ from existing therapies?
The administration is unique; it’s subcutaneous. While we’ve had subcutaneous injections previously, the subcutaneous route has an advantage in that it treats both eyes.
Where does the agent fit among the existing approved therapies?
We don’t have a treatment for GA at this moment. Several different modalities are looking at this. Apellis Pharmaceuticals seems furthest along with its complement factor 3 inhibitor (APL-2, pegcetacoplan) enrolling two Phase III trials. The C5 inhibitor avacincaptad pegol (Zimura, Iveric bio) is in a Phase IIb trial. The selective CD inhibitor lampalizumab (Genentech/Roche) failed.
There have been some investigative treatments that target inflammasomes, the inflammatory components of macrophages, to make the readjustment from active to inactive macrophages. However, without having a good animal model, developing a treatment for GA is very difficult. I think that’s the reason we’re unable to come up with an effective treatment at this time.
In addition to safety, what key finding of the Phase I trial will inform the next phase?
The trial showed a definite reduction in FB levels—a reduction of around 60 percent at 127 days. We know that the effect will probably last for a while, and it will reduce FB plasma levels, and that will reduce FB in the eye.
What are the primary and secondary endpoints of the Phase II trial?
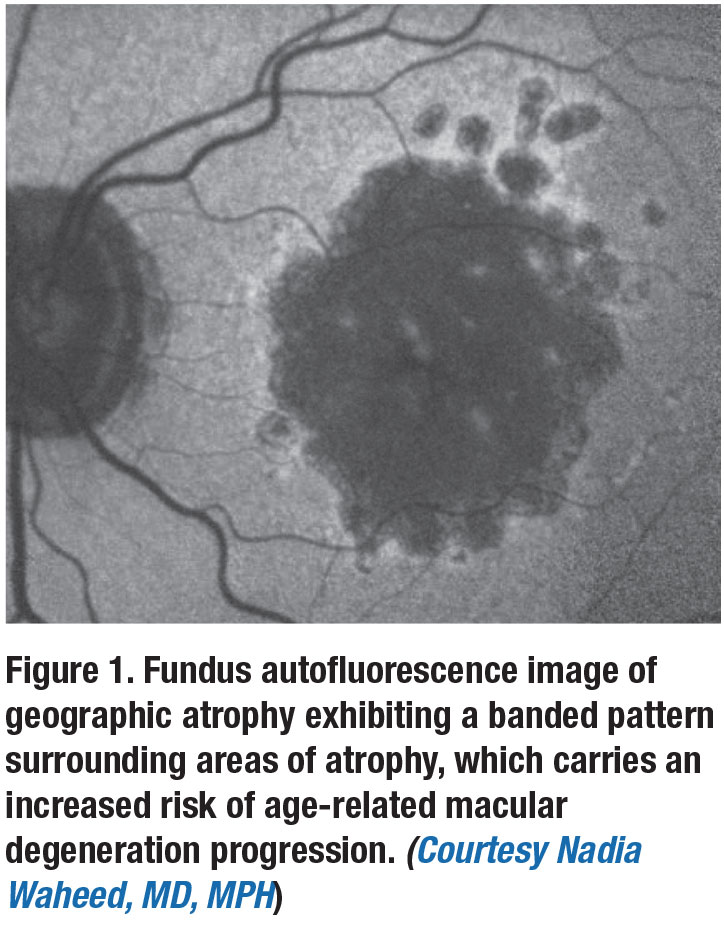
The primary endpoint is to evaluate the change of the area of GA as measured by fundus autofluorescence. The secondary endpoints are FB levels, the effect on low-luminance visual acuity as well as safety and tolerability of chronic administration. Low-luminance VA is becoming more important. Many people with GA have 20/20 vision, but they complain they can’t read anything; that they need more light.
Some sites are also using optical coherence tomography to investigate whether the choriocapillaris causes ischemia or becomes thinner during the disease process. RS
REFERENCE
1. Patel SS. Phase 1 results of a systemic antisense inhibitor of complement factor B for geographic atrophy. Paper presented at Angiogenesis, Exudation and Degeneration 2020; Miami, FL; February 8, 2020.



