 |
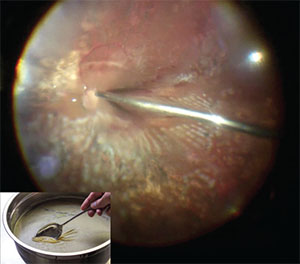
| Figure 1. The relative density of silicone oil creates an incomparable air-liquid interface. The essence of our technique is to significantly improve silicone oil extraction by removing the thin layer of oil that is gathering on the interface, like skimming fat from soup broth (inset). Inset image: Brandon Matzek/Kitchen Konfidence |
However, more recent reports have been published of significant visual deterioration following removal of silicone oil, and even of inexplicable and unanticipated sudden vision loss after uncomplicated silicone oil removal. Here, we describe the “soup-and-sandwich” technique we’ve used to remove silicone oil that may help avoid these vision-threatening complications.
Potential Consequences Of Silicone Oil
Over the past few decades, several studies have established the good intraocular safety profile of silicone oil in vitreoretinal surgery while rarely reporting toxic effects to the human retina.2-5 Only a small number of papers have brought to light concerns over potential harmful consequences of silicone oil on animal retinal structures, particularly in longstanding use.6-7 However, secondary anterior-segment complications to intraocular silicone oil, such as glaucoma, keratopathy and cataract, are well recognized.8
Since it can adversely affect nearly all ocular structures, silicone oil emulsification is a clinically serious complication. Moreover, in the emulsified state, silicone oil may not provide an optimal internal tamponade across the retinal surface. The duration of silicone oil in the eye, mainly after one year, seems to influence the propensity for emulsification.9 For these reasons, expert retinal surgeons recommend removing the silicone oil when successful reattachment is accomplished and the retinal status appears to be clinically stable. The optimal timing remains controversial, usually ranging from three to 12 months.
The Pan American Collaborative Retina Study described significant visual deterioration following removal of silicone oil mostly secondary to retinal re-detachment, proliferative vitreoretinopathy and vitreous hemorrhage from proliferative diabetic retinopathy.10 Other reports have emerged of inexplicable and unanticipated sudden vision loss after uncomplicated removal of silicone oil.11-15 The published cases were originally fovea-sparing retinal detachment that remained attached during the entire surgery. These reports documented good visual acuity in these patients following initial vitrectomy and prior to oil extraction. None suffered from re-detachment, proliferative vitreoretinopathy, macular edema or epiretinal membrane.
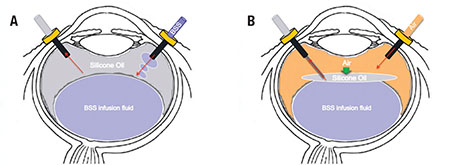 |
| Figure 2. Employing a standard three-port pars plana approach, the silicone oil is aspirated actively using a 23-gauge automated viscous extraction device while infusing basic salt solution (BSS) (A). Then an air-fluid exchange using a back-flush cannula is performed (B). The air injected pushes back the silicone oil toward the posterior pole, sandwiching it between the air and the BSS. The tip of the back-flush cannula is maintained at the level of the air-fluid interface where the surgeon can see a thin film of silicone oil. |
This phenomenon has implications for vitreoretinal specialists and leads one to consider what needs to be done to avoid it. Surely, one must take special care to ensure a silicone oil evacuation that is as complete as possible, but this can sometimes be challenging. In fact, when infusing basic salt solution (BSS) in the vitreous cavity, the silicone oil floats anteriorly and has a tendency to gather in the periphery, out of the range of the wide-angle viewing system.
Our silicone oil removal technique takes advantage of its physical properties. With the specific gravity of 0.97, silicone oil is lighter than BSS but heavier than air. This creates an incomparable air-liquid interface that allows the vitreoretinal surgeon to significantly improve silicone oil extraction by skimming away a thin layer of oil collecting on this interface, much like skimming the fat off of soup stock (Figure 1).
Surgical Technique
For our technique, we employ a standard three-port pars plana approach using a wide-angle viewing system. The silicone oil is aspirated actively using a 23-gauge automated viscous extraction device (Alcon Constellation) while infusing BSS (Figure 2A). The vitrectomy machine is set with a vacuum rate at 650 mmHg and with an intraocular pressure at 25 mmHg.
To improve the removal of silicone oil from the vitreous cavity, we preform an air-fluid exchange using a back-flush cannula. With the patient in the supine position, the air injected pushes back the silicone oil toward the posterior pole, sandwiching it between the air and the BSS (Figure 2B). This method is also handy in the presence of confined emulsified silicone oil droplets in the retro-iris plane.
To remove the oil overlay gathering on the interface, it is essential to place the tip of the back-flush cannula at the level of the air-fluid interface where a thin film of silicone oil can be observed.
Once the air-fluid exchange is taken down to the optic nerve, the vitreous cavity is partially infused with BSS. This essentially rinses the retinal surface of residual silicone oil that re-accumulates as BSS fluid refills the vitreous cavity. Be cautious during this step to re-infuse BSS at a low flow rate to avoid the stream of infusing BSS from creating an iatrogenic retinal break. The remaining air acts as a barrier by precluding the residual oil from traveling anteriorly again. In a similar manner, multiple sequential air-fluid exchanges are completed until all the oil has been skimmed off.
| To watch Drs. Trussart, Mark and Efrem Mandelcorn and Devenyi describe the 'soup and sandwich' technique for removal of silicone oil, click here. |
This silicone “soup-and-sandwich” skimming technique results in improved and more complete silicone oil removal. RS
Dr. Trussart is a vitreoretinal surgery fellow at the University of Toronto. Drs. Mark Mandelcorn, Ephrem Mandelcorn and Devenyi are attending vitreoretinal surgeons at the Toronto Western Hospital, Donald K. Johnson Eye Institute, University of Toronto.
DISCLOSURES: The authors have no relevant disclosures.
REFERENCES
1. Gonvers M. Temporary silicone oil tamponade in the management of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol.1985;100:239–245.
2. Inoue M, Iriyama A, Kadonosono K, Tamaki Y, Yanagi Y. Effects of perfluorocarbon liquids and silicone oil on human retinal pigment epithelial cells and retinal ganglion cells. Retina. 2009;29:677–681.
3. Lucke KH, Foerster MH, Laqua H. Long-term results of vitrectomy and silicone oil in 500 cases of complicated retinal detachments. Am J Ophthalmol. 1987;104:624–633.
4. Leaver PK. Vitrectomy and fluid/silicone oil exchange for giant retinal tears: 10 years follow up. Ger J Ophthalmol. 1993;2:20 –30.
5. Mandelcorn E, Howarth D, Mandelcorn M. Silicone oil-induced bilateral granulomatous uveitis. Can J Ophthalmol. 2010;45: 288-289.
6. Pastor JC, Lopez MI, Saornil MA, Refojo MF. Intravitreal silicone and fluorosilicone oils: pathologic findings in rabbit eyes. Acta Ophthalmol (Copenh). 1992;70:651–658.
7. Papp A, Kiss EB, Timar O, et al. Long-term exposure of the rabbit eye to silicone oil causes optic nerve atrophy. Brain Res Bull. 2007;74:130–133.
8. Patel AV, Papakostas TD, Elliot D. Silicone oil emulsification in retina surgery. Retina Today. 2015;6:29-32.
9. Barca F, Caporossi T, Rizzo S. Silicone oil: Different physical proprieties and clinical applications. BioMed Res Int. 2014;502143; epub 2014 June 11.
10. Alpizar-Alvarez N, Wu L, Roca JA, et al. Unexplained visual loss following silicone oil removal. Results of the Pan American Collaborative Retina Study (PACORES) Group. Invest Ophthalmol Vis Sci. 2014;55:2335.
11. Moya R, Chandra A, Banerjee PJ, Tsouris D, Ahmad N, Charteris DG. The incidence of unexplained visual loss following removal of silicone oil. Eye. 2015;29:1477–1482.
12. Shalchi Z, Mahroo OA, Shunmugam M, Mohamed M, Sullivan PM, Williamson TH. Spectral domain optical coherence tomography findings in long-term silicone oil-related visual loss. Retina. 2015;35:555–563.
13. Scheerlinck LM, Schellekens PA, Liem AT, Steijns D, Leeuwen Rv. Incidence, risk factors, and clinical characteristics of unexplained visual loss after intraocular silicone oil for macula-on retinal detachment. Retina. 2016;36:342-350.
14. Newsom RSB, Johnston R, Sullivan PM, Aylward GB, Holder GE, Gregor ZJ. Sudden visual loss after removal of silicone oil. Retina 2004;24:871–877.
15. Cazabon S, Groenewald C, Pearce IA, Wong D. Visual loss following removal of intraocular silicone oil. Br J Ophthalmol. 2005;89:799–802.
16. Dogramaci M, Williams K, Lee E, Williamson TH. Foveal light exposure is increased at the time of removal of silicone oil with the potential for phototoxicity. Graefes Arch Clin Exp Ophthalmol. 2013;251:35–39.
17. Winter M, Eberhardt W, Scholz C, Reichenbach A. Failure of potassium siphoning by Muller cells: a new hypothesis of perfluorocarbon liquid-induced retinopathy. Invest Ophthalmol Vis Sci. 2000;41:256–261.
18. Asaria RHY, Kon CH, Bunce C, et al. Silicone oil concentrates fibrogenic growth factors in the retro-oil fluid. Br J Ophthalmol. 2004;88:1439–1442.




