 |
 |
When navigated laser therapy for retinal disorders first emerged more than a decade ago, it had the potential to eliminate a potentially fallible human element—the retina specialist manually applying laser spots—and replace it with a computer assist to target the laser pulses more precisely to where they were needed. The concept was to combine diagnostic imaging and laser therapy in one system, which gave rise to the Navilas navigated retina laser (OD-OS), approved for U.S. use in 2015.
However, as with any new technology, navigated laser photocoagulation hasn’t been without controversy. We have authored multiple publications on laser photocoagulation—in a few cases as coauthors. Here, we take opposite sides of the argument that navigated laser has great potential as a treatment for diabetic macular edema.
PREMISE: Patterns (grids) in laser photocoagulation are beneficial.
Pro, Dr. Chhablani: Pattern laser helps to administer the laser patterns to achieve the therapeutic effect (as in macular laser), as well as to enhance the speed (as in peripheral laser). With Navilas, you have the option to accurately plan the treatment with each single spot if needed.
In some cases they might be forming a “grid” for quick application, making an optimal fit to the pathology. With Navilas, spacing between the laser spots can be modified, or even reduced, to overlapping spots to achieve therapeutic effect.
Con, Dr. Luttrull: Patterns—grids, originally—were used to allow photocoagulation of broad areas of retina while preserving enough function to prevent profound visual loss. Modern retinal laser therapy (MRT) instead improves retinal and visual function directly where it’s applied and faces no such constraint.
MRT directly treats all dysfunctional retina confluently to maximize the clinical benefits. Patterns (low-density treatment) thus, at worst, result in under-treatment and, at best, serve no useful purpose.
PREMISE: Differently shaped and sized patterns offer advantages.
Pro, Dr. Chhablani: Preplanned patterns for macular and peripheral lasers help to administer preferred laser patterns for specific lesions, such as grid, lattice degeneration, retinal holes and panretinal photocoagulation. Patterns could be made as the spacing, numbers and shape require.
So, with a single foot press you get what you planned. For DME, this allows for planning different-sized laser spots (for example, smaller burns for microaneurysms close to the fovea) and patterns for optical coherence tomography-thickness map-guided laser to the area of edema.
Con, Dr. Luttrull: Virtually every current laser platform offers pattern-scanning modes. All offer preset patterns of various shapes and sizes. Some allow the creation of customized patterns. Different pattern sizes and shapes imply a perceived utility to localized treatment. However, focal and local treatments are artifacts of the photocoagulation era required to limit retinal damage and visual loss, and MRT doesn’t employ them.
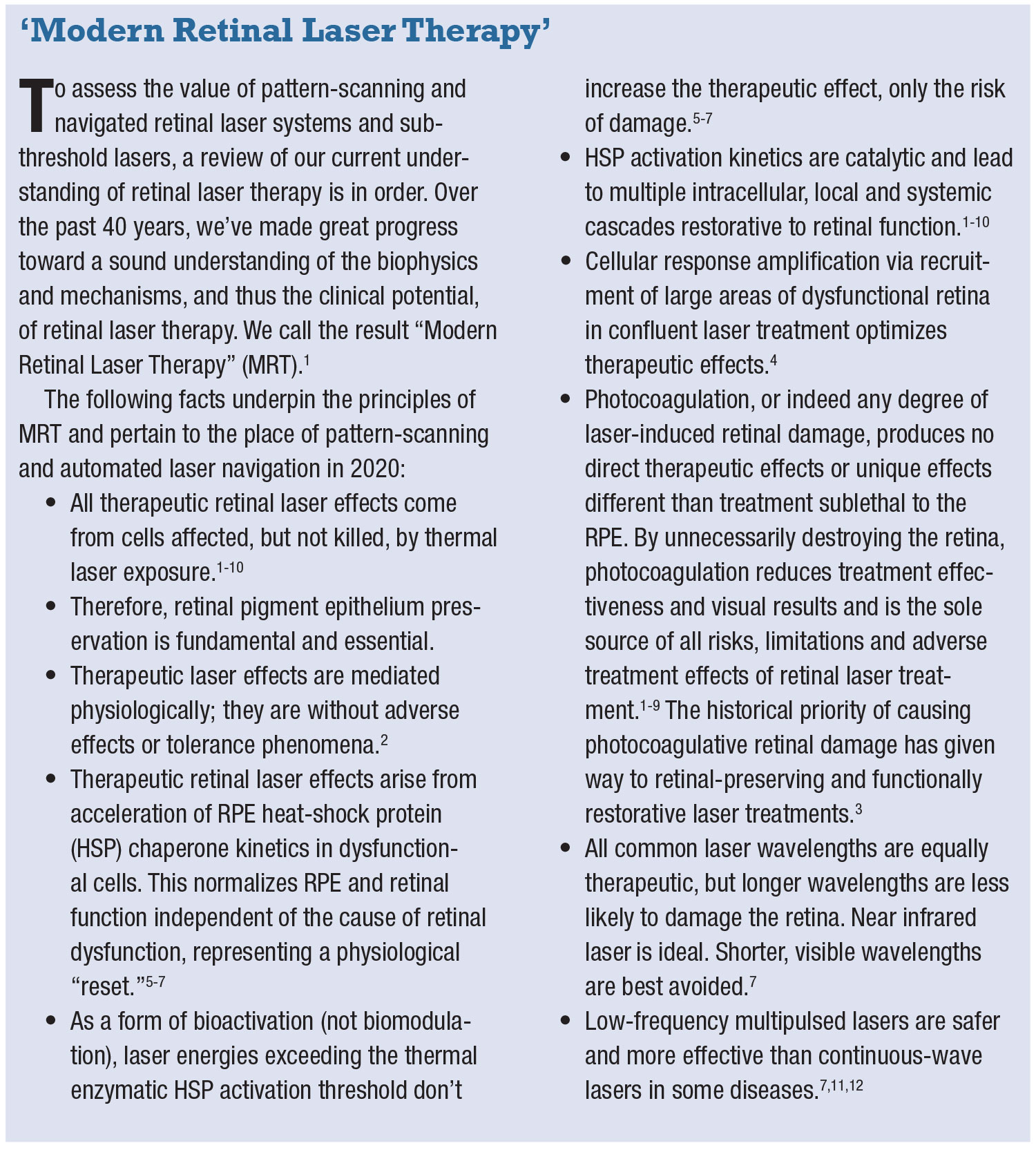
As noted, MRT improves retinal function directly where it’s applied. Further, DME is a local manifestation of a panretinal (and indeed systemic) disease, the tip of the iceberg. Thus, DME treatment should extend well beyond the DME itself; panmacular treatment at minimum, preferably the entire retina, is ideal, much the same as drug treatment (Figure 1, page 24). Use of variously shaped patterns results in undertreatment and suboptimal results. It’s a retinopathy. Treat it. All of it.
 |
 |
PREMISE: Pattern scanning speeds treatment.
Pro, Dr. Chhablani: I find it very useful, especially in the periphery, as the laser could be very difficult for peripheral lesions. Few patterns hasten the laser process. Yes, preplanning helps to minimize the time of the treatment.
Con, Dr. Luttrull: As a practitioner of MRT, I use identical laser parameters and treatment fields for every eye and every macular indication, including DME (panmacular low-intensity/high-density subthreshold diode micropulse laser, or “SDM”). So, no fiddling with the machine. I just put my foot down on the pedal in the fastest repeat mode and don’t lift it until I’m done. Thus, I finish treatment before the typical navigated and/or pattern-scanning user has even planned treatment and prepared their machine.
PREMISE: Documentation of treated areas is important.
Pro, Dr. Chhablani: Documentation is especially important when working with subthreshold laser treatment. In this treatment, the endpoint of the laser isn’t visible on ophthalmoscopy. However, a communication on “what has been done” isn’t possible (or only based on sketches, which can be inaccurate and often incomplete).
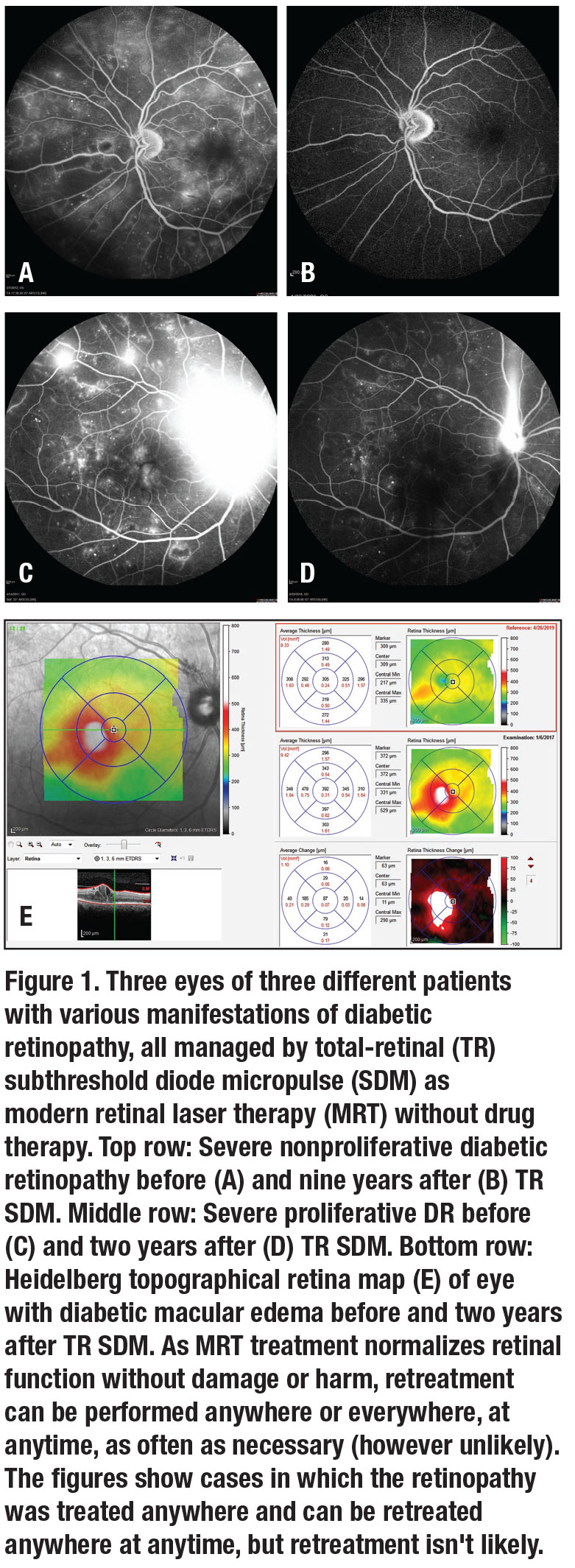
A high risk in subthreshold laser treatment is undertreatment because not enough “area” has been treated, and documentation can help in determining if undertreatment is the cause for no improvement or if the case is simply nonresponsive and other treatment should be considered. In a case of recurrence or poor response, detailed documentation of previous laser treatment helps to plan further treatment. Few providers believe in confluent grid covering the full macular area; however, imaging helps define the “diseased” area. Therefore, I treat only the diseased area with detailed documentation and transparency (Figure 2).
 |
Con, Dr. Luttrull: As identifiable MRT lesions are absent (like drug therapy), some laser platforms offer virtual documentation of treatment placement. The implication is that retreatment of a given area is undesirable, or that one needs evidence beyond the therapeutic effect of treatment having been done. The former is obviously relevant only to photocoagulation, which needs no virtual documentation. The latter has never been a concern with drug therapy. As MRT is reliably sublethal to the retina, MRT, like drug therapy, can be repeated infinitely anywhere in the retina, including previously treated areas. There’s no reason to know where you’ve been; only what you want to do next (Figure 1).
PREMISE: Focal/laser application improves accuracy.
Pro, Dr. Chhablani: Publications have shown that precise treatment with Navilas helps to improve accuracy and safety.13 Computerized preplanning allows a precise plan using multimodal imaging before execution. Marked caution zones prevent inadvertent damage to the fovea/optic nerve. Preplanning and live visualization of the laser process allows supervision, which, again, helps to avoid any complication and improves safety.
Con, Dr. Luttrull: Focal/local treatment epitomizes the photocoagulation era. MRT defines photocoagulation as a complication of treatment, and thus a contraindication. Thus, abandoning focal photocoagulation treatment is the best way to improve safety. Once done, pinpoint accuracy is irrelevant. When was the last time you aimed the needle at the DME? MRT, which is sublethal to the RPE and already clinically harmless, isn’t made safer or more effective by programmed and limited placement.
PREMISE: Pattern scanning/navigation reduces treatment time.
Pro, Dr. Chhablani: Pattern scanning/navigation for continuous wave reduces treatment time with increased comfort to the patient as well as reduces re-treatment rate.14-17 Subthreshold lasers are painless and faster.
Con, Dr. Luttrull: It’s shortening continuous-wave photocoagulation spot duration and intensity that reduces pain, not aiming or patterning. However, it also reduces efficacy. MRT is already painless. RS
 |
REFERENCES
1. Luttrull JK, Kent D. Modern retinal laser for neuroprotection in open-angle glaucoma. In: Samples JR, Ahmed IIK, eds. New Concepts in Glaucoma Surgery, Vol. 1. Amsterdam; Kugler Publications; 2019. In press.
2. Luttrull JK, Chang DB, Margolis BWL, Dorin G, Luttrull DK. Laser re-sensitization of medically unresponsive neovascular age-related macular degeneration: Efficacy and implications. Retina. 2015; 35:1184-1194.
3. Chhablani J, Roh YJ, Jobling AI, et al. Restorative retinal laser therapy: Present state and future directions. Surv Ophthalmol. 2018;63:307-328.
4. Luttrull JK, Dorin G. Subthreshold diode micropulse laser photocoagulation (SDM) as invisible retinal phototherapy for diabetic macular edema: A review. Curr Diabetes Rev. 2012;8:274-284.
5. Kregel K. Heat shock proteins: Modifying factors in physiological stress responses and acquired thermotolerance. J Appl Physiol. 2002;92:2177-2186.
6. Inagaki K, Shuo T, Katakura K, Ebugara Bm Nyrajanu Am Igjisgu J. Sublethal photothermal stimulation with a micropulse laser induces heat shock protein expression in arpe-19 cells. J Ophthalmol. Published online November 30, 2015.
7. Chang DB, Luttrull JK. Comparison of subthreshold 577nm and 810nm micropulse laser effects on heat-shock protein activation kinetics: Implications for treatment efficacy and safety. Translational Vis Sci Technol. In press.
8. Midena E, Bini S, Martini F, Enrica C, et al. Changes of aqueous humor Müller cells’ biomarkers in human patients affected by diabetic macular edema after subthreshold micropulse laser treatment. Retina. 2020;40:126-134.
9. Caballero S, Kent DL, Sengupta N, et al. Bone marrow-derived cell recruitment to the neurosensory retina and retinal pigment epithelial cell layer following subthreshold retinal phototherapy. Invest Ophthalmol Vis Sci. 2017;58:5164-5176.
10. De Cilla S, Vezzola D, Farruggio S, et al. The subthreshold micropulse laser treatment of the retina restores the oxidant/antioxidant balance and counteracts programmed forms of cell death in the mice eyes. Acta Ophthalmol. 2019:97:e559-e567.
11. Chhablani J, Alshareef R, Kim DT, Narayanan R, Goud A, Mathai A. Comparison of different settings for yellow subthreshold laser treatment in diabetic macular edema. BMC Ophthalmol. 2018;18:168.
12. Vujosevic S, Martini F, Longhin E, Convento E, Cavarzeran F, Midena E. Subthreshold micropulse yellow laser versus subthreshold micropulse infrared laser in center-involving diabetic macular edema: Morphologic and functional safety. Retina. 2015;35:1594-1603
13. Kozak I, Oster SF, Cortes MA, et al. Clinical evaluation and treatment accuracy in diabetic macular edema using navigated laser photocoagulator NAVILAS. Ophthalmology. 2011;118:1119-1124.
14. Chhablani J, Mathai A, Rani P, Gupta V, Arevalo JF, Kozak I. Comparison of conventional pattern and novel navigated panretinal photocoagulation in proliferative diabetic retinopathy. Invest Ophthalmol Vis Sci. 2014;55:3432-3438.
15. Kernt M, Cheuteu RE, Cserhati S, et al. Pain and accuracy of focal laser treatment for diabetic macular edema using a retinal navigated laser (Navilas). Clin Ophthalmol. 2012;6:289-296.
16. Neubauer AS, Langer J, Liegl R, et al. Navigated macular laser decreases retreatment rate for diabetic macular edema: a comparison with conventional macular laser. Clin Ophthalmol. 2013;7:121-128.
17. Ober MD, Kernt M, Cortes MA, Kozak I. Time required for navigated macular laser photocoagulation treatment with the Navilas. Graefes Arch Clin Exp Ophthalmol. 2013;251:1049-1053.



