 |
Bios Dr. Patel is a retina fellow with Associated Retina Consultants of Arizona. Dr. Hahn is a partner at New Jersey Retina in Teaneck. DISCLOSURES: Dr. Reddy is a consultant to Allergan/AbbVie, Regeneron Pharmaceuticals, Alimera Sciences, Bausch + Lomb and Dr. Patel has no relevant relationships to disclose. Dr. Hahn is a consultant to DORC. |
Subretinal proliferation is a well-known component of proliferative vitreoretinopathy and has been reported to occur in 15 to 47 percent of eyes with a retinal detachment.1-4 The vast majority of subretinal proliferation occurs in the form of diffuse sheets underneath the retina and is mainly composed of glial tissue. Due to a relative lack of collagen in glial cells, this sheet of tissue rarely contracts and seldom prevents retinal reattachment during surgery.5
In contrast, subretinal bands have been shown to contain differentiated pigment epithelial cells that contain myo-
fibroblasts.2 These cells initially grow as membranes beneath the retinal surface. With expansion under the contractile force of the myofibroblasts, breaks eventually occur in these membranes, leading to the formation of branching subretinal bands.5 These bands can create a contractile force on the retina, preventing retinal reattachment during surgery.6
|
|
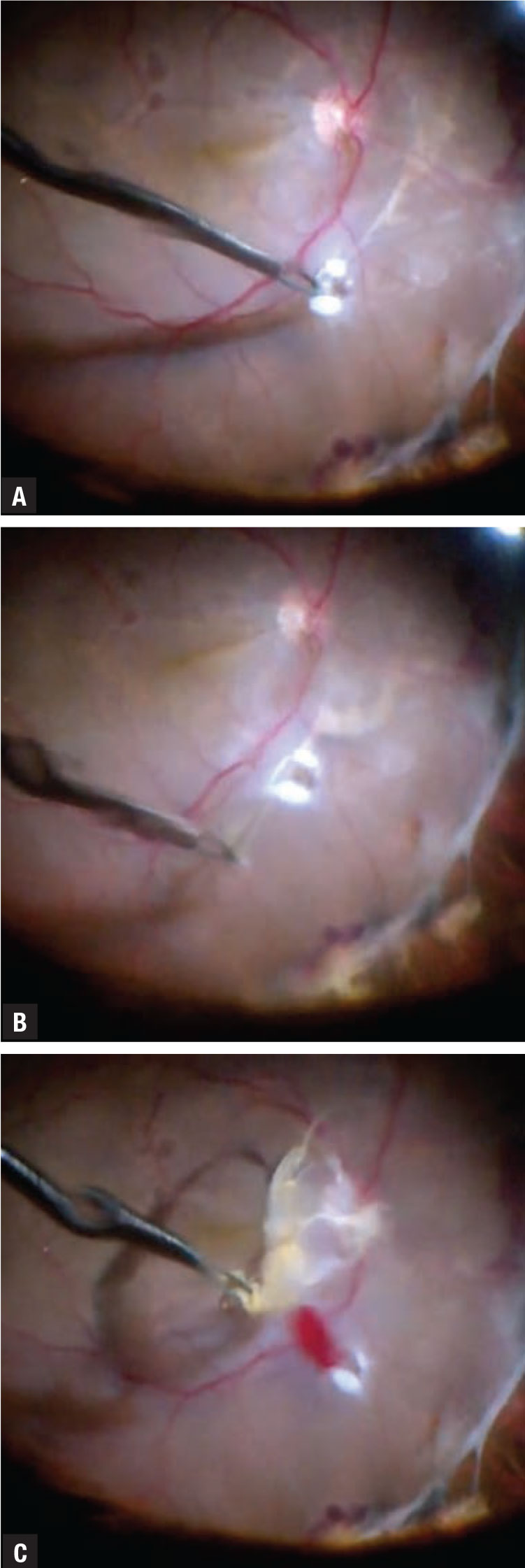
A) Subretinal band being grasped with forceps after the creation of an access retinotomy. The retinotomy was created with endocautery in an area where the band is thick and allows for good manipulation. B) The band is pulled tangentially 180 degrees away from the side of greatest adherence to avoid enlarging the retinotomy site. C) The subretinal band has been removed in one piece. Notice that the retinotomy site has largely retained its initial size thanks to maneuvers we discussed. |
Dealing with taut bands
In 13 to 28 percent of patients with subretinal bands, the retina remains taut despite appropriate maneuvers, requiring the bands to be excised to achieve proper anatomical success.6-7 Once you decide intraoperatively to remove the subretinal membranes, several techniques can ease the process.
First, if the subretinal band is adjacent to a preexisting retinal break, a retinotomy might not be required. With the use of a pic, a loop of the subretinal band can be brought through the existing retinal break and removed with intraocular forceps.7
However, if a retinotomy is needed to get access to the band, it should be made in a location that maximizes this access. To allow greater leverage on the band, the retinotomy needs to be made at a site where the band is thickest and the angle at which the forceps enter the subretinal space should be considered.
Take care to ensure the band itself isn’t severed during the creation of the retinotomy because the contractile force will cause the band to retract, which will prevent proper removal. Placing the retinotomy slightly adjacent to the band rather than directly over it will reduce the risk of making this crucial error.
Ways to remove the band
Once the subretinal space has been accessed, the band can be removed in several ways. One way is to grasp the band with serrated intraocular forceps and pull it tangential to the retina to avoid enlarging the retinotomy or causing further damage.8
Alternatively, swiveling the forceps to wrap the band around them or using chandelier illumination and a hand-over-hand technique with two forceps have also been shown to be successful.7
If the band is strongly attached to the underlying retinal pigment epithelium, preventing proper removal, cutting the band in several places to release the traction can provide enough flexibility to allow for reattachment.7
Rarely, if a diffuse sheet of subretinal proliferation requires removal, it may become prudent to make an extensive peripheral retinotomy and turn the retina over to grasp the tissue under direct visualization.8
Bottom line
The anatomical success in cases that require subretinal band removal matches that of PVR cases that require no SRM removal. While it’s rare to have subretinal bands that require removal, a proper understanding of the pathophysiology combined with the appropriate technique can help ensure surgical success and ease the removal of subretinal bands. RS
REFERENCES
1. Lean JS, Stern WH, Irvine AR, Azen SP. Classification of proliferative vitreoretinopathy used in the silicone study. The Silicone Study Group. Ophthalmology. 1989;96: 765-771.
2. Tabandeh H, Callejo SA, Rosa RH Jr, Flynn HW Jr. Subretinal “napkin-ring’ membrane in proliferative vitreoretinopathy. Arch Ophthalmol. 2000;118: 1287-1289.
3. Wallyn RH, Hilton GF. Subretinal fibrosis in retinal detachment. Arch Ophthalmol. 1979;97:2128-2129.
4. Kothari N, Kuriyan AE, and Harry W. Flynn Jr. Spectral domain optical coherence tomography imaging of subretinal bands associated with chronic retinal detachments. Clin Ophthalmol. 2016;10: 467-470.
5. Sternberg PJ, Machemer R. Subretinal proliferation. Am J Ophthalmol. 1984;98:456-462.
6. Hiscott P, Grierson I. Subretinal membranes of proliferative vitreoretinopathy. Br J Ophthalmol. 1991;75:53.
7. Lewis H, Aaberg TM, Abrams GW, McDonald HR, Williams GA, Mieler WF. Subretinal membranes in proliferative vitreoretinopathy. Ophthalmology. 1989;96:1403-1415.
8. Kimura M, Nishimura A, Saito Y, Ikeda H, Sugiyama K. Retinotomy with retinal turnover to remove subretinal membranes under direct visualization for proliferative vitreoretinopathy. Clin Ophthalmol. 2012;6:781-788.




