 |
Optic pit maculopathy can be surgically challenging and has variable outcomes. While many cases may resolve spontaneously, others persist and may be amenable to a variety of approaches. Here, we describe our approach after failed initial vitrectomy with internal limiting membrane peeling to improve the macular fluid associated with the optic pit.
Specifically, we use a flap of internal limiting membrane to “plug” the pit,1 using perfluorocarbon liquid to displace macular fluid while making a small
retinotomy for draining submacular fluid. We also apply endolaser
to barricade the subretinal space between the pit and outer
macula.
Surgical technique
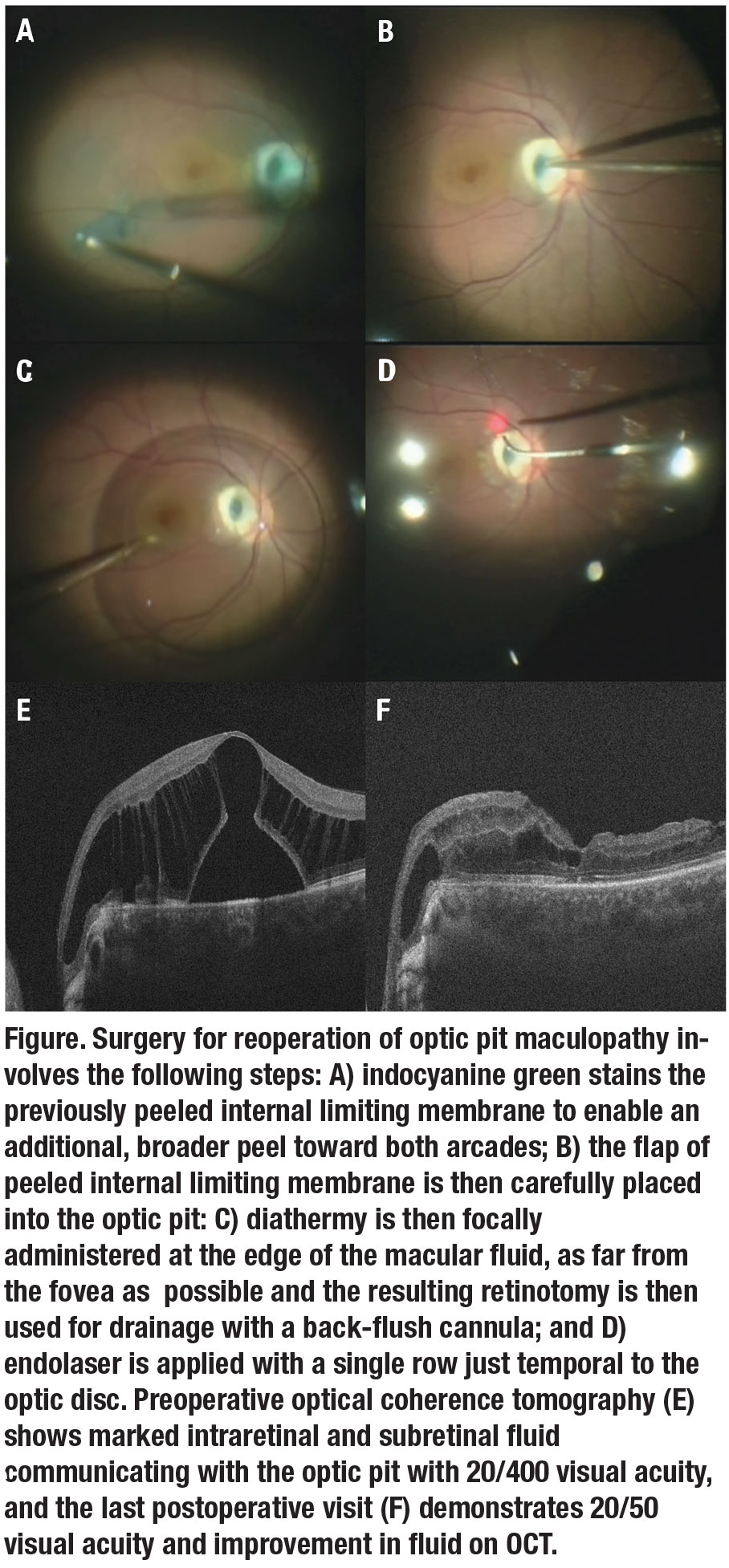
We prefer smaller-gauge vitrectomy (25- or even 27-ga) in these cases. We inject indocyanine green dye to stain the remaining ILM, which we then peel toward both arcades (Figure A). Carefully and gently, we place the subsequent ILM flap into the optic pit (Figure B). Any vitreous plug or remnants within the optic pit should first be removed, which can often be observed with preoperative optical coherence tomographic imaging.2
An injection of PFCL near the optic nerve displaces the macular fluid. A side-flow cannula avoids sudden pressure fluctuations, and the tip of the cannula should always stay within the bubble. PFCL is injected until it reaches the anterior-most fluid in the macula.
A small retinotomy on the edge of the macular fluid collection is created with diathermy (Figure C). A backflush cannula drains the subretinal fluid through the retinotomy, first with active and then passive aspiration. A partial air-fluid exchange removes infusion fluid but maintains the PFCL bubble for ongoing displacement of residual papillomacular fluid.
Application of endolaser creates a retinopexy 180 degrees temporally around the optic nerve in a single row (Figure D), as well as around the retinotomy. The residual PFCL is removed with additional and complete air-fluid exchange. Finally, 15% C3F8 gas is then exchanged.
We instructed this patient to remain face-down for one week. By six months, vision improved from 20/400 preoperatively (Figure E) to 20/50 with a marked decrease in macular fluid at the last postoperative exam (Figure F).
 |
Bottom line
Optic pit maculopathy is poorly understood and the best surgical approach isn’t well-defined. In cases of optic pit maculopathy refractory to initial vitrectomy, a combination of various approaches, including plugging the pit, draining subretinal fluid, temporal peripapillary endolaser, long-acting gas and face-down positioning, may increase the chances of success. RS
REFERENCES
1. Ravani R, Kumar A, Karthikeya R, et al. Comparison of inverted ILM-stuffing technique and ILM peeling alone for optic disc pit-associated maculopathy: Long-term results. Ophthalm Surg Lasers Imag Retina. 2018; 49:e226-e232.
2. Gregory-Roberts EM, Mateo C, Corcostegui B, et al. Optic disk pit morphology and retinal detachment: optical coherence tomography with intraoperative correlation. Retina. 2013; 33:363-370.




