 |
Bio Dr. González is a vitreoretinal surgeon and currently a second-year ocular oncology fellow at Princess Margaret Hospital, Toronto. |
We sometimes need to perform choroidal tumor biopsy for either diagnostic or prognostic purposes, or both. With the recent advances in tumor molecular genetics, there has been a significant increase in prognostic tumor biopsies.
A variety of techniques exist for obtaining choroidal tissue depending on the size, location and accessibility of the tumor. Transretinal biopsy is recommended for posterior tumors or tumors smaller than 2 mm. This technique can be performed using indirect ophthalmoscopy or with a microscope-assisted wide-angle viewing system and chandelier illumination.1 The latter can improve visualization, simplify the procedure and potentially result in a shorter and safer learning curve. Here, we share some tips that can increase the chances of performing a successful transretinal biopsy.
Preoperative strategies
Review the key tumor measurements. Come to the operating room prepared with a diagram of the tumor and its overall dimensions.
Know your element. Verify in advance the media most appropriate for the tissue sample and whether you should contact a cytology team member for specimen collection.
Intraoperative strategies
Lights on. Identify an appropriate clock hour for chandelier placement to maximize illumination.
Needle entry. Under the microscope, identify the biopsy site and determine the approach angle. In our experience, an approach that’s opposite the biopsy target works best. After passing through the retina into the tumor, a gentle back-and-forth motion will help to dislodge more tumor cells.
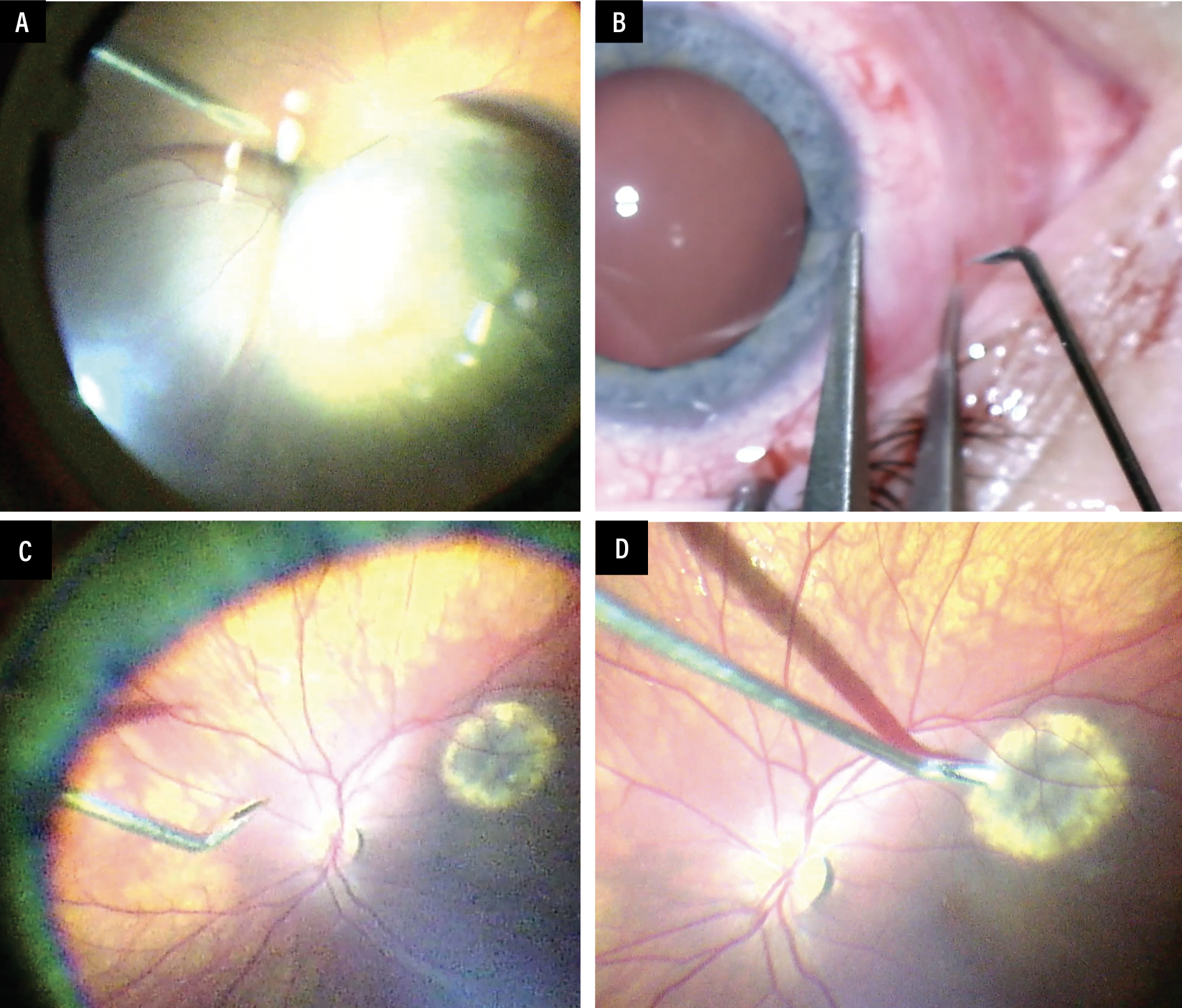 |
| A) A straight needle enters directed toward the apex of a choroidal melanoma. B to D) The approach for a transretinal fine-needle aspiration biopsy in a tumor with a less than 2-mm thickness. In these cases, the needle is bent and a tangential incision is performed. |
Aspiration. Stop suction before withdrawing the needle from the tumor.
Needle exit. Steady the needle while exiting the tumor as the sharp side of the needle can cut into the retina.
Don’t panic. Hemorrhage can occur in some cases, but it’s commonly self-limiting. Raising the intraocular pressure with a cotton-tip applicator may be helpful in controlling the hemorrhage.
Finishing touches. Once you withdraw the needle through the sclera, use a cotton-tip applicator and directly apply pressure followed by cryotherapy at the exit site.
Becoming familiar with the different types of biopsy techniques will improve the chances of safely obtaining an adequate sample for testing. RS
REFERENCE
1. Venkatesh P, Kashyap S, Temkar S, Gogia V, Garg G, Bafna RK. Endoillumination (chandelier) and wide-angle viewing-assisted fine-needle aspiration biopsy of intraocular mass lesions. Indian J Ophthalmol. 2018;66:845-847.




