 |
Bios The authors are with the department of ophthalmology, Duke University Hospital, Durham, North Carolina. Dr. Hahn is a vitreoretinal specialist at NJ Retina in Teaneck. DISCLOSURES: The authors have no relevant disclosures. Dr. Hahn has no relevant disclosures. |
 |
|
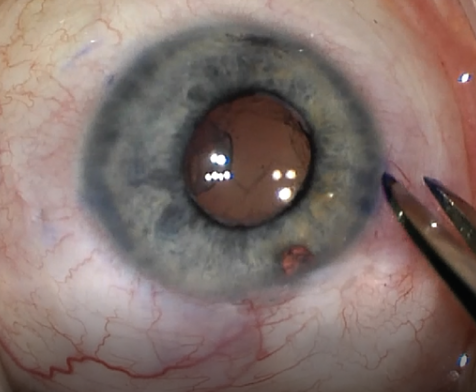
Figure 1. This patient with nanophthalmos and a prior trabeculectomy required placement of ports at 2.5 mm and in a location to avoid the trabeculectomy bleb. |
Aqueous misdirection, also known as malignant glaucoma, is an uncommon type of secondary angle- closure glaucoma that can require vitreosurgical management.1 The pathophysiology is believed to be secondary to misdirection of aqueous fluid, resulting in hydration of the vitreous body. The vitreous hydration causes anterior rotation of the ciliary body with forward displacement of the iris and lens, and subsequent shallowing of the anterior chamber.
Patients with aqueous misdirection present with a shallow anterior chamber and high intraocular pressure. The differential diagnosis includes pupillary block, choroidal detachment, suprachoroidal hemorrhage or over-filtration from a filtering bleb. To rule out pupillary block, patients must have a patent iridotomy or iridectomy. B-scan ultrasonography and ultrasound biomicroscopy can also aid in evaluating the differential diagnoses.
Malignant glaucoma treatments
The initial medical treatment for aqueous misdirection uses cycloplegics and pressure-lowering eyedrops. Acetazolamide and hyperosmotic agents such as mannitol can also be initiated. Medical treatment is successful in about 50 percent of cases.
But when medical treatment doesn’t work, a Nd:YAG laser anterior hyaloid-otomy can be attempted. However, in treatment-resistant cases, a pars plana vitrectomy with irido-zonulo-hyaloidectomy (PPV-IZH) may be required to reverse the flow of aqueous humor.1,2 The PPV removes the pathologically hydrated vitreous, and the IZH ensures communication between the anterior chamber and vitreous cavity.
Performing PPV-IZH-PPV
These are the key components of PPV-IZH to consider:
1. Port placement. Many patients with aqueous misdirection will have concurrent medical conditions that require thoughtful port placement (Figure 1). Hyperopia is a known risk factor, and patients may be nanophthalmic. As a result, the standard 3-to-4-mm port placement may result in iatrogenic retinal breaks. Transillumination can help to better evaluate the pars plana location. Further, a previous trabeculectomy or a glaucoma drainage device requires careful port placement that accounts for the location of the filtering blebs.
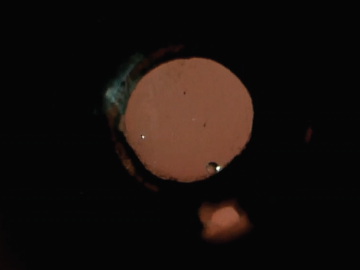 |
| Figure 2. Retroillumination demonstrates no vitreous debris or intraocular lens haptic blocking the irido-zonulo-hyaloidectomy passage. |
2. Anterior/core vs. complete PPV. A recent systematic review evaluated anterior/core vitrectomy vs. complete PPV and found a higher rate of relapse in the anterior/core vitrectomy cases.1 The primary goal of vitrectomy is to disrupt the anterior hyaloid face. However, fluid may continue to fill vitreous cisterns if a complete PPV isn’t performed. Also, residual vitreous in the periphery may block the communication the IZH creates, so careful vitreous shave of the vitreous base should be performed underneath the IZH.
3. Synechiolysis. If the aqueous misdirection has been present for years, then prolonged iridotrabecular contact can result in significant synechiae, which can cause chronic angle closure. This can also result in patients still needing IOP-lowering drops after the procedure. PPV-IZH should be considered earlier to prevent these complications. Additionally, the release of both posterior synechiae and combination surgery with a glaucoma colleague for goniosynechiolysis may be required.
4. Retroillumination. Frequently, blockage of the IZH opening by residual vitreous, inflammatory membranes or the haptic of an intraocular lens can cause relapse of aqueous misdirection. Retroillumination (Figure 2) using the light pipe can evaluate for residual material blocking the IZH. RS
REFERENCES
1. Schmidt DC, Kessel L, Pedersen KB, Villumsen JE, Bach-Holm D. Pars plana vitrectomy combined with hyaloido-zonula-iridectomy in treatment of patients with chronic aqueous misdirection: A systematic literature review and case series. Acta Ophthalmol. 2021;99:251-259.
2. Bitrian E, Caprioli J. Pars plana anterior vitrectomy, hyaloido-zonulectomy, and iridectomy for aqueous humor misdirection. Am J Ophthalmol. 2010;150:82-87.e1.




