 |
 |
Retinal detachments occur in about one out of every four eyes with a ruptured globe, typically days to weeks after the initial injury. They are often associated with vitreous hemorrhage, as well as choroidal hemorrhage or detachment, which can make surgical planning and the surgery itself more complicated.
Here we offer 10 suggestions we’ve found useful in the management of these complex patients.
1. Do a careful preoperative exam. Anticipate potential difficulties (e.g., limited anterior view secondary to corneal sutures, site of rupture where you might normally place your infusion) and plan appropriately.
Ultrasonography the day or morning before surgery can be helpful to assess the presence of choroidal detachments and to evaluate the location of the retinal detachment, which may change from the time of diagnosis to surgery. Recognize that there may be incarcerated retina within a posteriorly ruptured site. Read the operative report from the initial surgery.
2. Start by thoughtfully placing your infusion. If you have no view of the posterior pole, place an anterior infusion, either with an anterior chamber maintainer or a small-gauge microcannula placed at the limbus.
3. Work from front to back. Begin by clearing your view anteriorly by whatever means necessary—scrape the cornea, wash out the anterior chamber, remove the traumatic cataract.
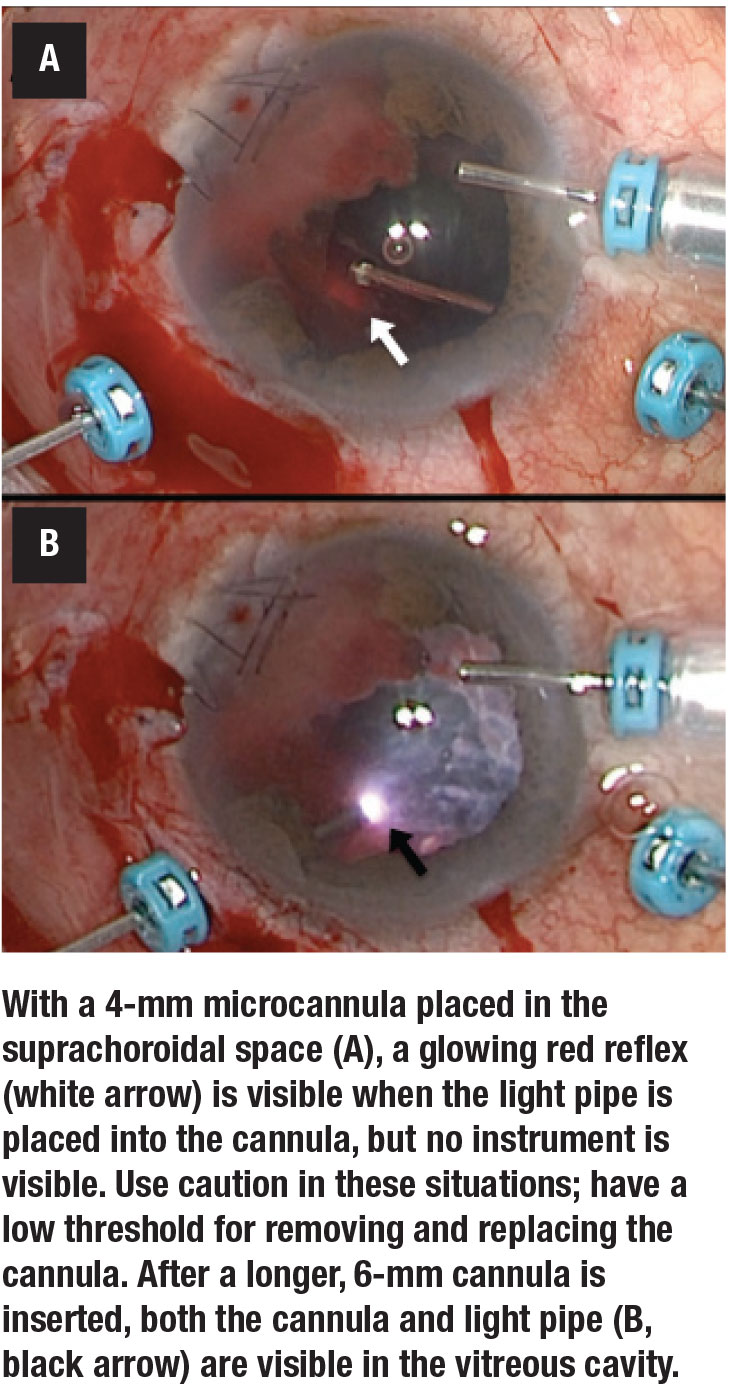
4. When you have a view of the vitreous cavity, make your posterior sclerotomies. Be careful; shallow choroidal detachments or suprachoroidal hemorrhage, often accompanied by vitreous hemorrhage that obscures the view, puts an eye at risk for inadvertent placement of a cannula in the suprachoroidal space, especially into a soft eye.
It may be helpful to replace a standard 4-mm cannula with a longer 6-mm cannula, available in some systems. Be vigilant to avoid trimming what may be retina or choroid masquerading as vitreous overlying the cannula.
5. Once both instruments are safely in the vitreous cavity, slowly clear dense hemorrhage, cautiously proceeding
anterior to posterior until the retina is visualized. At this point a posterior infusion may be placed. Apply similar caution to directly visualize the infusion line and avoid placement in the suprachoroidal space. As noted above, a longer 6-mm cannula can be helpful in this situation.
6. If the retina is incarcerated or extensive proliferative vitreoretinopathy membranes are present, a posterior retinectomy is often needed. Peel all membranes from posterior to anterior prior to performing a generous relaxing retinectomy. Remember that in these eyes, the PVR may be both preretinal and subretinal.
7. Perfluorocarbon liquids can be helpful. PFCLs can be used both for stabilizing the posterior retina and for displacing subretinal blood.
8. Once a relaxing retinectomy has been performed, these cases can be approached like a giant retinal tear. Bring the PFCL up past the retinectomy edge to allow for placement of a laser barricade and an air-fluid exchange.
9. Silicone oil is often the tamponade of choice given its stability and duration.
10. Follow the patients closely for the development of PVR redetachment.
Good luck! RS
Surgery to repair RD after ruptured Globe.
REFERENCES
1. Stryjewski TP, Andreoli CM, Eliott D. Retinal detachment after open globe injury. Ophthalmology. 2014;121:327-333.
2. Nowomiejska K, Choragiewicz T, Borowicz D, et al. Surgical management of traumatic retinal detachment with primary vitrectomy in adult patients. J Ophthalmol. 2017;2017:5084319. 3. Orban M, Islam YFK, Haddock LJ. Timing and outcomes of vitreoretinal surgery after traumatic retinal detachment. J Ophthalmol. 2016;2016:4978973.




