Take-home points
|
 |
|
Bios Ms. Pakravan is a medical student at the University of Miami Miller School of Medicine. Dr. Sridhar is an associate professor of clinical ophthalmology at the Bascom Palmer Eye Institute in Miami. DISCLOSURES: Ms. Pakravan has no disclosures to report. Dr. Sridhar is a consultant to Alcon, DORC, Genentech/Roche and Regeneron Pharmaceuticals. |
It’s well known that treatments with anti-VEGF agents pose a significant burden on patients due to the high costs for certain agents, patient anxiety and discomfort, time constraints, the need for frequent clinic visits and the treatments’ transient effects.1 Additionally, real-world studies have reported suboptimal response or failure to maintain a response compared to randomized clinical trials, possibly because adherence to therapy may not be feasible for some patients.2 It has been well-documented that undertreatment of neovascular age-related macular degeneration may result in progressive vision loss.2
Moreover, agents that target the complement cascade in dry AMD are emerging. Two potential drugs now in clinical trials are pegcetacoplan (APL2, Apellis Pharmaceuticals), which targets C3 in the complement cascade, and avacincaptad pegol (Zimura, Iveric Bio), which targets C5.3,4 Both of these agents are injected monthly per the trial protocol and have shown a reduction in the growth rate of geographic atrophy lesions. Although they have the potential for treating the millions of people suffering vision loss from GA worldwide, the monthly injections for this population may further overwhelm retina providers and practices. This only heightens the urgency to achieve better durability in treatment for wet AMD patients.
To address the limitations the current anti-VEGF treatment paradigm imposes on patients, their families and the health-care system, longer-lasting agents, alternative therapies and novel delivery systems are in development, which we discuss here.
 |
|
Figure 1. The port delivery system with ranibizumab (Susvimo, Genentech/Roche) as it appears under the healed sclera one month after implantation. (Courtesy Carl D. Regillo, MD) |
Seeking greater durability with what we already have
Brolucizumab (Beovu, Novartis) is an anti-VEGF agent the Food and Drug Administration approved in 2019 for the treatment of nAMD.5 It’s concentrated to achieve higher molar equivalent doses than other anti-VEGF drugs because of its high solubility and small molecular weight.
The HAWK and HARRIER Phase III clinical trials reported that optical coherence tomography-based anatomical outcomes favored brolucizumab over aflibercept, with 76 percent of brolucizumab participants maintained on q12-week dosing after loading doses up to week 48.6 However, anecdotal and published reports of postmarket data demonstrated a higher rate of intraocular inflammation, occlusive retinal vasculitis and permanent vision loss associated with intravitreal brolucizumab.5 These safety signals have deterred many providers from using this agent for their patients.
 |
Targeting Tie-2
Another novel pathway involves the role of Tie-2 receptors in vascular permeability. Angiopoietin-1 (Ang-1) is a ligand that activates Tie-2 receptors and reduces vascular permeability, while angiopoietin-2 (Ang-2) is a competitive antagonist that increases vascular leakage.7
Intravitreal faricimab (Vabysmo, Genentech/Roche), the newest FDA-approved addition to drugs for nAMD, is a bispecific antibody that targets both VEGF-A and Ang-2.1 The approved labeling allows administration every one to four months, depending on patient response, after four initial monthly injections.8
The Phase III TENAYA and LUCERNE trials demonstrated noninferiority of faricimab with treatment intervals up to 16 weeks compared to aflibercept q8 weeks. More importantly, TENAYA and LUCERNE showed that 45.7 and 44.9 percent of nAMD patients on faricimab, respectively, were extended to dosing every 16 weeks.8 Notably, 79.7 and 77.8 of patients in TENAYA and LUCERNE, respectively, achieved at least 12-week intervals between injections.
As such, faricimab appears to have the potential to enhance patient quality of life without negative outcomes. However, real-world data regarding the safety of faricimab aren’t available yet. Because of the reports of postmarket adverse events with brolucizumab, many clinicians are awaiting more real-world experience before they start treating stable patients with this newest-approved intravitreal agent. 8
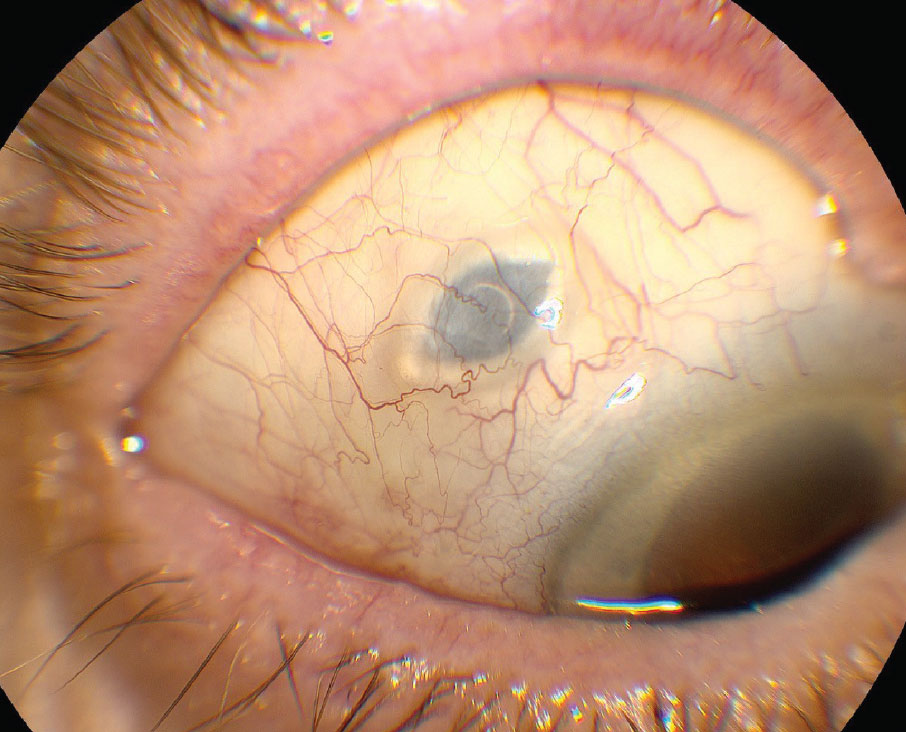
Sustained-release options
Besides newer drugs, clinicians now have the option of sustained-release of long-approved anti-VEGF therapy. The FDA last year approved the port delivery system with ranibizumab (Susvimo, Genentech/Roche) for patients with nAMD (Figure 1).9 The PDS is a surgically implanted device that involves a refillable reservoir accessible via the conjunctiva and extending via the pars plana into the vitreous cavity.
The Phase III ARCHWAY study demonstrated the potential of PDS; the need for refill injection was no more than twice a year after implantation.9 They reported that results for PDS with refill frequency of every 24 weeks was both noninferior and equivalent to monthly ranibizumab injections, and 98.4 percent of PDS patients didn’t need rescue therapy before the first refill-exchange.9
Despite the obvious benefit of less frequent treatments and potentially less clinic visits, the PDS was associated with a higher rate of endophthalmitis (1.6 percent) compared with ranibizumab monthly injections in ARCHWAY.9 Other reported adverse events from the trial included retinal detachments (5.2 percent), vitreous hemorrhage (2.4 percent), conjunctival erosion (2.4 percent) and conjunctival retraction (2 percent).9 Again, given its recent approval, real-world data regarding the efficacy and safety of PDS aren’t available.
 |
Investigative gene therapies
Gene therapy is a promising opportunity that has been explored most vigorously in ophthalmology in inherited retinal diseases. This process introduces a foreign DNA into host cells via a viral vector. The transfected cells become capable of transcribing the new copy of genes into functional proteins to treat the disease.2
The eye represents an ideal target for gene therapy because of its accessibility, the relative ease of measuring structural and functional outcomes and the blood-retina barrier, which prevents a systemic immunogenic response. Gene therapies may provide an avenue for continuous anti-VEGF therapy with only one treatment.
Although the FDA has approved one gene therapy for inherited retinal diseases (Luxturna [voretigene neparvovec-rzyl] Spark Therapeutics) and spinal muscular atrophy, gene therapy for nAMD is still investigative.
RegenxBio is studying a vector, RGX-314, that can express an anti-VEGF antibody fragment similar to ranibizumab.10 RGX-314 is injected subretinally after completion of pars plana vitrectomy. The Phase IIb/III ATMOSPHERE trial is enrolling patients with nAMD, and has shown promising results so far with no reports of clinically determined immune responses, drug-induced ocular inflammation or postoperative inflammation beyond what’s expected after a vitrectomy procedure.10
Alternatively, Adverum Biotechnologies is studying gene vectors for nAMD that may not require surgery. ADVM-022 and ADVM-032 are vectors that can express aflibercept and ranibizumab, respectively, using a single in-office intravitreal injection.11
These agents are still in clinical trials, but early results have shown greater than an 80-percent reduction in monthly anti-VEGF injection burden, and maintenance of best-corrected visual acuity and central retinal thickness with no reported systemic adverse events.2,11
However, last year Adverum suspended its gene therapy clinical trials in diabetic macular edema because of emerging cases of unexpected hypotony 16 to 36 weeks after receiving a high dose of ADVM-022.12 As such, safety signals are being monitored closely in the nAMD trials of ADVM-022.
 |
An adjunct: Home-based monitoring
Even if these investigative therapies alleviate the treatment burden on patients, their families and the healthcare system, the issue of monitoring between treatments would remain. Patients could theoretically come to a physician’s office as infrequently as twice a year with a functional PDS, but they would still need to make an office visit for OCT imaging to monitor their treatment response.
The ForeseeHome (Notal Vision) remote telemonitoring technology has been developed to give physicians the capability to monitor disease activity remotely.13 ForeseeHome monitors changes in visual function using preferential hyperacuity perimetry to detect signs of scotoma or metamorphopsia suggestive of choroidal neovascularization.14 The device informs the retina specialist of vision changes so they can schedule an office appointment to evaluate the patient’s disease activity.
Another technology, home-based OCT (Figure 2), is an investigative device that captures OCT scans in the patient’s home. Data have shown that more than 90 percent of patients were able to obtain analyzable images.13 The data also suggest the device’s high sensitivity in detecting intraretinal and subretinal fluids.
These home devices may have the potential to detect disease activity earlier in patients with nAMD, improve their treatment outcomes and allow providers to use pro re nata treatment for more patients.
 |
|
Figure 2. A patient self-images with the Home OCT (Notal Vision) investigational home-based optical coherence tomography device. |
Bottom line
Although anti-VEGF therapy has become the primary treatment option for patients with wet AMD and has improved their prognosis, the long-term and frequent treatment requirement poses an excessive financial and logistical burden on both patients and their providers. The development of newer drugs with a possibility for less frequent injections or delivery methods with sustained release of anti-VEGF-A could offer the retina community better options to manage patients with nAMD.
Patients may also more widely use home devices to monitor their disease progression and schedule their clinic visits when necessary. These strategies can potentially improve patient compliance and help them stay on top of their AMD treatment, which will ultimately result in enhanced visual outcomes, while easing the treatment burden on them, their providers and the healthcare system. RS
REFERENCES
1. Al-Khersan H, Hussain RM, Ciulla TA, Dugel PU. Innovative therapies for neovascular age-related macular degeneration. Expert Opin Pharmacother. 2019;20:1879-1891.
2. Tan CS, Ngo WK, Chay IW, Ting DS, Sadda SR. Neovascular age-related macular degeneration (nAMD): A review of emerging treatment options. Clin Ophthalmol. 2022;16:917-933.
3. Jaffe GJ, Westby K, Csaky KG, et al. C5 inhibitor avacincaptad pegol for geographic atrophy due to age-related macular degeneration: A randomized pivotal Phase 2/3 trial. Ophthalmology. 2021;128:576-586.
4. Liao DS, Grossi FV, El Mehdi D, et al. Complement C3 inhibitor pegcetacoplan for geographic atrophy secondary to age-related macular degeneration: A randomized phase 2 trial. Ophthalmology. 2020;127:186-195.
5. Motevasseli T, Mohammadi S, Abdi F, Freeman WR. Side effects of brolucizumab [published correction appears in J Ophthalmic Vis Res. 2022;17:157]. J Ophthalmic Vis Res. 2021;16:670-675.
6. Dugel PU, Koh A, Ogura Y, et al. HAWK and HARRIER: Phase 3, multicenter, randomized, double-masked trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology. 2020;127:72-84.
7. Hansen TM, Singh H, Tahir TA, et al. Effects of angiopoietins-1 and -2 on the receptor tyrosine kinase Tie2 are differentially regulated at the endothelial cell surface. Cell Signal. 2010 ;22: 527–532.
8. Heier JS, Khanani AM, Quezada Ruiz C, et al. TENAYA and LUCERNE Investigators. Efficacy, durability, and safety of intravitreal faricimab up to every 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): Two randomized, double-masked, phase 3, non-inferiority trials. Lancet. 2022;399:729-740.
9. Holekamp NM, Campochiaro PA, Chang MA, et al. Archway randomized Phase 3 trial of the port delivery system with ranibizumab for neovascular age-related macular degeneration. Ophthalmology. 2022;129:295-307.
10. Wet age-related macular degeneration (wet AMD) is caused by the formation of new leaky blood vessels in the retina, a tissue at the back of the eye that is responsible for sight (senses light and forms visual images). RegenxBio. https://www.regenxbio.com/wet-amd/. Accessed May 16th, 2022.
11. Adverum Biotechnologies provides update on OPTIC phase 1 trial for ADVM-022 in wet AMD [press release]. Menlo Park, CA; Adverum Biotechnologies; May 16, 2019. http://investors.adverum.com/news-releases/news-release-details/adverum-biotechnologies-provides-update-optic-phase -1-trial-advm.
12. Adverum provides update on ADVM-022 and the INFINITY Trial in patients with diabetic macular edema [press release]. Menlo Park, CA; Adverum Biotechnologies; July 22, 2021. https://investors.adverum.com/news/news-details/2021/Adverum-Provides-Update-on-ADVM-022-and-the-INFINITY-Trial-in-Patients-with-Diabetic-Macular-Edema/default.aspx.
13. Busquets MA, Sabbagh O. Current status of home monitoring technology for age-related macular degeneration. Curr Opin Ophthalmol. 2021;32:240-246.
14. Yu HJ, Kiernan DF, Eichenbaum D, Sheth VS, Wykoff CC. Home monitoring of age-related macular degeneration: Utility of the ForeseeHome device for detection of neovascularization. Ophthalmol Retina. 2021;5:348-356.



