 |
Common intraocular lens designs include open-loop anterior chamber IOLs (AC-IOL), iris clipped, sutured IOLs and scleral-haptic fixated IOLs. Clipping of lenses on the iris using an iris-claw IOL is a well-established technique in the treatment of aphakia without capsular support. Jan Worst, MD, first described this technique in 1972, initially implanting the lens into the anterior chamber clipped to the anterior surface of the iris.1 This technique proved to be safe and effective, and provided predictable clinical results without direct angle compromise.2–4 It was also faster to perform compared to iris-sutured or scleral haptic-fixated IOL.
The main concern of implanting the iris-claw IOL in the anterior chamber is endothelial cell loss; studies have reported rates as high as 10.5 to 13.4 percent at three to four years post-implantation of anterior Artisan IOLs (Ophtec),4–6 particularly in the presence of narrow anterior chambers.7,8 These lenses have since been implanted retropupillary, clipped to the posterior surface of the iris, a technique that has been shown to have lower risk of endothelial cell loss while providing good and predictable clinical outcomes.9–11
Here, the last in the series “Beyond the Retina,” we describe our surgical technique for retropupillary implantation of the iris-claw IOL and discuss the efficacy and safety of the IOL.
Surgery Planning and Technique
The ideal candidate for an Artisan IOL would be a patient with adequate iris stroma, pupil size of ≤5 mm and central pupil position. Small iris defects that do not preclude stable IOL implantation and corectopia where the optic can cover the pupil are not excluded. Although sufficient iris tissue is required for support, the surgeon may employ suture pupilloplasty if needed to reform the pupil, and the IOL may be placed in any axis desired.1 Contraindications to implanting an iris-claw IOL would include uveitis and large iris defects.
The Artisan Aphakia IOL is a single-piece biconvex polymethyl methacrylate IOL that is 8.5 mm in length and 1.04 mm in height with a 5.4 mm optical zone width. The manufacturer’s recommended A constant for implantation above the iris is 115 for ultrasound biometry or 115.7 for optical biometry. For retropupillary implantation, we use an A constant of 116.8 for ultrasound biometry or 116.9 for optical biometry
.
Preferred Surgical Technique
The following describes the surgeon’s preferred surgical technique:
Introduce the anterior chamber maintainer through an inferotemporal limbal corneal incision to maintain intraocular pressure.
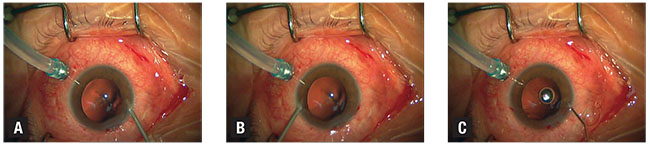 |
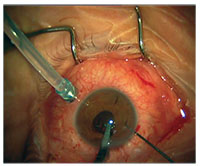
| Figure 1. This is a patient who underwent insertion of a retropupillary Artisan IOL combined with 27-gauge removal of silicone oil in the left eye. Posterior infusion is used for maintenance of intraocular pressure. The first step involves creating a nontunneled paracentesis at the limbus at 10 o’clock (A). Posterior infusion is kept for maintenance of intraocular pressure. This specific patient had a pre-existing inferior peripheral iridectomy. Then, create a second paracentesis at the limbus at 2 o’clock (B). Inject acetylcholine chloride 1% (Miochol) to achieve miosis of the pupil (C). |
Create two nontunneled paracentesis incisions at the 2 and 10 o’clock positions (Figures 1A and B) and inject acetylcholine chloride 1% (Miochol) to achieve miosis (Figure 1C).
Inject a cohesive ophthalmic viscosurgical device (OVD) (Figure 2A) into the anterior chamber and create a superior 5.5-mm limbal corneal incision at 12 o’clock (Figure 2B) or in the desired axis. Perform a superior iridotomy.
Flip the Artisan iris-claw IOL upside-down outside of the eye and introduce it into the anterior chamber through the superior corneal wound using the DO2-70/72/74 Artisan Implantation Forceps (Ophtec) (Figure 3A).
Once in the
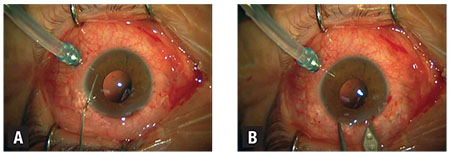 |
| Figure 2. Inject a cohesive ophthalmic viscosurgical device to deepen the anterior chamber and protect the corneal endothelium during Artisan IOL insertion (A). Create a superior corneal incision with a keratome, using calipers to measure 5.5 mm (B). |
Once the Artisan IOL is in the desired position, gently slide it behind the iris one haptic at a time. To facilitate enclavation, tilt the IOL so the haptic on the side of the nondominant hand is pressed upward against the iris, creating an imprint against the iris and thus facilitating location of the haptic slot.
Using the nondominant hand, insert a iris hook through the paracentesis on the same side and push sufficient mid-peripheral iris tissue into the slot of the haptic (Figure 4A). Swap hands and repeat this step on the other side (Figure 4B). Take care not to distort the iris while sliding the second haptic posteriorly to avoid disenclavation of the first haptic, to promote central positioning of the optic and maintain a round pupil.
Close the corneal incisions with interrupted 10-0 vicryl sutures (Figure 5). Flush the OVD in the anterior chamber with balanced salt solution and hydrate the paracentesis wounds to ensure a watertight seal.
Should a simultaneous vitrectomy be required, our preference is a 27-gauge vitrectomy for its superior wound closure and lower conjunctival
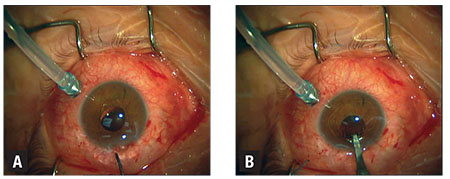 |
| Figure 3. After flipping the Artisan intraocular lens outside the eye, insert it into the anterior chamber centered over the pupil (A), and rotate it so that the haptics are at 3 and 9 o’clock (B). The DO2-70/72/74 Artisan Implantation Forceps hold the IOL stable. This patient did not have a superior iridectomy as he had a pre-existing inferior iridectomy. |
Options for IOL Fixation
With the advances in surgical devices, IOL models and suture materials, surgeons are now presented multiple options to tackle aphakia without adequate capsule support. Implantation of an AC-IOL is a quick and easy option; however, its use in younger patients is less preferred due to the considerable risks of angle damage and endothelial cell loss compared to iris- or scleral-haptic-fixated IOLs.12
Scleral-haptic fixation of IOLs can be performed with or without sutures and is most commonly approached ab externo through the ciliary sulcus or pars plana using the corneal limbus as an external landmark.13,14 This requires IOLs with suture eyelets to allow stable anchoring of sutures to the IOL. These include the Akreos Adapt (Bausch + Lomb), CZ 70 BD (Alcon) and enVista MX60 (B+L) IOLs. Preferred sutures are polypropylene or Gore-tex. Scleral-haptic fixation is accomplished by threading sutures through the haptic eyelets and then insertion of the IOL into the posterior chamber.
The sutures are then externalized through the sclera 2 to 3 mm from the limbus using a 27-gauge needle to dock the needle, or using intraocular forceps to grasp the suture through the pars plana cannula. Timothy Olsen, MD, and Jonathan Pribila, MD, at Emory Eye Center in Atlanta described a novel technique of passing sutures ab interno using intraocular endoscopy to locate the ciliary sulcus under direct visualization.15
Fixation
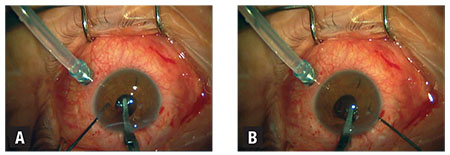 |
| Figure 4. Once the desired position is achieved, gently slide one haptic behind the iris and tilt it upwards against the iris, creating an imprint on the iris to facilitate the location of the haptic slot. Insert the iris hook through the paracentesis on the same side and use it to push sufficient mid-peripheral iris tissue into the slot of the haptic (A). Repeat the previous steps with the other haptic (B). |
Once the IOL is inserted into the posterior chamber, haptic retrieval is done using 27-gauge needle to dock the needle in a “handshake” technique and the externalized haptics can be tucked under scleral flaps or scleral tunnels.16–18 Authors have also described modified techniques employing the use of fibrin glue or thermal cautery to create a flanged haptic.16,19, 20
The options for iris fixation of IOLs include sutured or clipped. Suturing of the IOL onto the iris involves the use of a three-piece posterior chamber lens that can be injected though a 3- to 3.5-mm corneal incision; a Siepser sliding knot with 10-0 polypropylene secures the haptics to the peripheral iris. Compared to scleral fixation of IOLs, iris suturing has the advantage of no externalized sutures, hence reduced risk of endophthalmitis, and it preserves the conjunctiva, which is of importance in glaucoma patients.
Safer and Faster
In our opinion, once one acquires sufficient experience, either anterior or posterior chamber iris-claw IOL implantation is safer and faster compared to the other techniques. The disadvantages of the iris-claw IOL technique are, when compared to iris-sutured techniques, induced astigmatism secondary to the larger corneal incision wound of 5.5 mm, and, when compared to scleral fixated or sutured IOL techniques, its contraindication in uveitis patients. Reported complications
 |
| Figure 5. Close the main corneal wound with interrupted 10-0 vicryl sutures after removal of OVD. |
A study of 320 eyes with retropupillary iris-fixated Artisan IOL evaluated its long-term stability and reported over an average of 5.3 years three (0.9 percent) cases of disenclavation with one complete posterior dislocation, one (0.3 percent) retinal detachment and three (0.9 percent) cases of CME.9 The investigators reported no cases of iritis or postoperative elevated intraocular pressure and no statistically significant change in endothelial cell density at the study end.
Another study of 137 eyes reported higher rates of complications with a mean follow-up of five months. These researchers found CME occurring in 12 eyes (8.7 percent), endophthalmitis in one (0.7 percent), hyphema in three (2.1 percent), chronic uveitis requiring IOL removal in one (0.7 percent) and disenclavation in 12 (8.7 percent).21 However, such rates are still comparatively lower than with the transscleral-sutured IOL, in which CME has been reported to occur in 5.8 percent to 33 percent of cases,22,23 retinal detachment in 6.3 percent to 8.2 percent, IOL dislocation in 6.3 percent and suture breakage in up to 27.9 percent of cases.24,25 RS
REFERENCES
1. Worst JGF, Massaro RG, Ludwig HHH. The introduction of an artificial lens into the eye using Binkhorst’s technique. Ophthalmologica. 1972;164:387–391.
2. Sawada T, Kimura W, Kimura T, et al. Long-term follow-up of primary anterior chamber intraocular lens implantation. J Cataract Refract Surg. 1998;24:1515–1520.
3. Chen Y, Liu Q, Xue C, Huang Z, Chen Y. Three-year follow-up of secondary anterior iris fixation of an aphakic intraocular lens to correct aphakia. J Cataract Refract Surg. 2012;38:1595–1601.
4. Güell JL, Velasco F, Malecaze F, Vázquez M, Gris O, Manero F. Secondary Artisan–Verysise aphakic lens implantation. J Cataract Refract Surg. 2005;31:2266–2271.
5. Menezo JL, Cisneros AL, Rodriguez-Salvador V. Endothelial study of iris-claw phakic lens: four year follow-up. J Cataract Refract Surg. 1998;24:1039–1049.
6. Koss MJ, Kohnen T. Intraocular architecture of secondary implanted anterior chamber iris-claw lenses in aphakic eyes evaluated with anterior segment optical coherence tomography. Br J Ophthalmol. 2009;93:1301-1306.
7. Saxena R, Boekhoorn SS, Mulder PG, Noordzij B, van Rij G, Luyten GP. Long-term follow-up of endothelial cell change after Artisan phakic intraocular lens implantation. Ophthalmology. 2008;115:608–613.
8. Shajari M, Scheffel M, Koss MJ, Kohnen T. Dependency of endothelial cell loss on anterior chamber depth within first 4 years after implantation of iris-supported phakic intraocular lenses to treat high myopia. J Cataract Refract Surg. 2016;42:1562–1569.
9. Forlini M, Soliman W, Bratu A, Rossini P, Cavallini GM, Forlini C. Long-term follow-up of retropupillary iris-claw intraocular lens implantation: a retrospective analysis. BMC Ophthalmol. 2015;15:143.
10. Gicquel J-J, Guigou S, Bejjani RA, Briat B, Ellies P, Dighiero P. Ultrasound biomicroscopy study of the Verisyse aphakic intraocular lens combined with penetrating keratoplasty in pseudophakic bullous keratopathy. J Cataract Refract Surg. 2007;33:455–464.
11. Gonnermann J, Amiri S, Klamann M, et al. Endothelial cell loss after retropupillary iris-claw intraocular lens implantation. Klin Monatsbl Augenheilkd. 2014;231:784–787.
12. Moschos MM, Nitoda E. The correction of aphakia using anterior chamber intraocular lens in vivo. 2016;30:733–738.
13. Nakashizuka H, Shimada H, Iwasaki Y, Matsumoto Y, Sato Y. Pars plana suture fixation for intraocular lenses dislocated into the vitreous cavity using a closed-eye cow-hitch technique. J Cataract Refract Surg. 2004;30:302–306.
14. Teichmann KD. Pars plana fixation of posterior chamber intraocular lenses. Ophthalmic Surg. 1994;25:549–553.
15. Olsen TW, Pribila JT. Pars plana vitrectomy with endoscope-guided sutured posterior chamber intraocular lens implantation in children and adults. Am J Ophthalmol. 2011;151:287–296.
16. Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinivasan S. Fibrin glue–assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34:1433–1438.
17. Rodríguez-Agirretxe I, Acera-Osa A, Ubeda-Erviti M. Needle-guided intrascleral fixation of posterior chamber intraocular lens for aphakia correction. J Cataract Refract Surg. 2009;35:2051–2053.
18. Gabor SG, Pavlidis MM. Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2007;33:1851–1854.
19. Prakash G, Agarwal A, Jacob S, Kumar DA, Chaudhary P, Agarwal A. Femtosecond-assisted Descemet stripping automated endothelial keratoplasty with fibrin glue-assisted sutureless posterior chamber lens implantation. Cornea. 2010;29:1315–1319.
20. Cervantes LJ. Combined double-needle flanged-haptic intrascleral fixation of an intraocular lens and Descemet-stripping endothelial keratoplasty. J Cataract Refract Surg. 2017;43:593–596.
21. Gonnermann J, Klamann MKJ, Maier A-K, et al. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg. 2012;38:2139-2143.
22. Mittelviefhaus H. A modified technique of transscleral suture fixation of posterior chamber lenses. Ophthalmic Surg Lasers Imaging Retina. 1992;23:496–498.
23. Uthoff D, Teichmann KD. Secondary implantation of scleral-fixated intraocular lenses. J Cataract Refract Surg. 1998;24:945–950.
24. Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol. 2006;141:308–312.
25. Bading G, Hillenkamp J, Sachs HG, Gabel V-P, Framme C. Long-term safety and functional outcome of combined pars plana vitrectomy and scleral-fixated sutured posterior chamber lens implantation. Am J Ophthalmol. 2007;144:371–377.



