 |
Bios Dr. Kibe is the first-year vitreoretinal surgery fellow and Dr. Megalla is the senior vitreoretinal surgery fellow at Yale University School of Medicine, New Haven, Conn. Dr. Nwanyanwu is an assistant professor of ophthalmology and visual science at Yale. Dr. Hahn is a partner at New Jersey Retina in Teaneck. DISCLOSURES: Drs. Kibe, Megalla and Nwanyanwu have no relevant disclosures. Dr. Hahn is a consultant to DORC. |
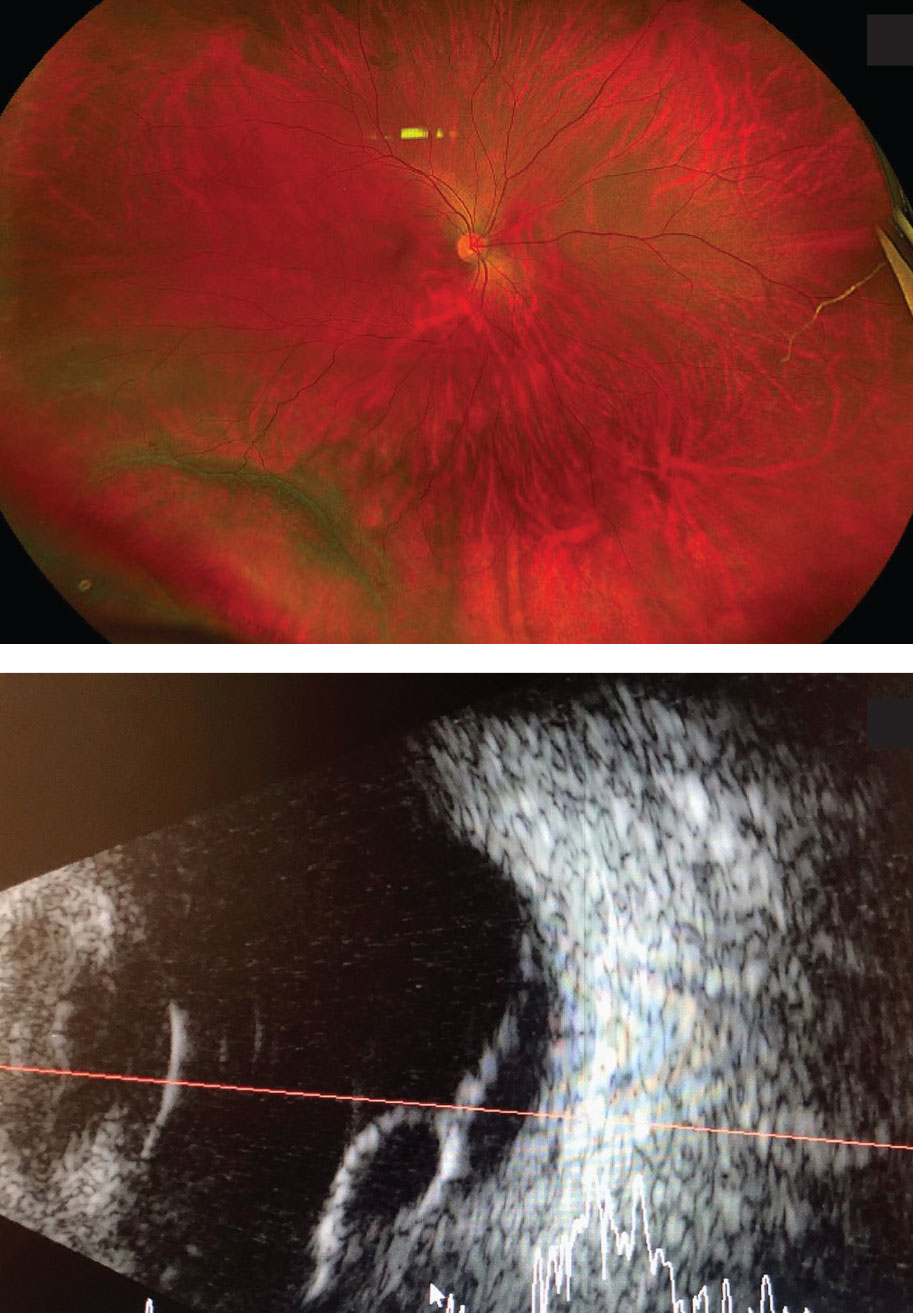
A 29-year-old, myopic, pregnant woman at 36 weeks gestation was referred for evaluation of a macula-on inferotemporal retinal detachment with a retinoschisis component as indicated by ultrasonography (Figure).
|
|
Fundus photograph and B-scan at presentation showed a macula-sparing inferotemporal retinoschisis-associated retinal detachment in our 26-year-old pregnant patient. |
Timing and planning of surgery
Timing of surgical repair was complicated by the fact that the patient was in her third trimester of pregnancy. The American College of Obstetrics and Gynecology recommends delaying elective surgery until after delivery. However, pregnant women should not be denied medically necessary surgery at any trimester.1 The optimal time for non-
obstetric surgery in a pregnant patient is the second trimester, when the risk of preterm labor is lower compared to the third.2
Because this patient was so close to her due date and had an acute-on-chronic appearing retinal detachment, we elected to delay the repair until after delivery, with consultation from her obstetrics team.
From the time of diagnosis to surgery, we followed her with weekly exams and fundus photography for documentation, which demonstrated only minimal progression of her detachment. Surgical repair was undertaken six weeks after initial presentation (two weeks postpartum).
Making the repair
While observation may be appropriate in some cases of retinoschisis-associated retinal detachments, which can often remain stable and asymptomatic long-term, surgical repair is typically required in the setting of progressive symptoms.3
No consensus exists regarding the best surgical methods to repair retinoschisis-associated retinal detachments, although various methods of repair have been employed.4
We elected a scleral buckle combined with a vitrectomy and gas tamponade (15% C3F8) because of the chronic-appearing cavity and inferior location. We also considered the potential challenges with positioning because she was a first-time mother of a newborn. During the case, we did not note any distinct break with scleral depression, but we did observe thinning over the schisis cavity.
We applied endodiathermy to mark the areas of thinning. We drained the subretinal fluid through a drainage retinotomy at 8 o’clock using soft-tip extrusion, then noted a flattening of the retinal schisis cavity. We then applied endolaser around the retinotomy and throughout the retinal schisis cavity. On subsequent postoperative visits, the retina remained attached.
Bottom line
Surgery in a pregnant patient needs to be coordinated with the obstetrics team and anesthesia providers, balancing the urgency of surgery, risks of delay and risks to the pregnancy.5
In a pregnant patient with a chronic-appearing retinoschisis-associated retinal detachment, one can consider close monitoring for progression of detachment and delay surgical repair until safe delivery. RS
REFERENCES
1. ACOG Committee opinion no. 775: Nonobstetric surgery during pregnancy. Obstet Gynecol. 2019;133:844-845.
2. Goodman S. Anesthesia for nonobstetric surgery in the pregnant patient. Semin Perinatol. 2002;26:136-145.
3. Jeroudi AM, Shah V, Blinder KJ, Shah GK. Management of degenerative retinoschisis-associated retinal detachment. Ophthalmol Retina. 2017;1:266-271.
4. Grigoropoulos VG, Williamson TH, Kirkby GR, Laidlaw DA. Outcomes of surgery for progressive symptomatic retinal detachment complicating retinoschisis. Retina. 2006;26:37-43.
5. Brooks CC, Brodie F, Brodie R, Buck M, Postel EA. Management of a rhegmatogenous retinal detachment in a pregnant patient. Am J Ophthalmol Case Rep. 2020;18:100708.




