Techniques and technologies for both cataract and vitrectomy surgery have evolved tremendously in recent years, resulting in improved outcomes and shorter operating times. Cataract surgery is typically performed via a clear-corneal incision ranging in size from 1.5 to 2.8 mm. Similarly, pars plana vitrectomy has been performed safely using progressively smaller instrumentation, including 23, 25 and 27 gauges.1-5
 |
Given the improved safety, speed and recovery time seen with these surgeries, it is apparent that, when done appropriately, combining phacoemulsification and vitrectomy is in the best interests of the patient. This article highlights some of the indications, surgical techniques, advantages and disadvantages of phacovitrectomy when the retina surgeon performs it.
Indications
Patients with visually significant cataracts undergoing vitrectomy are candidates for phacovitrectomy. Even patients with mild degrees of lenticular change are suitable for this procedure, because it will
negate their need for inevitable cataract surgery later on and provide excellent posterior pole visualization for the surgeon.
 |
A relative contraindication is a retina surgeon who is inexperienced in phacoemulsification, because prolonged phacoemulsification can lead to corneal edema and poor visualization of the retina during vitrectomy.
 |
However, with existing machines, techniques and viscoelastic devices, phacoemulsification with intraocular lens implantation can be safely performed in 10 minutes without corneal decompensation.
Phacovitrectomy Advantages
Phacovitrectomy provides a number of advantages to both the patient and the retina specialist. The patient avoids two trips to the operating room and has a faster overall postoperative recovery course compared with undergoing two separate procedures at different dates. This saves the patient money by avoiding copayments for the second procedure. The patient who does not have health insurance or who otherwise pays out of pocket greatly benefits from the combined procedure. It also saves the patient time because he or she does not need to make appointments to see an anterior segment surgeon for the cataract procedure. Visual rehabilitation is faster.
 |
For the retina surgeon, advantages include the following:
Thorough and safe shaving of the vitreous base is possible without fear of lenticular touch.
It affords a better view of the retina for delicate maneuvers such as internal limiting membrane peeling and for detection of small retinal breaks.
Posterior capsular rupture or lens drop is less of a concern, because the retina surgeon has the ability to address such issues immediately if they occur.
Phacoemulsification is easier in a non-vitrectomized eye, because after vitrectomy, cataracts tend to be harder and the anterior chamber tends to fluctuate during phacoemulsification due to the absence of vitreous support, possibly leading to posterior-capsule rents and dropped nuclear fragments. For these reasons, anterior segment surgeons are not keen to operate on vitrectomized eyes.
There are no scheduling mishaps causing the retina surgeon to have to wait for the cataract surgeon to begin the case.
Most third-party payers reimburse 100 percent for the retina procedure and 50 percent for the phacoemulsification, which can be an increased source of revenue for the retina surgeon.
The patient is happy with the retina surgeon’s results, rather than allowing the cataract surgeon to become the hero when he or she does the phacoemulsification later.
Many ophthalmic manufacturers offer combined packs for phacovitrectomy at almost the same rates as individual phaco packs.
The U.S. health-care system also stands to benefit from cost savings if retina surgeons perform more phacovitrectomies.3
But There are Disadvantages
The retina specialist must also consider several potential disadvantages of combined phacovitrectomy. For example, the retina surgeon may fear a loss of referrals from anterior segment colleagues, although our experience has been quite the opposite. As noted, cataract surgeons like to avoid doing phacoemulsification in vitrectomized eyes due to the higher risk of complications, and they are happy to let us take care of their patients’ cataracts during the vitrectomy procedure. Referrals stop, however, when the retina surgeon starts doing primary cataract surgeries.
Another potential disadvantage is that the retina surgeon must be experienced with phacoemulsification. There is also a slightly higher chance of anterior segment inflammation when phacovitrectomy is performed in eyes with diabetic tractional retinal detachment. In such cases, our practice prescribes steroid drops every two hours for the first week rather than the usual four times daily.
Surgery Prep and Techniques
Phacovitrectomy does require some considerations that may be out of the norm for most retina specialists. The following scenarios may provide ideas about how to approach these concerns.
Preoperatively, the retina surgeon must do the IOL power calculation. In our practice’s experience, biometry with the IOLMaster (Carl Zeiss Meditec) has given consistent results. The only time we don’t insert an IOL is if the patient has a macula-off retinal detachment, as the calculations may be inaccurate. In such cases, we perform phacoemulsification without IOL implantation.
After the retina is attached, we send the patient to the referring anterior segment colleague for secondary IOL implantation in the bag. If the patient was not referred, we implant the IOL in a secondary procedure after performing the IOL measurements and calculations.
Preoperatively, we check for the presence of small pupils or posterior synechiae so that we can be ready to use iris hooks if necessary during surgery. We assess the red reflex, especially in vitreous hemorrhages, and use trypan blue dye if the reflex is poor. Use of trypan blue or iris hooks allows for coding at a higher level.
Our office informs the patient that, due to the retinal pathology, multifocal IOLs are probably not indicated. A monofocal accommodating IOL may be a better choice if the patient desires intermediate and near vision independent of spectacles.
How Phaco and Vit Differ
Intraoperatively, most of the basic surgical steps for phacoemulsification and vitrectomy procedures are similar, with the following exceptions.
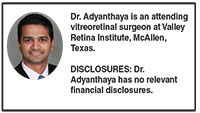
We insert all three ports before starting phacoemulsification (Figure 1, page 21). We do this because inserting the ports after phacoemulsification creates a slightly higher risk of the main cataract incision gaping due to the pressure applied for port insertion.
 |
We make sure to insert the superior ports closer to the horizontal meridian so that they don’t get in the way of the phaco handpiece and chopper. When operating on a right eye and sitting at the patient’s head, we insert the infusion port inferotemporally.
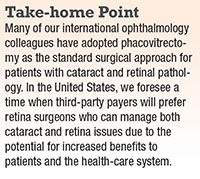
After we visualize that the infusion port is in the proper position, we turn on the infusion, then place the two superior ports in the usual manner transconjunctivally at the 2:30- and 9:30 clock positions (Figure 2). We prefer to use valved trocar systems; however, one can use plugs when valved trocar systems are not available.
We then turn off the infusion so that it can be connected to the phaco handpiece, and start the phacoemulsification portion of the procedure with the side port incision at 2 o’clock and the main incision at the 10-o’clock position.
We have a low threshold for using trypan blue dye if there is a doubt regarding the red reflex, especially with vitreous hemorrhages. If we anticipate the need to use gas at the end of the vitrectomy, we make the capsulorhexis slightly smaller than usual to prevent anterior subluxation of the IOL in the postoperative period. This is a rare occurrence. In the few postoperative IOL subluxations we’ve encountered, we’ve managed to put them back in position at the slit lamp with a 30-gauge needle.
For very dense cataracts, we use ample dispersive viscoelastic material to coat the endothelium prior to phacoemulsification.
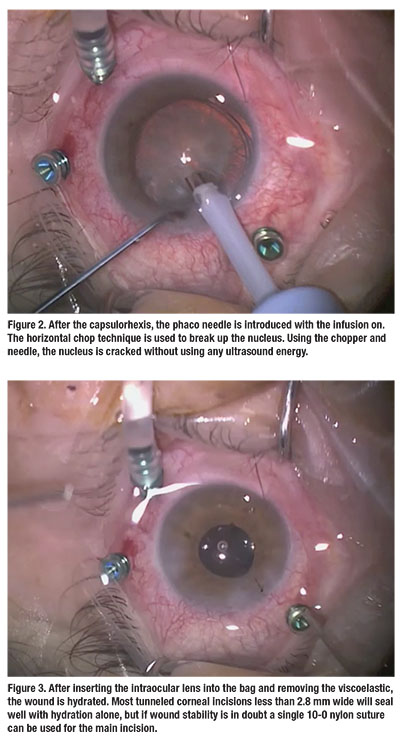
After we insert the IOL into the bag and remove the viscoelastic, we hydrate the wounds (there is no need for sutures). Most tunneled corneal incisions less than 2.8 mm wide will seal well with hydration alone. If wound stability is in doubt, we use a single 10-0 nylon suture for the main incision (Figure 3), then start the vitrectomy in a standard approach after turning on the infusion (Figure 4).
| View the Video Dr. Adyanthaya narrates a video on the key steps of phacovitrectomy in the case of a high myope with a history of a rhegmatogenous retinal detachment who developed a full-thickness retinal hole with a cataract. Click here to view the video. |
Conclusion
Many of us foresee a time when third-party payers will prefer retina surgeons who can manage both cataract and retina issues due to the potential for increased benefits to patients and efficiencies for the health-care system. For these reasons, it behooves the young retina fellowship trainee to avoid losing the phacoemulsification skills learned during residency. Additionally, vitreoretinal fellowship training programs should encourage more phacovitrectomy procedures, given the multitude of benefits outlined here. RS
REFERENCES
1. Canan H, Sizmaz S, Altan-Yaycioglu R. Surgical results of combined pars plana vitrectomy and phacoemulsification for vitreous hemorrhage in PDR. Clin Ophthalmol.2013;7:1597-1601.
2. Oshima Y, Wakabayashi T, Sato T, Ohji M, Tano Y. A 27-gauge instrument system for transconjunctival sutureless microincision vitrectomy surgery. Ophthalmology.2010;117:93-102.e2.
3. Seider MI, Michael Lahey J, Fellenbaum PS. Cost of phacovitrectomy versus vitrectomy and sequential phacoemulsification. Retina. 2014;34:1112-1115.
4. Zheng Q, Wu R, Yang S, Zhang Y, Li W. Clear lens phacoemulsification combined with vitrectomy to correct high myopia: four years of follow-up. Ophthalmic Res. 2013;49:73-80.
5. Savastano A, Savastano MC, Barca F, Petrarchini F, Mariotti C, Rizzo S. Combining cataract surgery with 25-gauge high-speed pars plana vitrectomy: results from a retrospective study. Ophthalmology. 2014;121:299-304.



