 |
 |
 |
When giving anti-VEGF injections for neovascular age-related macular degeneration, most retina specialists “treat to dry,” whether using monthly, bimonthly, pro re nata or treat-and-extend injection regimens. Since the beginning of the anti-VEGF era, retina specialists have collectively concluded that a “dry” retina— one resolved of intraretinal, subretinal or sub-retinal pigment epithelium fluid—would have a better visual acuity outcome than a “wet” retina, one with incompletely resolved fluid in any layer.
However, it's unclear if complete retinal fluid resolution is required for optimal vision outcomes. For example, some nAMD patients will have persistent fluid despite monthly injections and demonstrate good vision, perhaps even 20/20.
In fact, these patients seem to see as well as other patients who are completely dry and perhaps require less frequent injections. This raises the question: What’s the relationship between retinal fluid and vision outcomes?
 |
Lessons from HARBOR post-hoc analysis
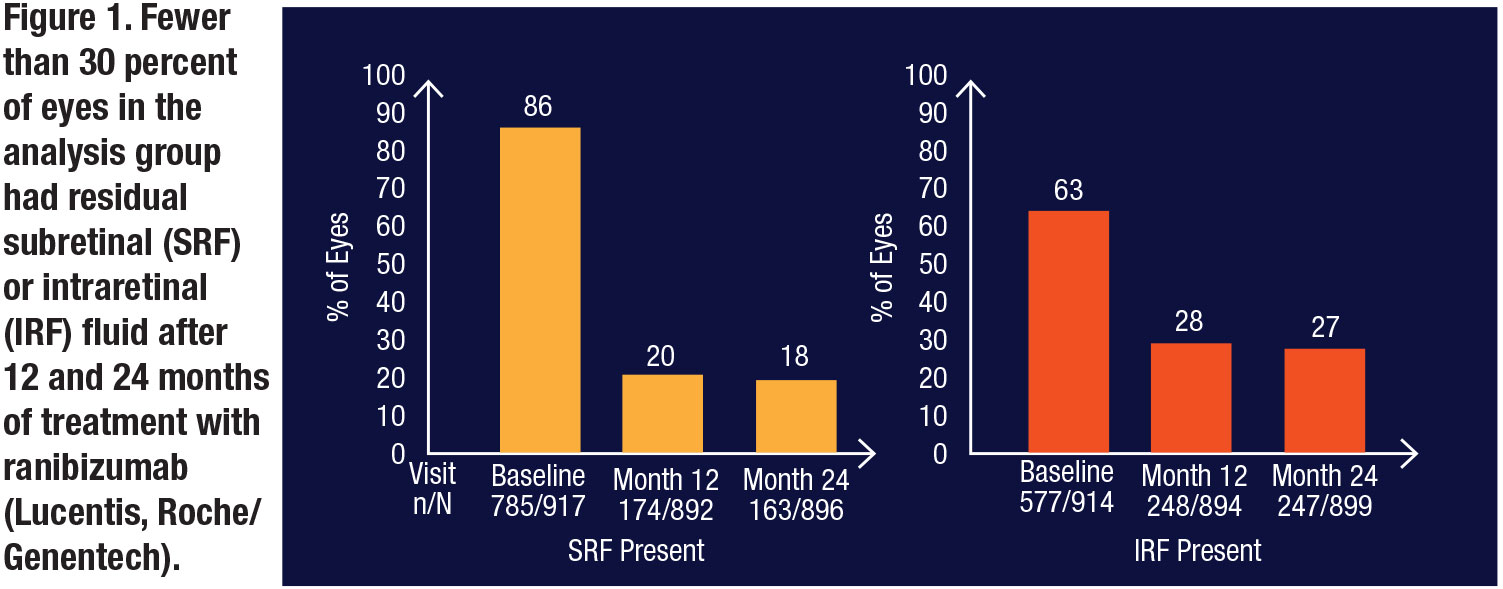
A post-hoc analysis of the HARBOR randomized clinical trial offers insight to this question.1 Of the 1,097 treatment-naïve patients with nAMD randomized in
HARBOR, 917 met inclusion criteria of 24 months of available spectral-domain optical coherence images and either SRF and/or IRF present at baseline, screening or week one, and were pooled for an analysis of fluid and vision parameters. The primary outcome was fluid status and change in best-corrected visual acuity from baseline.
Importantly, fewer than 30 percent of eyes in the analysis population had residual SRF or IRF after 12 and 24 months of ranibizumab injected monthly or prn (Figure 1).
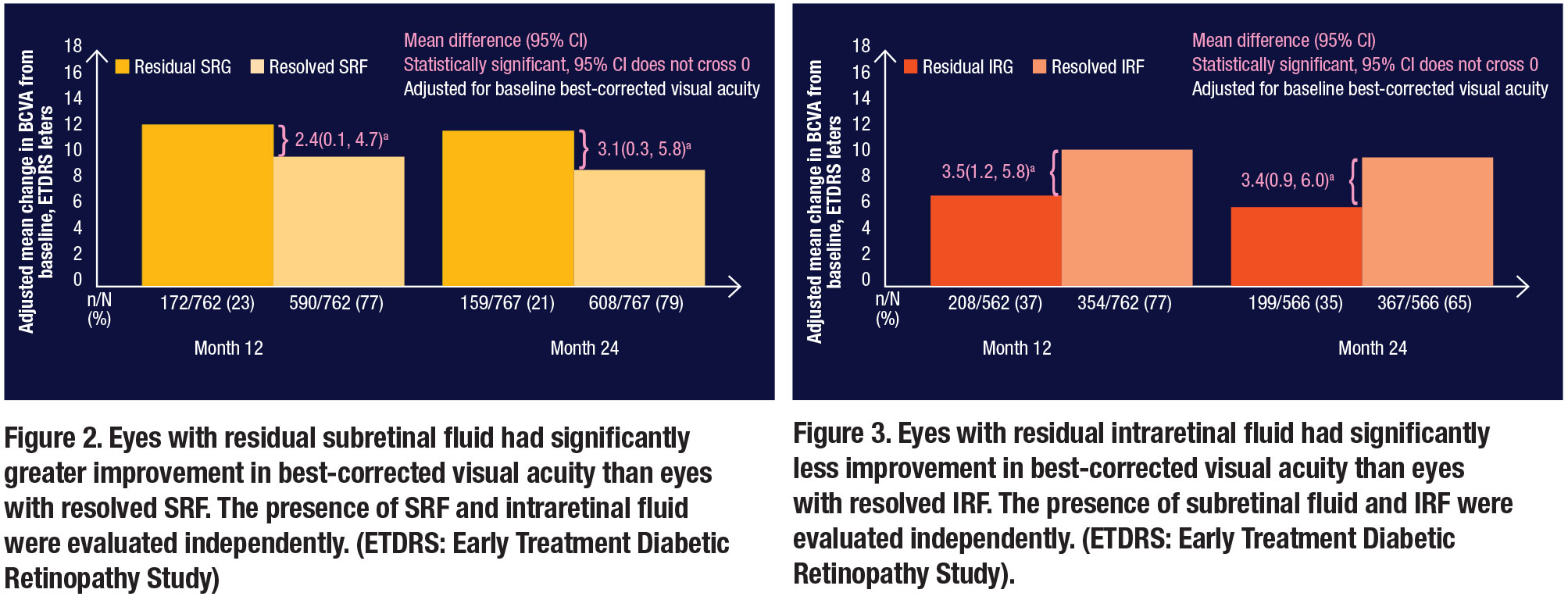
The post-hoc analysis also examined SRF and compared adjusted mean change in BCVA in eyes with residual SRF to eyes with resolved SRF at months 12 and 24 (Figure 2). Eyes with residual SRF had statistically better visual acuity outcomes than eyes with resolved SRF. In short, when looking at SRF, drier was not necessarily better.
In contrast, eyes with residual IRF had statistically worse visual acuity outcomes than eyes with resolved IRF at months 12 and 24 (Figure 3). In short, when looking at IRF, drier was definitely better.
 |
A more nuanced view of fluid
It's important to note that in HARBOR, all eyes were treated monthly or PRN with the purpose of “drying the retina”. Retinal fluid was not tolerated; rather, it was treated consistently.
However, some eyes with nAMD will never achieve complete resolution of fluid, even with treatment. Under these circumstances, the HARBOR post-hoc analysis demonstrated that eyes with persistent SRF see better than eyes that are dry, and eyes with persistent IRF see worse than eyes that are dry, suggesting a very complex relationship between retinal fluid and functional outcomes.
Bottom line
Given this HARBOR analysis and emerging analyses of other large data sets in nAMD, such as the LADDER trial, perhaps a more nuanced view of fluid status and visual acuity outcomes is warranted. RS
Editor’s note: This article is based on a presentation Dr. Holekamp gave at the 37th annual meeting of the American Society of Retina Specialists July 27, 2019, in Chicago.
REFERENCE
1. Ho AC, Busbee BG, Regillo CD, et al, for the HARBOR Study Group. Twenty-four-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology. 2014;121:2189-2192.



