 |
 |
Early detection of diabetic retinopathy is essential to prevent vision loss, and annual eye exams are recommended for surveillance of diabetic patients. Vision changes secondary to DR can be irreversible. Identification of prognostic markers in the peripheral retina may be essential to guiding management and reducing the disease burden earlier in the disease course. Novel ultra-widefield imaging systems are greatly enhancing our ability to observe diabetic changes in the peripheral retina.
Here, we review the state of the science of ultra-widefield imaging in monitoring and managing diabetic retinopathy.
 |
Improving upon ETDRS standard
Back in 1991 the Early Treatment Diabetic Retinopathy Study established the standard seven-field image as the gold standard for detection and classification of DR.1 While montage images have been found to be reliable for the assessment of DR, they‘re time-consuming to acquire and require a skilled photographer and pharmacologic pupil dilation. Conventional fluorescein angiography utilizes retinal photography that can view 30 to 50 degrees of the retina at any given time.2 However, this field of view excludes much of the peripheral retina.
UWFI systems can generate high-resolution images with up to 200-degree (82 percent) views of the retina with scanning laser ophthalmoscopy. UWFI includes options for color photos, red-free images, fundus autofluorescence, and fluorescein and indocyanine green angiography.3,4
 |
Concordance between standard images and UWFI
Several studies have examined concordance in the detection of DR between reference standard images and UWFI. Similar concordance in DR detection has been established between dilated fundus examination, standard seven-field images and UWFI.4-8 However, agreement between DR severity grades in dilated fundus examination or reference standard images and UWFI has been variable.
Visualization of the peripheral retina with UWFI allows the detection of more peripheral lesions and has been demonstrated to lead to higher DR severity grading compared to grading based upon standard seven-field imaging.9,10 UWFI has also been shown to detect more proliferative DR and severe nonproliferative DR than clinical exam alone.6
Significance of predominantly peripheral lesions
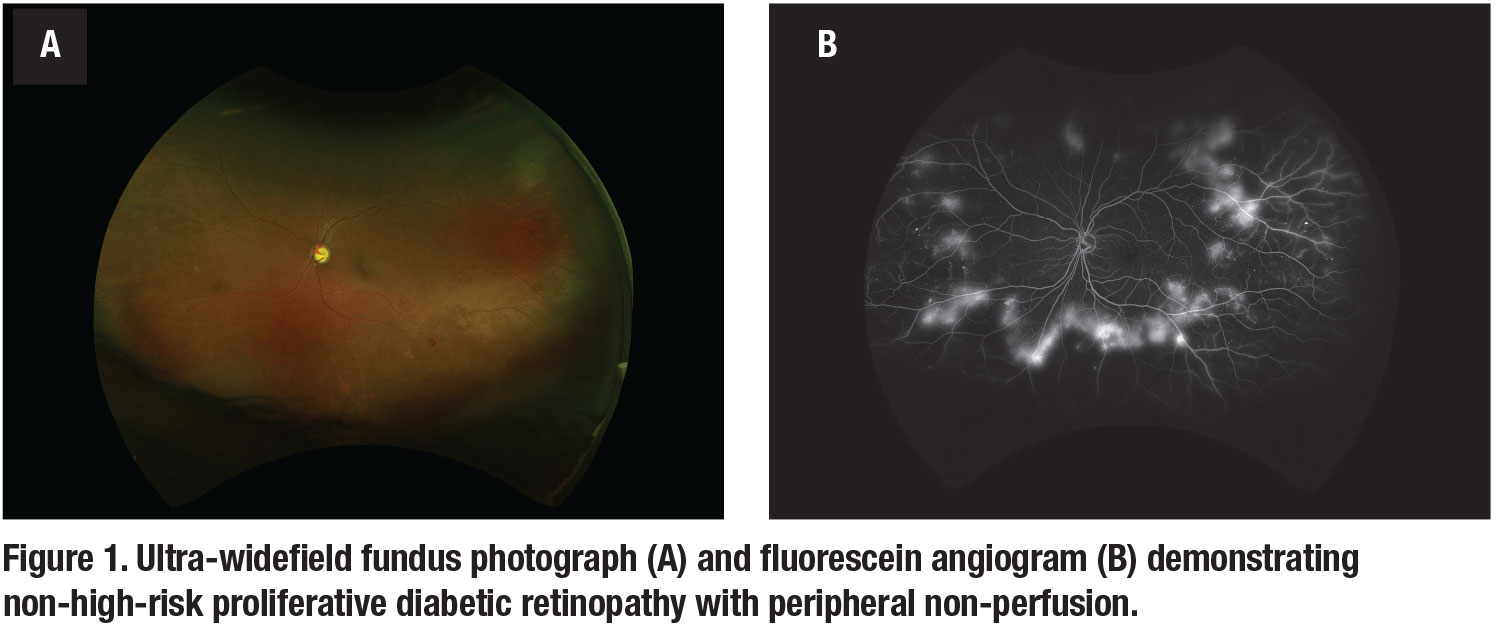
Predominantly peripheral lesions (PPLs) have been defined as DR lesions with a greater extent of the lesions outside vs. inside the standard seven ETDRS fields. A comparison between eyes with and without PPLs as identified on UWFI demonstrated that eyes with PPLs had a 3.2-fold increased risk of two-step or more DR progression on the ETDRS DR severity scale and a 4.7-fold increased risk of progression to PDR (Figure 1).11 Two retrospective case series reported that approximately 10 percent of DR cases presented with lesions only outside of the standard seven fields.9,12
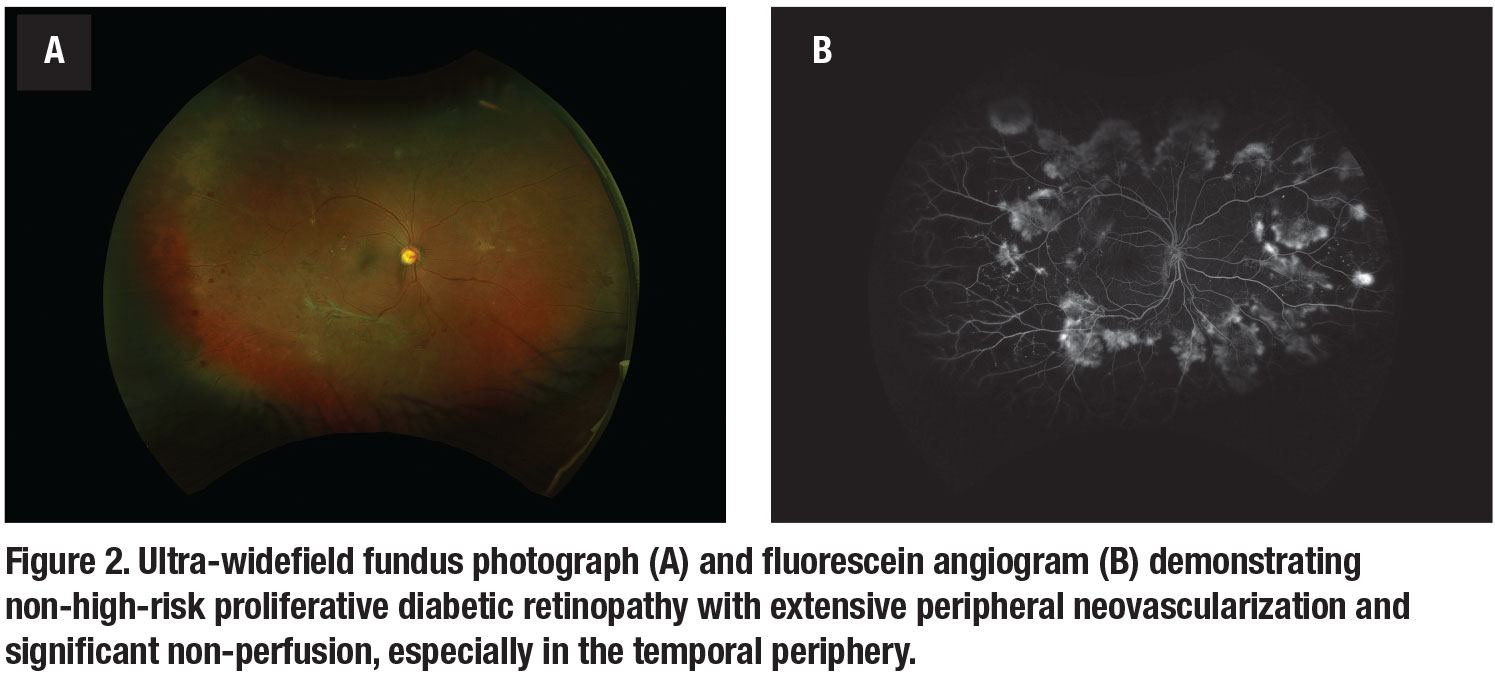
Peripheral retinal non-perfusion in DR stimulates the production of vascular endothelial growth factor, leading to a breakdown of the blood-retinal barrier and development of diabetic macular edema and neovascularization (Figure 2).13,14
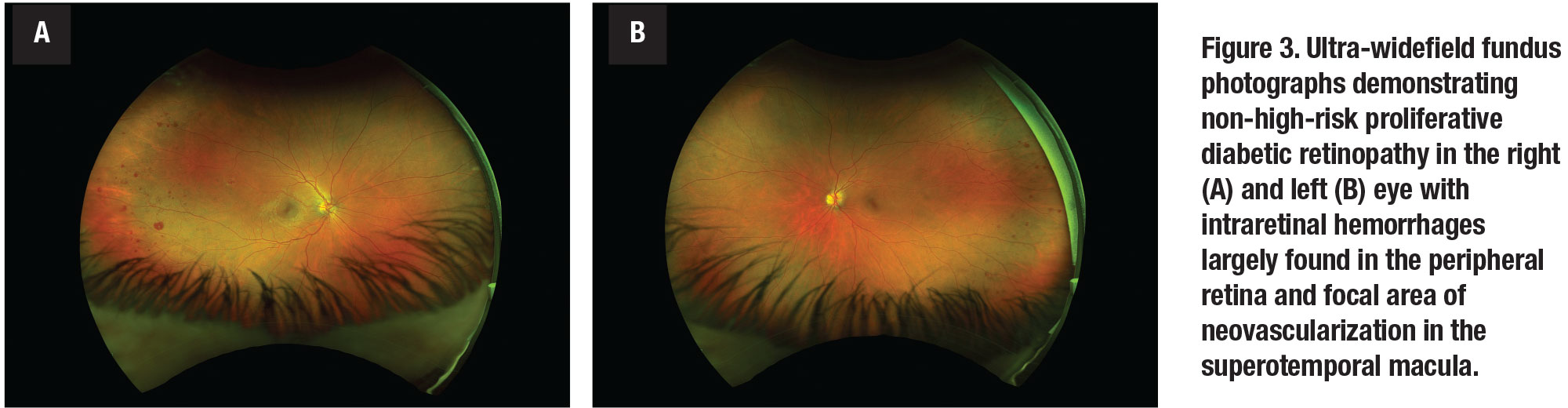
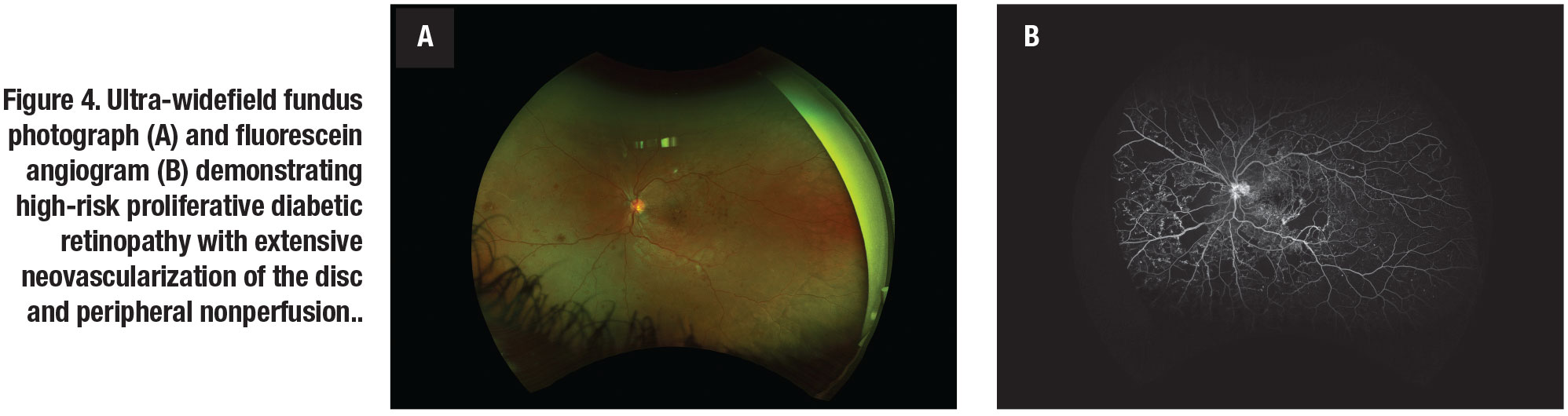
Ultra-widefield angiography has been shown to detect approximately four times more retinal non-perfusion and two times more neovascularization compared to conventional standard seven-field imaging (Figure 3, page 34). Additionally, UWFA detected non-perfusion and neovascularization in 10 percent of eyes that would have otherwise been missed by standard FA (Figure 4,).9
Reports of the association between peripheral non-perfusion and DME are conflicting. Some studies have reported a significant correlation between DME and peripheral retinal ischemia on UWFI. Matthew Wessel, MD, and colleagues found that eyes with retinal ischemia had 3.75-times increased odds of having macular edema compared to those without retinal ischemia.13
Similarly, Ravi Patel, MD, and colleagues reported a correlation between recalcitrant DME with larger areas of retinal non-perfusion in UWFA and greater severity of DR.14 In contrast, Paolo Silva, MD, and colleagues didn’t find an association between clinically significant macular edema and the area of non-perfusion.11
 |
 |
Potential of nonmydriatic UWFI
As a screening tool for DR, fundus photography is especially useful in geographic areas where access to an ophthalmologist is limited. A large study comparing nonmydriatic fundus photos to nonmydriatic UWFI showed that UWFI reduced the number of ungradable eyes by 81 percent, increased the identification of DR by nearly twofold and identified peripheral lesions suggesting more severe DR in approximately 10 percent of patients.15 These findings suggest that UWFI is a convenient and practical tool that can provide high-quality images for reliable diabetic retinopathy screening.
One major advantage of these imaging systems is that they can capture ultra-widefield images without pupil dilation, which is beneficial in diabetic patients who may have a poor response to mydriatic agents.16
Nonmydriatic UWF color images were compared to mydriatic UWF color images and were found to have exact agreement in DR grading in 96.8 percent of cases.5 Additionally, UWFI can be achieved with single-field photography, which allows for shorter imaging time and greater comfort for the patient.
Nonmydriatic UWFI for fundus photography was compared to standard nine-field imaging acquired after pupil dilation. The results showed that DR severity grading was similar between the two systems, and concluded that UWFI was fast and effective, making it acceptable for mass screening for diabetic retinopathy.17
 |
Emerging imaging platforms
New treatment modalities, such as targeted retinal photocoagulation (TRP), are being explored for the treatment of DME and neovascularization. TRP involves selective application of laser to areas of non-perfusion as detected by FA to reduce the level of vascular endothelial growth factor produced by ischemic retina.18 Mahiul M.K. Muqit, PhD, FRCOphth, and colleagues evaluated the effect of UWF FA-guided TRP in 28 eyes with proliferative DA, finding disease regression in 76 percent of eyes at 12 weeks and complete regression in 37 percent at 24 weeks.18
The same group compared TRP, minimally traumatic panretinal photocoagulation (MT-PRP) and standard-intensity panretinal photocoagulation (SI-PRP) and found that, while all three groups had similar rates of PDR regression, the TRP and MT-PRP groups had significant reductions in central retinal thickness.19 UWF FA allows for improved identification of specific areas of retinal non-perfusion to assist in techniques, such as TRP.
 |
 |
Bottom line
The use of UWFI in screening for DR has been widely studied, and its utility is well-established. There is now a growing body of evidence that suggests that UWFI is of considerable importance in the diagnosis, grading and management of DR. Research has established a similar concordance between reference standard images and UWFI with regard to rate of DR detected.
In terms of diabetic severity grading, UWFI has demonstrated high agreement with standard seven-field imaging and improved detection of proliferative and severe non-proliferative DR compared to dilated fundus examination. UWFI has a clear advantage over reference standard images with regard to documenting peripheral lesions. The importance of these peripheral lesions is still under investigation.
New treatment approaches based on UWFI technology are being studied. Large-scale clinical studies investigating UWFI are underway and may further shape our understanding of the role of UWFI technology in diabetic retinopathy. RS
REFERENCES
1. Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98(Suppl):786-806.
2. Ghasemi Falavarjani K, Tsui I, Sadda SR. Ultra-wide-field imaging in diabetic retinopathy. Vision Res. 2017;139:187-190.
3. Shoughy SS, Arevalo JF, Kozak I. Update on wide- and ultra-widefield retinal imaging. Indian J Ophthalmol. 2015;63:575-581.
4. Kernt M, Hadi I, Pinter F, et al. Assessment of diabetic retinopathy using nonmydriatic ultra-widefield scanning laser ophthalmoscopy (Optomap) compared with ETDRS 7-field stereo photography. Diabetes Care. 2012;35:2459-2463.
5. Rasmussen ML, Broe R, Frydkjaer-Olsen U, et al. Comparison between Early Treatment Diabetic Retinopathy Study 7-field retinal photos and non-mydriatic, mydriatic and mydriatic steered widefield scanning laser ophthalmoscopy for assessment of diabetic retinopathy. J Diabetes Complications. 2015;29:99-104.
6. Manjunath V, Papastavrou V, Steel DHW, et al. Wide-field imaging and OCT vs clinical evaluation of patients referred from diabetic retinopathy screening. Eye Lond Engl. 2015;29:416-423.
7. Silva PS, Cavallerano JD, Sun JK, Soliman AZ, Aiello LM, Aiello LP. Peripheral lesions identified by mydriatic ultrawide field imaging: Distribution and potential impact on diabetic retinopathy severity. Ophthalmology. 2013;120(12):2587-2595.
8. Silva PS, Cavallerano JD, Sun JK, Noble J, Aiello LM, Aiello LP. Nonmydriatic ultrawide field retinal imaging compared with dilated standard 7-field 35-mm photography and retinal specialist examination for evaluation of diabetic retinopathy. Am J Ophthalmol. 2012;154:549-559.
9. Wessel MM, Aaker GD, Parlitsis G, Cho M, D’Amico DJ, Kiss S. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 2012;32:785-791.
10. Price LD, Au S, Chong NV. Optomap ultrawide field imaging identifies additional retinal abnormalities in patients with diabetic retinopathy. Clin Ophthalmol Auckl NZ. 2015;9:527-531.
11. Silva PS, Cavallerano JD, Haddad NMN, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 Years. Ophthalmology. 2015;122:949-956.
12. Bae K, Lee JY, Kim TH, et al. Anterior diabetic retinopathy studied by ultra-widefield angiography. Korean J Ophthalmol KJO. 2016;30:344-351.
13. Wessel MM, Nair N, Aaker GD, Ehrlich JR, D’Amico DJ, Kiss S. Peripheral retinal ischaemia, as evaluated by ultra-widefield fluorescein angiography, is associated with diabetic macular oedema. Br J Ophthalmol. 2012;96:694-698.
14. Patel RD, Messner LV, Teitelbaum B, Michel KA, Hariprasad SM. Characterization of ischemic index using ultra-widefield fluorescein angiography in patients with focal and diffuse recalcitrant diabetic macular edema. Am J Ophthalmol. 2013;155:1038-1044.
15. Silva PS, Horton MB, Clary D, et al. Identification of diabetic retinopathy and ungradable image rate with ultrawide field imaging in a national teleophthalmology program. Ophthalmology. 2016;123:1360-1367.
16. Huber MJ, Smith SA, Smith SE. Mydriatic drugs for diabetic patients. Br J Ophthalmol. 1985;69:425-427.
17. Mathis T, Lereuil T, Bruneteau L, et al. [Performance of ultra-wide field retinophotography for screening of diabetic retinopathy]. J Fr Ophtalmol. 2019;42:572-578.
18. Muqit MMK, Marcellino GR, Henson DB, et al. Optos-guided pattern scan laser (Pascal)-targeted retinal photocoagulation in proliferative diabetic retinopathy. Acta Ophthalmol. 2013;91:251-258.
19. Muqit MMK, Young LB, McKenzie R, et al. Pilot randomized clinical trial of Pascal TargETEd Retinal versus variable fluence PANretinal 20 ms laser in diabetic retinopathy: PETER PAN study. Br J Ophthalmol. 2013;97:220-227.



