 |
Bios Dr. Sivalingam is a second-year vitreoretinal fellow at Wills Eye Hospital, Philadelphia. Dr. Cohen is an assistant professor of ophthalmology at Thomas Jefferson University Hospital, Philadelphia, a member of the retina service at Wills Eye Hospital and a member of Mid Atlantic Retina. Dr. Hahn is a vitreoretinal specialist at NJ Retina in Teaneck. DISCLOSURES: The authors have no relevant financial disclosures. Dr. Hahn has no relevant financial disclosures. |
As retina specialists, we have several techniques for intraocular lens placement in eyes with poor capsular support. GORE-TEX-sutured intraocular lens fixation remains a steadfast method that has several advantages, including excellent stability, minimal risk of suture breakage and a small corneal wound through which the IOL can be inserted.1–3
Here, we review GORE-TEX-sutured IOL placement using the Bausch + Lomb enVista MX60 lens with four-point fixation and highlight key steps, and tricks to avoid common issues such as suture tangling, lens decentration and optic tilt.
Cannula positioning
We create peritomies temporally and nasally with relaxing radial incisions for adequate exposure, then use external cautery to achieve proper hemostasis.
Precise and careful measurement before placing the cannula is essential. The corneal limbus is marked at two points along the horizontal axis, each 180 degrees apart to establish the axis of fixation. Rotation by a few clock hours can help avoid interference from the nasal bridge. The sclera is marked at two points, each 3 mm posterior to the limbus, 5 mm apart, centered around the horizontal limbal marks (Figure 1).
A 25-gauge cannula is placed, non-tunneled, at the superior mark and the 25-g trocar, marked with a sterile marking pen, is used to create a sclerotomy at the inferior mark. The same is repeated on the opposite side of the limbus.
When creating these sclerotomies, the blade must be oriented parallel to the limbus to avoid wound gaping when tightening the suture. Mismeasurement during trocar placement can lead to lens tilt and decentration, so it’s essential to take extra time to confirm proper placement.
Avoiding fog
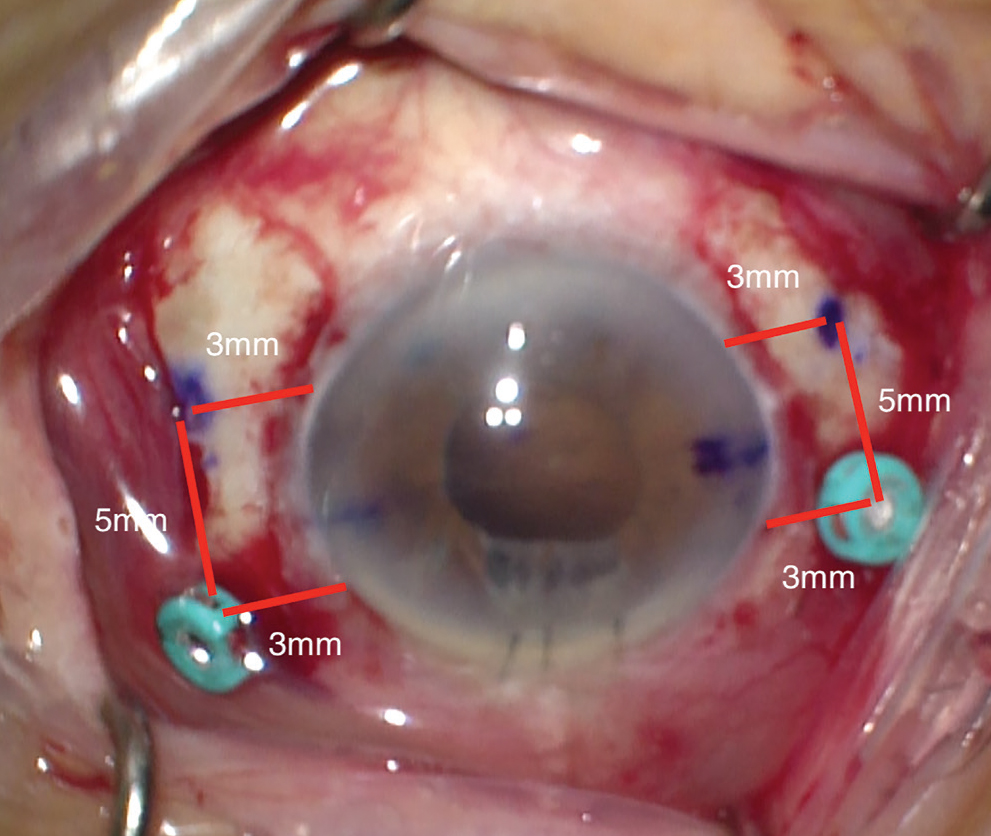 |
| Figure 1. Schematic of the 25-gauge cannula and sclerotomy placement. The corneal limbus is marked at two points, 180 degrees apart, along the horizontal meridian. The 25-g cannulas are placed 3 mm posterior to the limbus. Sclerotomies are made 3 mm posterior to the limbus and 5 mm inferior to the cannulas. Cannulas and sclerotomies are centered around the horizontal meridian. |
The enVista MX60 lens is a hydrophobic acrylic lens, so it’s not susceptible to opacification under gas or air. This makes it a great choice for patients with a history of retinal pathology who may be at risk for future retinal surgery requiring a tamponade.
Threading the lens
Proper placement of the 8-0 GORE-TEX suture through the eyelet is a key step to avoiding lens tilt. We pass the suture down through the islet and then back up and over the optic (Figure 2). We bring both ends of the suture anterior to the haptic to rest on its anterior surface. This orientation must be maintained after the lens is placed inside the eye. If a suture end slips under the haptic, lens tilt will surely happen.
Avoiding suture twisting
It’s paramount to maintain proper superior and inferior orientation of the suture ends while threading through the cannula and sclerotomy. Threading one side of the suture through the sclerotomies before inserting the lens helps with stability.
Once one side is carefully threaded, the lens must be folded carefully while maintaining the orientation of the suture. We do this by folding the IOL in half and tucking the lead optic into the “taco.”
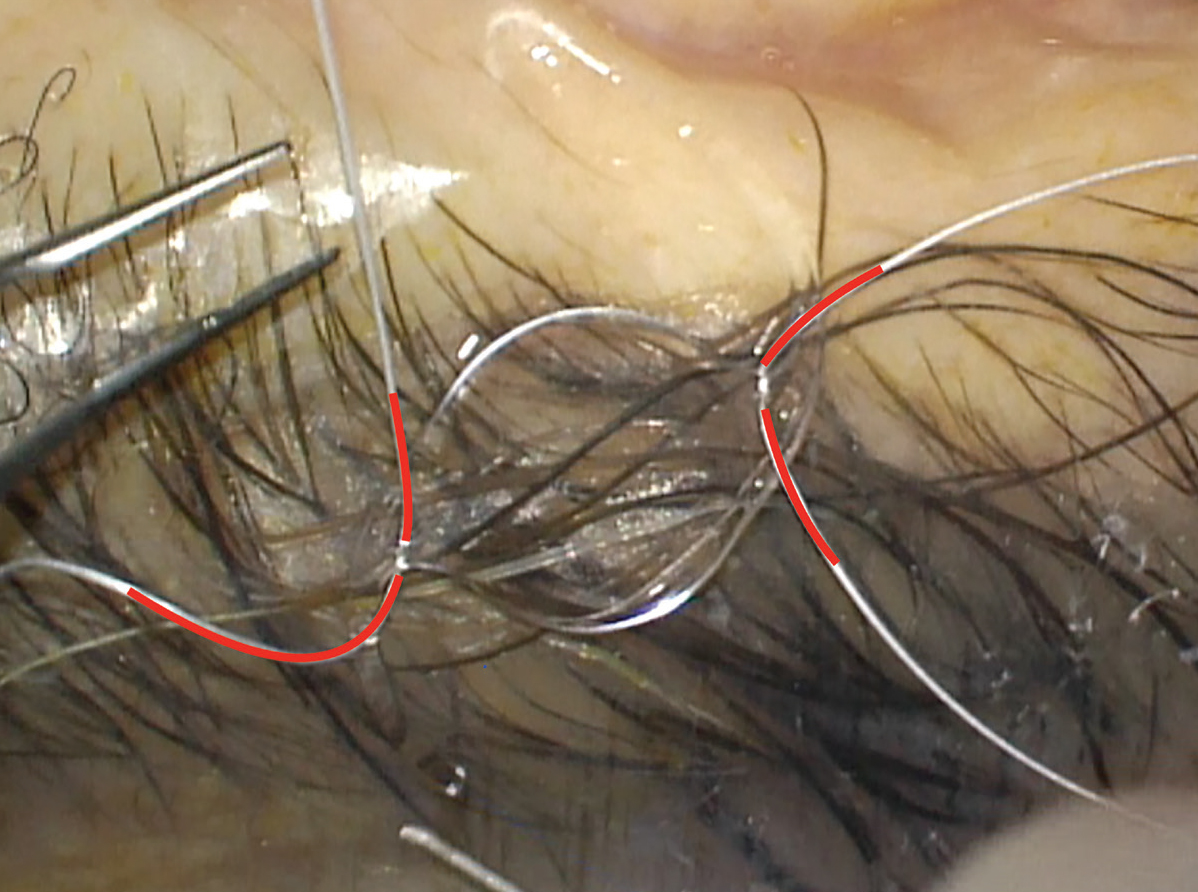 |
| Figure 2. The enVista MX60 lens (Bausch + Lomb) in proper backwards S configuration. Two CV-8 GORE-TEX sutures are passed down through each eyelet and passed back over the haptic. Each end of the suture lies flat on the anterior surface of the haptic. |
The corneal wound must be large enough to smoothly allow for IOL insertion into the eye while maintaining a constant tension on the suture. Once the IOL is in the appropriate position, you can remove the cannula and throw a stabilizing knot to keep the IOL in position. This allows for easier visualization of the optic through the pupillary margin to ensure that the suture is oriented correctly for threading the opposite sclerotomies.
Once the lens is stabilized on both sides (using the first tie of a slipknot or the first throw of a 3-1-1 tie), we recommend using a Sinskey hook or a Lester pusher to displace the iris peripherally and visualize the suture orientation over the haptic and verify the position is appropriate.
Mind the eyelet
It’s important to place minimal tension on the eyelet itself during suture tightening, because not doing so can lead to eyelet tears and lens dislocation. The tension should be just enough that the lens is centered, suture slack is minimal and the lens sits flush to the sclera. You can titrate this by gently pulling the suture loop to gauge its tension.
Bottom line
GORE-TEX-sutured IOL placement using the enVista MX60 along with standard pars plana vitrectomy is a safe, predictable and efficient method for secondary IOL placement. Proper sclerotomy placement, careful suture threading through the eyelet, and consistent suture placement through the sclerotomies are all key steps that, if done properly, will lead to success. RS
REFERENCES
1. Khan MA, Gerstenblith AT, Dollin ML, et al. Scleral fixation of posterior chamber intraocular lenses using GORE-TEX suture with concurrent 23-gauge pars plana vitrectomy. Retina. 2014;34:1477-1480.
2. Parekh P, Green WR, Stark WJ, Akpek EK. Subluxation of suture-fixated posterior chamber intraocular lenses A clinicopathologic study. Ophthalmology. 2007;114:232-237.
3. Khan MA, Gupta OP, Smith RG, et al. Scleral-fixation of intraocular lenses using GORE-TEX suture: Clinical outcomes and safety profile. Br J Ophthalmol. 2016. 100:638-643.




