Take-home points
|
 |
|
Bios Dr. Amarasekera is a clinical assistant professor of ophthalmology at the University of Pittsburgh School of Medicine. Dr. Chhablani is an associate professor at the University of Pittsburgh School of Medicine, specializing in medical retina and vitreoretinal surgery. DISCLOSURES: |
Endoscopic vitrectomy can be an important addition to the retina surgeon’s armamentarium. In ophthalmology, Harvey Thorpe, MD, first described the endoscopic approach in 1934, and then Claude Boscher, MD, and colleagues applied it to vitrectomy in 1981.
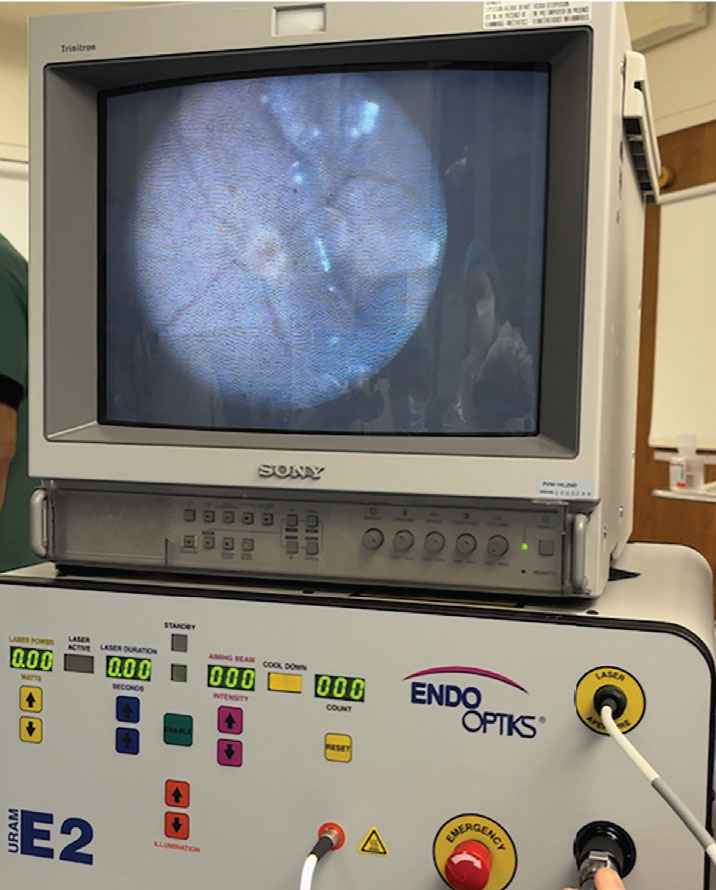
Endoscopic vitrectomy involves use of a coaxial instrument that both provides illumination while capturing an image that’s viewed through a separate monitor rather than a surgical microscope. Commercially available endoscopic viewing vitrectomy systems include the EndoOptiks Ophthalmic Laser Endoscopy System (Beaver Visitec, Figure 1) and the FiberTech Ophthalmic Endoscope (FiberTech). These endoscopes have either rigid or curved probes.1 Available sizes include larger 19-gauge and 20-gauge probes, as well as 23-, 25- and 27-gauge probes that can be used through traditional microsurgical cannulas.
Unlike traditional pars plana vitrectomy that relies on contact or noncontact “top down” viewing systems, the current endoscopic approach doesn’t require clear media or an adequately dilated pupil size.
Advantages of endoscopy
Unique advantages of coaxial illumination include improved visualization of otherwise transparent structures, such as the vitreous and subretinal membranes,2 and the ability to easily magnify an image by moving the endoscope toward it. Further, a hybrid vitrectomy approach uses both traditional PPV in conjunction with an endoscope to allow the greatest range of surgical maneuvers.3
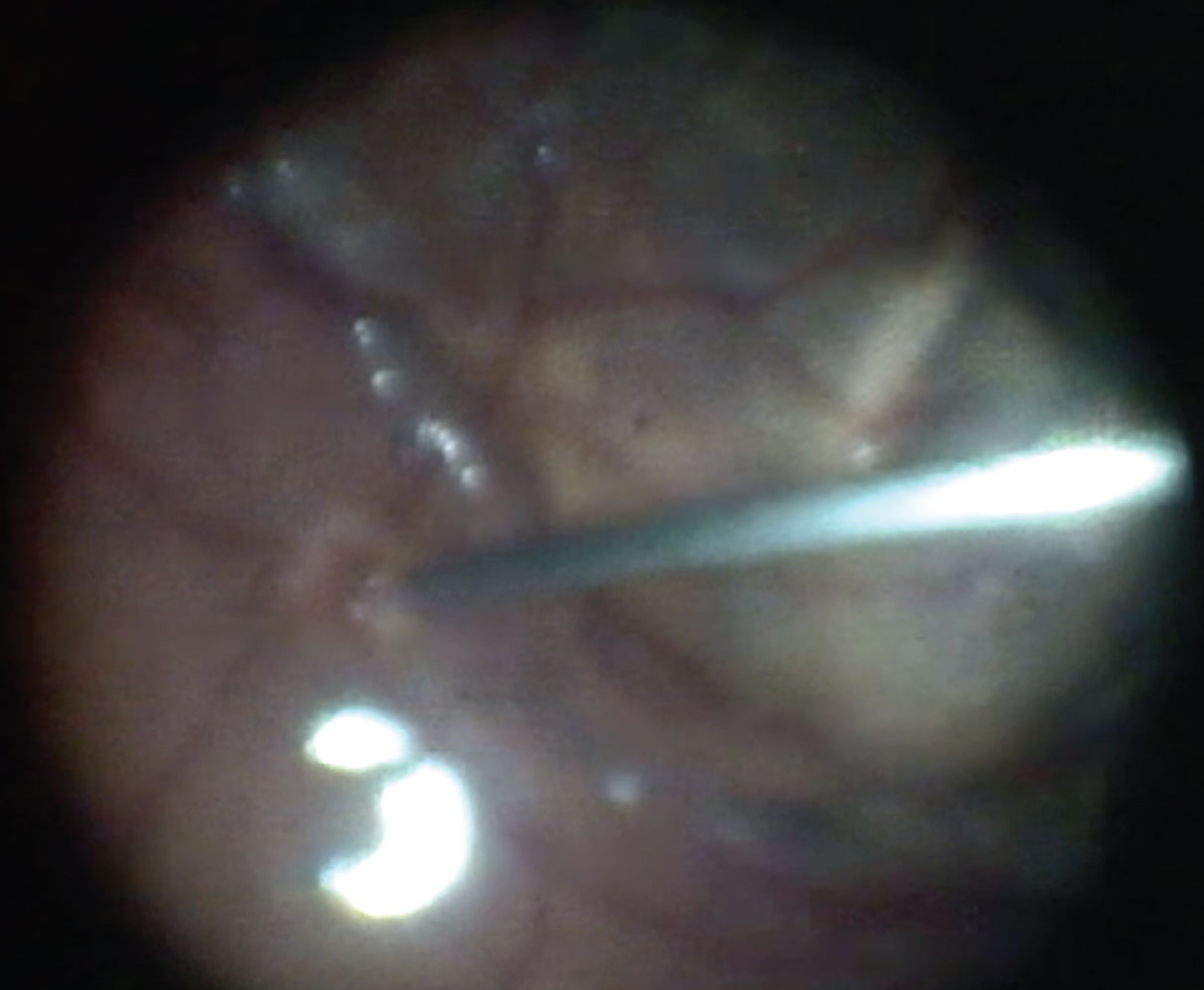
These features bestow advantages of endoscopic vitrectomy in the diagnosis and treatment of complex retinal pathology. For example, endoscopy provides unparalleled access to the anterior vitreous cavity. You can reach difficult-to-access retained lens fragments or anterior proliferative vitreoretinopathy that may otherwise contribute to surgical failure, including cyclitic ciliary body membranes (Figure 2) and contracted anterior edges of prior retinectomies.4
Endoscopy also has benefits when dealing with hazy media. Ocular trauma may result in corneal or lenticular compromise or anterior- or posterior-segment hemorrhage that may delay or limit the use of vitrectomy.
In these cases, traditional PPV may require bringing in an anterior-segment surgeon and donor tissue to use a temporary keratoprosthesis followed by penetrating keratoplasty.5 In such cases, as Radwin Ajlan, MD, and colleagues noted, endoscopy can ultimately reduce time to surgery as well as the duration of retinal surgery.6
Dealing with corneal edema
 |
|
Figure 1. External view of the endoscopic viewing system. |
Likewise, in the setting of corneal edema accompanying endophthalmitis, endoscopic vitrectomy may allow for faster intervention with the ability to perform a more comprehensive diagnostic and therapeutic vitrectomy than the traditional approach.7
Further, endoscopy provides direct visualization of the posterior segment to help determine the visual potential of an eye with corneal opacification. The endoscopic approach allows for a more reliable prognostication to aid in counseling and surgical planning than other imaging modalities, such as ultrasound alone.8
Endoscopy in routine retina cases
However, endoscopy can also be used in routine retinal cases as well (Figure 3). For example, groups have documented the benefits of magnified endoscopic views in the identification of retinal breaks9 and drainage of subretinal fluid in routine retinal detachment repair, as well as in internal limiting membrane peeling for macular holes.10 These procedures also highlight the benefit of endoscopy in circumventing the need for scleral depression for vitrectomy completion.
What’s holding us back?
Despite its obvious benefits, multiple factors have limited the widespread adoption of endoscopic vitrectomy. They include the lack of true stereopsis with existing two-dimensional viewing system and narrow field of view with limited resolution. These anomalies may make it difficult for surgeons to assess distances of intraocular structures and keep the desired focal point in good view.
Additionally, depending on the complexity of the surgical case, some surgeons may prefer, or even require, a bimanual technique. While traditional endoscopic vitrectomy precludes the bimanual technique, use of a chandelier may eliminate this problem.
Perhaps the most commonly cited deterrents of widespread adoption of endoscopic vitrectomy is its steep early learning curve and limited training of vitreoretinal fellows in the endoscopic approach. Therefore, we advocate for a systematic approach to this problem.
Training is lacking
Overall, there’s a paucity of data on the training of vitreoretinal surgeons in the endoscopic approach. Currently in the United States, there are no formal requirements for vitreoretinal fellows in the training of endoscopic vitrectomy techniques. It’s unknown how many programs train fellows in endoscopy and whether faculty often use this approach. As a result, there may be limited formal opportunities for fellows to learn this important skill during their fellowship.
However, endoscopes are often readily available at ophthalmic surgical facilities, especially in those that also do glaucoma procedures given their use in endoscopic cyclophotocoagulation.
How to learn endoscopy
 |
|
Figure 2. Endoscopic view of the vitrectomy probe at the edge of cyclic membrane. |
So, if possible, we encourage trainees to take the initiative to develop endoscopy during their training. A good start is to practice orienting the endoscopic probe in routine cases that don’t necessarily require a endoscopic approach.
Focus the probe outside the eye using the surgical drape or speculum as the focal point. Once inside the eye, posterior pole structures, such as the optic nerve and arcades, can serve as landmarks to orient positioning within the vitreous cavity. The endoscope can be withdrawn slightly as needed to increase the field of view and help with reorientation. Take care to avoid lens touch in phakic eyes.
 |
|
Figure 3. Endoscopic view of the vitrectomy probe being used for fluid-air exchange near the optic disc. |
With time, moving the probe within the eye and lighting tissues adequately will become more facile. Looking ahead, developers of multiple viewing platforms are working to integrate three-dimensional viewing with endoscopy.
Bottom line
As endoscopic vitrectomy continues to evolve, we advocate integrating endoscopic techniques into fellowship training to ultimately provide our patients with the most timely and effective surgical care. RS
REFERENCES
1. Dave VP, Tyagi M, Narayanan R, Pappuru RR. Intraocular endoscopy: A review. Indian J Ophthalmol. 2021;69:14-25.
2. Wong SC, Lee TC, Heier JS, Ho AC. Endoscopic vitrectomy. Curr Opin Ophthalmol. 2014;25:195–206.
3. Kita M, Mori Y, Hama S. Hybrid wide-angle viewing-endoscopic vitrectomy using a 3D visualization system. Clin Ophthalmol. 2018;12:313-317.
4. Rezende FA, Vila N, Rampakakis E. Endoscopy-assisted vitrectomy vs. vitrectomy alone: comparative study in complex retinal detachment with proliferative vitreoretinopathy. Int J Retina Vitreous. 2020;6:34.
5. Sabti KA, Raizada S. Endoscope-assisted pars plana vitrectomy in severe ocular trauma. Br J Ophthalmol. 2012;96:1399-403.
6. Ajlan RS, Desai AA, Mainster MA. Endoscopic vitreoretinal surgery: Principles, applications and new directions. Int J Retina Vitreous. 2019;5:15.
7. Ren H, Jiang R, Xu G, et al. Endoscopy-assisted vitrectomy for treatment of severe endophthalmitis with retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2013;251:1797-1800.
8. Farias CC, Ozturk HE, Albini TA, et al. Use of intraocular videoendoscope examination in the preoperative evaluation of keratoprosthesis surgery to assess visual potential. Am J Ophthalmol. 2014;158:80-86.
9. Yokoyama S, Kojima T, Mori T, et al. Clinical outcomes of endoscope-assisted vitrectomy for the treatment of rhegmatogenous retinal detachment. Clin Ophthalmol. 2017;11:2003-2010.
10. Kita M, Yoshimura N. Endoscope-assisted vitrectomy in the management of pseudophakic and aphakic retinal detachments with undetected retinal breaks. Retina. 2011;31:1347-1351.
24. ClinicalTrials.gov. Study to compare the efficacy and safety of intravitreal APL-2 therapy with sham injections in patients with geographic atrophy (GA) secondary to age-related macular degeneration. Identifier: NCT03525613. https://clinicaltrials.gov/ct2/show/NCT03525613. Updated June 22, 2022. Accessed January 23, 2023.



