 |
 |
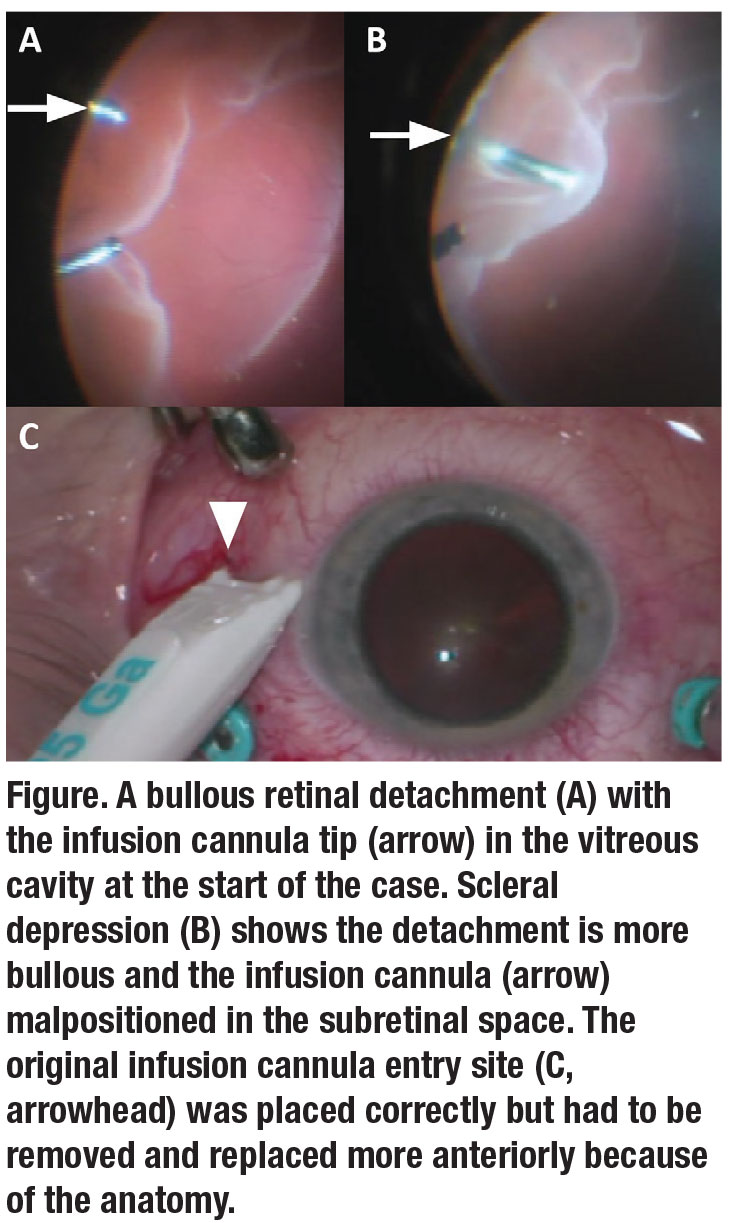
Cannula placement in pars plana vitrectomy is routine, but significant complications may potentially occur with malpositioning. A cannula tip placed in the subretinal (Figure) or suprachoroidal space may cause air or fluid to enter these regions, creating a surgical challenge. Here, we discuss the operative field and explain corrective measures.
The ora serrata is 7 to 8 mm posterior from the limbus, and nasally is 1 mm more anterior than the temporal side due to postnatal growth.1 Some patients may have an anteriorly inserted retina. Cannulas are typically placed around 4 mm from the limbus in phakic patients and 3 to 3.5 mm in pseudophakic patients.
Confirming cannula tip location
Malpositioned superior cannulas typically affect the light pipe and vitrector and are noticeable once you insert the instruments. The retina will move with the instruments. A malpositioned infusion cannula may be more difficult to detect. These techniques can confirm the infusion tip’s location:
Direct visualization using the external light pipe and/or the microscope, indenting the eye with the infusion line as needed to visualize.2,3
When dealing with traumatic cataracts or endophthalmitis, a partially inserted light pipe within the infusion cannula may help determine the cannula tip location. Light from a light pipe within the suprachoroidal space results in a reddish-brown light, while a correctly placed cannula reveals white light.3
Intraoperative malposition
Even if the infusion line is correctly placed at the start of the case, scleral depression, eyelid anatomy or a long sclerotomy tunnel can cause the cannula to shift. The former may cause mechanical malposition or retraction as the eye is rotated or the cannula is torqued. If the infusion cannula is too close to the inferior eyelid, rotating the eye inferiorly may cause the infusion line to contact the lower lid, rotating or retracting the infusion cannula. A long sclerotomy tunnel decreases the length of cannula in the intraocular space and can also cause displacement into the subretinal or suprachoroidal space with only minimal retraction.
 |
With a misplaced infusion line, subretinal infusion fluid can cause iatrogenic breaks, tears or retinal detachment. Subretinal air may make it difficult to flatten the retina. Suprachoroidal infusion of air or fluid may cause a choroidal detachment and present with hypotony.
Fatalities from an air embolus in the lungs or cerebral infarct in conjunction with a patent foramen ovale in the heart have been associated with inadvertent suprachoroidal infusion of air. A porcine model demonstrated that pressurized air from a suprachoroidal infusion tip can enter the vortex veins and systemic circulation.2 To prevent this, some surgeons recommend reconfirming the infusion tip location just before an air-fluid exchange.
Corrective measures
It’s important to identify a misplaced infusion line promptly. Corrective measures include stopping the infusion and repositioning the line either in a different cannula already in place or by removing and replacing the infusion cannula in another location.
Steve Charles, MD, has reported using a micro-vitreoretinal blade to incise any tissue overlying the infusion line. Other techniques include using the smooth forceps to advance a retracted cannula until flush to the sclera, or a 6-mm cannula to help ensure extension of the cannula in the vitreous cavity.
It’s important to constantly monitor the infusion line position and address any concerns for malposition. RS
Surgical Pearl Video: Correcting a malpositioned infusion cannula.
REFERENCES
1. Schepens C, Bahn G. Examination of the ora serrata: Its importance in retinal detachment. AMA Arch Ophthalmol. 1950;44:677-690.
2. Gayer S, Palte H, Albini T, et al. In vivo porcine model of venous air embolism during pars plana vitrectomy. Am J Ophthalmol. 2016;171:139-144.
3. Shoeibi N, Ansari-Astaneh M. A simple method for detecting vitrectomy infusion line position in hazy media, in case of poor visualization. Retina. 2014;34:1707-1709.




