Many of us may not have the luxury of consistently operating with trained fellows or surgical assistants. An important trend in modern-day vitreoretinal surgery has been minimizing dependence on an assistant.
In this regard, foot-pedal-controlled, non-contact, wide-angle viewing systems have been an important technology for independent
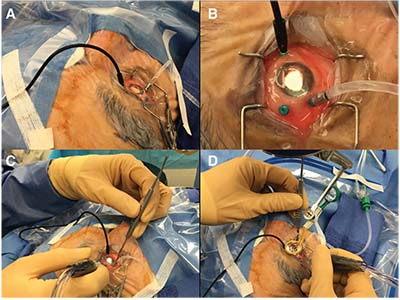 |
| Placement of a chandelier endoilluminator via a pre-existing vitrectomy instrument cannula allows the surgeon to perform simultaneous peripheral vitreous surgical maneuvers and scleral indentation. Key steps are: A) orient the semi-rigid cable like a gooseneck lamp to allow for optimal peripheral illumination and minimize inadvertent misdirection of the chandelier; B) orient the cannulas for unconstrained maneuverability of the active instrument, which facilitates the next two steps: C) simultaneous peripheral vitrectomy; and D) scleral indentation by the surgeon. |
surgery. Scleral indentation-assisted peripheral vitrectomy often still requires an assistant. However, in the absence of a skilled assistant, a chandelier enables a surgeon to indent with one hand and cut vitreous with the other. For routine cases, surgeons may hesitate to create an additional (fourth) sclerotomy for chandelier placement.
Here, Yannek Leiderman, MD, PhD, of Illinois Eye and Ear Infirmary shares a simple but valuable pearl for performing scleral indentation-assisted peripheral vitrectomy without an assistant.
Use Existing Cannulas
This technique involves inserting the chandelier in one of the two already placed open cannulas, reserving the other available cannula for the vitreous cutter held in one hand and freeing the other hand for the scleral depressor. Peripheral vitrectomy and vitreous base shaving do not require a second active instrument. Placing the chandelier in a pre-existing surgical cannula obviates the need for additional sclerotomies and may be performed immediately prior to peripheral vitrectomy.
Here, Dr. Leiderman shares some valuable tips for independent peripheral vitreous surgery.
Gooseneck-like Lamp
Place the chandelier via one of the instrument cannulas with the semi-rigid cable oriented like a gooseneck lamp (Figure A).
This facilitates optimal peripheral illumination and minimizes inadvertent misdirection of the chandelier. Often only a single reorientation of the chandelier to the contralateral hemi-fundus is necessary after the initial six clock-hours of peripheral maneuvers.
Use Nasal Instrument Cannula
The most efficient way to perform pseudophakic peripheral vitrectomy is to place the chandelier in the nasal instrument cannula. Peripheral vitrectomy may be performed circumscribing 360° via the temporal instrument cannula.
To minimize any constraints to movement of the vitrectomy probe, place the port close to the temporal horizontal meridian. Simultaneous scleral indentation and peripheral maneuvers at the temporal horizontal meridian present the greatest challenge when the chandelier is placed in the nasal instrument port. This is most effectively addressed by inserting the scleral depressor into the temporal fornix from above or below the temporal cannula.
Alternate Cannulas
Phakic peripheral vitrectomy may require alternating the chandelier between the nasal and temporal cannulas to minimize passing the vitrectomy probe across the antero-posterior axis of the crystalline lens in removing contralateral peripheral vitreous.
Advantages of Chandelier
A chandelier endoilluminator allows the surgeon to simultaneously perform scleral indentation and use the vitrectomy probe, enabling dynamic and coordinated peripheral surgery that is more controlled and efficient, and may very well confer an improved margin of safety.
Dr. Leiderman’s pearl to place the chandelier in one of the already placed cannulas eliminates the need for an additional sclerotomy for vitreous base shaving. True bimanual intraocular techniques will still require a fourth sclerotomy. I have routinely adopted this simple but efficient tip from Dr. Leiderman to perform vitreous surgery independently. RS
Dr. Hahn is an associate at New Jersey Retina in Teaneck. Dr. Leiderman is associate professor of ophthalmology in the retina service at Illinois Eye and Ear Infirmary, University of Illinois at Chicago.




