Starting treatment for diabetic macular degeneration with bevacizumab (Avastin) step therapy and switching to aflibercept (Eylea) seems to be just as effective for improving and maintaining vision over two years as starting and staying with aflibercept, and carries a substantial cost savings, according to the latest research from the DRCR Retina Network.1
 |
|
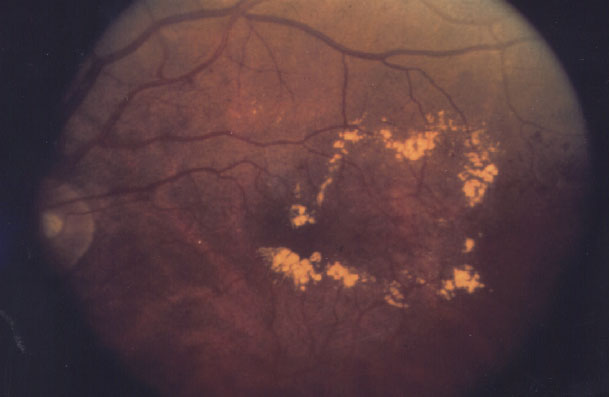
For this, bevacizumab first then aflibercept may be as effective as aflibercept only, but the Protocol AC results aren't generalizable. (NEI photo) |
Reporting results of the Protocol AC study, Chirag D. Jhaveri, MD, and colleagues evaluated 312 eyes in 270 adults who were randomized to aflibercept monotherapy (n=158) or bevacizumab first with a switch to aflibercept later (n=154). Dr. Jhaveri is with Retina Consultants of Austin and the Austin Research Center for Retina in Texas.
“Findings from this trial are particularly relevant given the increasing frequency of insurers mandating step therapy with bevacizumab before the use of other drugs that have been approved by the FDA,” Dr. Jhaveri and colleagues wrote.
Obvious cost issues
Cost is the primary driver in the mandate for step therapy. The study noted that aflibercept is 26 times more expensive than bevacizumab: $1,830 vs. $70 per dose, according to Medicare data the study cited. DRCR Retina Network is developing a manuscript detailing the cost differences between the two treatment strategies, second author Adam R. Glassman, MS, executive director of the Jaeb Center for Health Research in Tampa, Fla., says in comments submitted via e-mail to Retina Specialist. The Jaeb Center organized the trial with the DRCR Retina Network,
Mr. Glassman further explains what this study adds to the literature.
“Prior to this study it was known that in eyes with center-involved diabetic macular edema and starting visual acuity of 20/50 or worse, treatment with aflibercept monotherapy resulted in superior outcomes compared with bevacizumab monotherapy,” Mr. Glassman says. “It, however, was unknown how aflibercept monotherapy compared with bevacizumab first with a switch to aflibercept if the eye condition did not improve sufficiently.
“Based on the results of this study, we found no evidence that visual outcomes over a two-year period were different between aflibercept monotherapy and bevacizumab first with a switch to aflibercept when there was suboptimal response.”
The primary outcome was mean change in visual acuity from baseline over two years (area under the curve): 15±8.5 letters for aflibercept monotherapy vs. 14±8.8 letters for bevacizumab-first (adjusted difference, 0.8 letters; 95% CI, –0.9 to 2.5; p=0.37).
Secondary outcomes
Findings for key secondary outcomes for the aflibercept monotherapy and bevacizumab-first groups, respectively, are:
- Mean change in visual acuity from baseline at two years: 14.7 ±14.5 vs. 15.9 ±12.4, with an adjusted between-group difference of –1.8 letters (95% CI, –4.9 to 1.2).
- 77 percent of eyes in each group had a >10-letter VA gain.
- Mean change in central subfield thickness from baseline to two years: –192 ±143 µm vs. –198 ±160 µm.
The aflibercept monotherapy eyes received fewer injections over two years on average: 14.6 ±4.1 vs. 16.1 ±4.1 injections. The bevacizumab-first eyes received 9.2 ±5.2 bevacizumab injections and 6.9 ±5.8 aflibercept treatments.
Study strengths
Regarding the strengths of the study, Mr. Glassman says, “This was a large National Institutes of Health-funded clinical trial conducted at 54 clinical sites across the United States. The study had strict criteria for retreatment and strict criteria for switching to aflibercept in the bevacizumab-first group, both of which were strongly adhered to during the study. The study also had good retention for a clinical trial in this population.” Except for 14 patients who died, 88 percent of the patients completed the two-year trial.
In BriefApellis Pharmaceuticals reports that pegcetacoplan for treatment of geographic atrophy has shown lesion-growth reductions of 36 and 24 percent for monthly treatment and 29 and 25 percent for bimonthly dosing, according to the latest readouts from the Phase III DERBY and OAKS trials. Twelve-month results of the Phase III GATHER2 trial of another investigative treatment for GA, Zimura (avacincaptad pegol), has shown a 14.3-percent reduction in lesion growth. Trial sponsor Iveric Bio says it plans to submit a New Drug Application with the Food and Drug Administration early next year. Kodiak Sciences reports that the BEACON Phase III study of KSI-301 (tarcocimab tedromer) met its primary endpoint—that is, noninferior change in visual acuity from baseline at 24 weeks compared to aflibercept in patients with macular edema due to retinal vein occlusion. |
“The biggest limitation in this study,” Mr. Glassman adds, “is that we were only able to assess one set of switching criteria. Therefore, we do not know whether the results would have been different if stricter or milder criteria would have been used.”
The study authors wrote that these findings are generalizable only to patients who receive therapy based on the same switching criteria, with the same anti-VEGF agents and using the same treatment algorithm in the Protocol AC trial.
“There are many components that go into deciding what treatment approach is best for an individual patient,” Mr. Glassman says. “This study should allow for more informed decisions by clinicians and patients.”
‘Beyond reproach’
In an accompanying editorial,2 David C. Musch, PhD, MPH, and Emily Y. Chew, MD, wrote, “The design, methods, and conduct of the current trial are beyond reproach.”
They also noted that one of the issues with the bevacizumab-first strategy used in the trial is the frequent follow-up these patients required, which “exceeds what usually takes place in clinical practice.” Dr. Musch and Dr. Chew cited previous DRCR Retina Network research that reported aflibercept wasn’t cost-effective compared to ranibizumab,3 but they added, “it is conceivable that some patients who receive bevacizumab first will have irreversible vision loss that might have been prevented with a prompt switch to aflibercept therapy.”
Dr. Musch is with the University of Michigan and Dr. Chew with the National Eye Institute.
Dr. Jhaveri disclosed financial relationships with Genentech/Roche, Novartis and RegenxBio. Mr. Glassman disclosed relationships with Genentech/Roche and Regeneron Pharmaceuticals. The National Eye Institute and the National Institute of Diabetes and Digestive and Kidney Diseases provided study grants. RS
— Richard Mark Kirkner
REFERENCES
1. Jhaveri CD, Glassman AR, Ferris FL, et al, for the DRCR Retina Network. Aflibercept monotherapy or bevacizumab first for diabetic macular edema. N Engl J Med. 2022;387:692-703.
2. Musch DC, Chew EY. Evidence for step therapy in diabetic macular edema. N Engl J Med. 2022;387:751-752.
3. Ross EL, Hutton DW, Stein JD, Bressler NM, Jampol LM, Glassman AR. Cost-effectiveness of aflibercept, bevacizumab, and ranibizumab for diabetic macular edema treatment: analysis from the Diabetic Retinopathy Clinical Research Network comparative effectiveness trial. JAMA Ophthalmol 2016; 134:888-96.



