| View the Video
|
You see the thick glasses. The globe looks like an egg that is about to burst. Pathologic myopia can make any retina specialist nervous, especially when surgery is indicated. Highly myopic eyes are not uncommon in the retina clinic.
Here, Michael A. Klufas, MD, of Wills Eye Hospital and Tatsuhiko Sato, MD, of Hayashi Eye Hospital in Japan provide their pearls for operating on these challenging eyes.
Anesthesia
Myopic eyes may have a posterior staphyloma. Consider appropriate local anesthesia techniques to prevent inadvertent globe perforation. If you’re not so familiar with retrobulbar block in high-myopia cases, we recommend a peribulbar injection or sub-Tenon’s block.
Reach
Preoperatively, axial length measurement (>30 mm) can be helpful to determine if special instrumentation will be required, such as extra-long forceps. For Alcon products, 23-gauge instruments (or 25-gauge, non-plus) are approximately 1 to 2 mm longer than 25-gauge-plus instruments that have a stiffening sleeve. Longer forceps designed for high-myopia cases are also available (e.g., Dutch Ophthalmic Research Center [DORC] or Synergetics/ Bausch + Lomb Retina).
If you get caught in a pinch and need additional reach from standard forceps, remove the cannula after complete removal of the vitreous gel. Otherwise there is a risk of entry-site associated dialysis. As a last resort, the infusion pressure can be lowered to allow partial compression of the globe, but this causes optical distortions that can make fine macular work difficult.
 |
Macular manipulation
A myopic, tessellated fundus can make visualization of membranes and the internal limiting membrane difficult. Adjuncts, including triamcinolone, brilliant blue or indocyanine green, can enhance visualization. Gently instill and remove these adjuncts because the retinal tissue can be very thin. A sudden jet from an injection or an infusion can cause iatrogenic damage or even a retinal break including, macular hole.
Even for patients with a clinical posterior vitreous detachment, there can often be an element of residual vitreous membranes on the posterior pole as well as mid- to peripheral retina. Triamcinolone can be helpful to identify residual vitreous, which can promote growth of epiretinal membranes and/or proliferative vitreoretinopathy.
Initiating ILM peel at the temporal raphe can minimize mechanical damage to the retinal nerve fibers. In cases with schisis, a fovea-sparing ILM peel may be desirable to limit the chance of progression to full-thickness macular hole.1
For myopic macular holes with and without retinal detachment, inverted ILM flap technique may facilitate anatomic success. If you have to use an autologous ILM flap, perfluorocarbon may be helpful to stabilize the ILM flap even after fluid-air exchange. Other options include autologous retinal graft2 and amniotic membrane3 for refractory macular hole cases.
 |
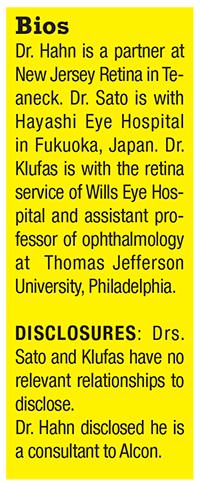
| Figure. A 59-year-old, phakic -20 D myope presented with progressive myopic schisis without macular hole in the left eye (A). Preoperative vision was 20/300. After pars plana vitrectomy with internal limiting membrane peeling and gas tamponade (B), the macular schisis resolved and vision at one-year follow-up after phacoemulsification was 20/60. |
Bottom line
The next time that a high myope is sitting in your examination chair, don’t let that big eye worry you. Use these pearls to formulate the proper preoperative plan and obtain any special instrumentation that may be required in the setting of extreme axial length. Thinking carefully about the goals of surgery and the operative approach in these fragile eyes will minimize iatrogenic complications and maximize success.
REFERENCES
1. Shimada N, Sugamoto Y, Ogawa M, et al. Fovea-sparing internal limiting membrane peeling for myopic traction maculopathy. Am J Ophthalmol 2012;154:693-701.
2. Grewal DS, Mahmoud TH. Autologous neurosensory retinal free flap for closure of refractory myopic macular holes. JAMA Ophthalmol 2016;134:229-30.
3. Rizzo S, Caporossi T, Tartaro R, et al. A human amniotic membrane plug to promote retinal breaks repair and recurrent macular hole closure. Retina (in press).





