 |
|
Bios
Dr. Felfeli is an ophthalmology resident at the University of Toronto. Dr. Grewal is a vitreoretinal surgeon at the University of Toronto. Dr. Mandelcorn is an associate professor of ophthalmology at the University of Toronto. DISCLOSURES: The authors have no relevant financial relationships to disclose. |
Vitreoretinal surgical techniques should be tailored and targeted to the patient’s unique pathology, as well as the surgeons’ preference and experience. While pars plana vitrectomy techniques have improved and direct drainage of subretinal fluid is the more common approach, external needle drainage can be part of a vitreoretinal surgeon’s armamentarium. Here, we present our approach to transcleral external needle drainage, and some of its applications in unique surgical scenarios.
Transcleral drainage: A brief history
Steve T. Charles, MD, first described transscleral drainage of subretinal fluid by using a 5/8-inch, 25-gauge needle during scleral buckling.1 It has since been described with different gauges, ranging from 26- to 28-gauge,2,3 as well as with different types of needles, including a guarded 26-gauge needle4 and a 24-gauge intravenous catheter.5 While this technique was originally described in 1985 with indirect visualization during scleral buckle surgery, recent literature has demonstrated its continued relevance in the era of vitrectomy with direct visualization.
More recently, Peter J. Belin, MD, and colleagues described a case series of 83 eyes with rhegmatogenous retinal detachment (RRD) that underwent external needle drainage during PPV, SB or combined PPV/SB.3 Their findings demonstrated good safety outcomes.
Our preferred approach
Our preferred approach to external needle drainage is to use a 27-gauge, thin-walled TSK needle, guarded with a trimmed 70-buckle sleeve to limit intraocular entry and reduce the risk of retinal incarceration and iatrogenic break (Figure and video). This guarded needle is connected to the active extrusion tubing of the vitrectomy machine.
We perform external drainage in a transconjunctival, transscleral fashion, introducing the needle in the highest portion of the retinal detachment. Here are the key steps in our approach:
- First, viewing externally, engage the conjunctiva and sclera.
- Under direct visualization, with the needle tangential, depress the sclera to confirm the needle’s location.
- Orient the needle in a more perpendicular fashion and slowly advance it until it’s visualized in the subretinal space.
- Actively aspirate the SRF in a slow and controlled fashion using low active vacuum.
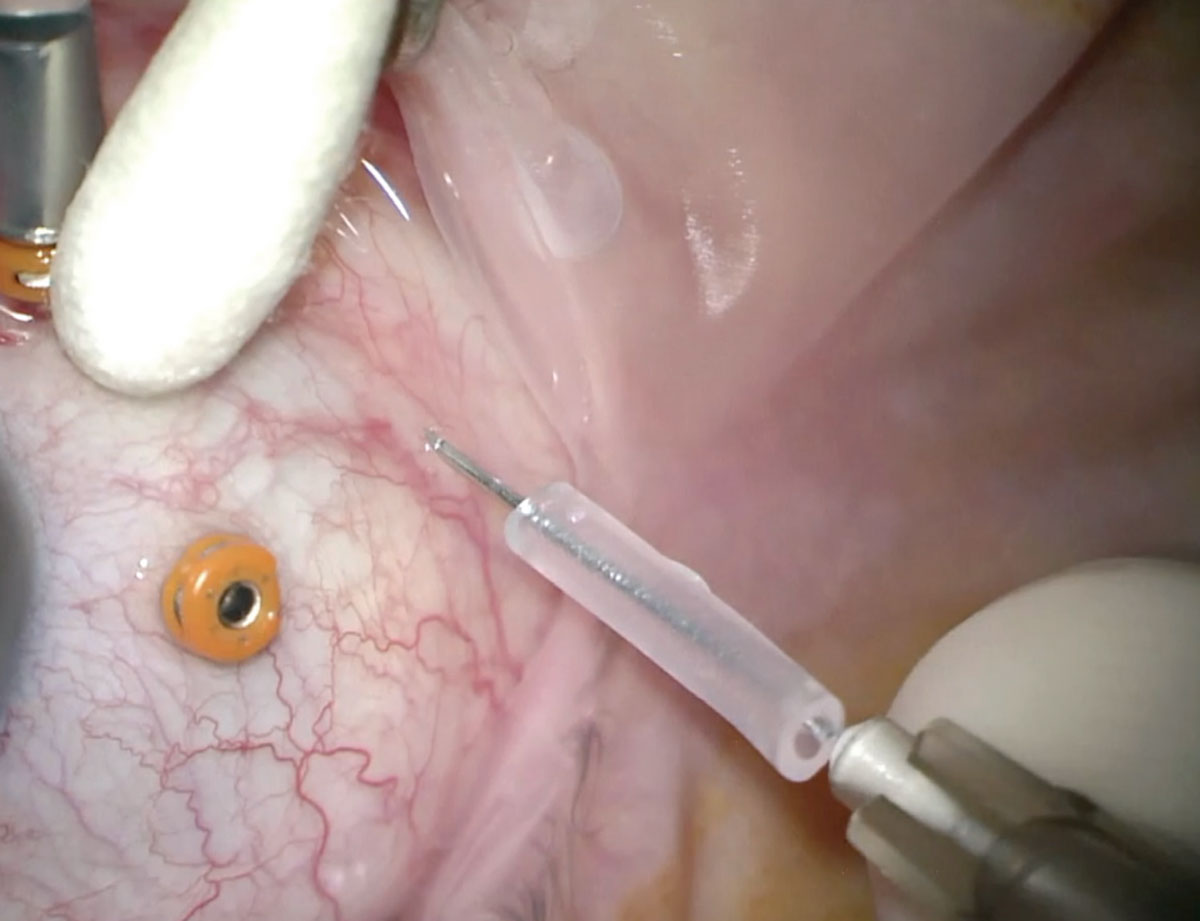 |
| Our preferred approach to external needle drainage is to use a 27-gauge, thin-walled TSK needle, guarded with a trimmed 70-buckle sleeve. |
In cases of subretinal biopsy, the guarded needle can be attached to a syringe which can passively aspirate the SRF directly into the syringe.
Here, we summarize some of our favorite applications of external needle drainage.
1. Very bullous retinal detachment
The presentation of individual RRDs can vary significantly. Very bullous and mobile retinal detachments present a unique challenge. One challenge is the occurrence of iatrogenic retinal breaks during vitrectomy cutting, which can complicate the repair and increase the risk of anatomical failure and proliferative vitreoretinopathy.
Additionally, the vitreous overlying very mobile retina may be difficult to remove completely. In these cases, we like to use external needle drainage early on to flatten the retina. This creates a more controlled surgical setting by reducing the risk of iatrogenic retinal breaks, enabling a more complete removal of adherent vitreous and facilitating membrane removal and macular peeling as required.
2. RRDs with small, anterior retinal breaks
The varying nature and location of retinal breaks can require different approaches for optimal repair. Small, very anterior retinal breaks present a particular challenge. Complete drainage of SRF from the break itself can be challenging, especially in a phakic setting. Yet, drainage of SRF is important to apply optimal laser retinopexy to the break and achieving good fill with gas or oil.
Posterior drainage retinotomies are an option in this setting. However, they carry additional risks, including PVR. Perfluorocarbon is another option, but it introduces significant cost and risk of subretinal migration. External needle drainage is an effective, cost-saving option for reattaching the retina in cases of small anterior retinal breaks.
 |
3. Drainage during chandelier-assisted scleral buckle/combined SB-vitrectomy
External drainage during SB carries the risk of choroidal hemorrhage and retinal incarceration, which can carry significant morbidity. External needle drainage under direct visualization may reduce this risk compared with conventional external cut-down because it enables an improved view of the needle tip and a more controlled flow.
External needle drainage in this setting can be performed in combination with chandelier illumination and visualization with the operating microscope.6 Chandelier illumination is well-suited for external needle drainage when direct visualization is available and careful drainage of subretinal fluid can be performed in a controlled way, as the accompanying video shows.
4. Prevention of underfill of oil tamponade in RRDs
The accompanying video demonstrates two scenarios in which external needle drainage can prevent the underfilling of oil tamponade in RRDs. They are:
• Choroidal effusion. Silicone oil tamponade is commonly used for chronic RRDs and complex retinal detachments. The concern about oil underfill in RRDs with choroidal detachment can be an issue as it may lead to failure and redetachment.
Using the guarded needle, the choroidal detachment can be drained to restore the vitreous volume and ensure a full fill of silicone oil at the end of the case. We’ve found that using this maneuver is best after the fluid-air exchange. We usually increase the air pressure and then place a guarded needle on an open syringe with no plunger to allow for passive egress of the choroidal effusion.
• RD with macrocysts. Chronic RDs can be associated with macrocysts that usually resolve spontaneously postoperatively after tamponade. In cases of large cysts, this can result in silicone oil underfill. To maintain the integrity of the inner retina, these cysts can be drained and “popped” sequentially with an external needle that can be placed in the subretinal space.
10 essential applications of external needle drainage in vitreoretinal surgery 1. Very bullous retinal detachment 2. Rhegmatogenous retinal detachment with small, anterior retinal breaks 3. Drainage during chandelier-assisted scleral buckle/combined scleral buckle-vitrectomy 4. Prevention of underfill of oil tamponade in RRDs with choroidals 5. Subretinal gas or air 6. Lysing a subretinal band 7. Draining a suprachoroidal hemorrhage 8. Tractional retinal detachments 9. RD without a definitive break 10. Exudative RD and subretinal biopsy |
5. Subretinal gas or air
This is a rare, challenging situation that may be encountered intraoperatively or after inadvertent subretinal injection of gas during pneumatic retinopexy.7 It may be challenging to remove subretinal air, particularly if it’s extensive, because it may become sequestered quite anteriorly at the retinal insertion to the pars plana.
By placing a guarded needle in the subretinal space, these bubbles of air or gas can easily be aspirated, either actively or passively, without the need to create large retinotomies for removal. External needle drainage is an elegant way to debulk subretinal air or gas (Video).
 |
6. Lysing a subretinal band
Subretinal PVR and bands may limit retinal reattachment and are challenging to repair given their location. With large retinal breaks or in the setting of retinectomy, these can be accessed more directly and removed. In the absence of adjacent retinal breaks, however, various approaches have been described, including creating retinotomies near or overlying the band, cutting the band and/or removing it through such retinotomies.8
Retinotomies in the setting of pre-existing PVR carry the risk of recurrence. An external needle approach in select cases is an option to facilitate direct lysis of subretinal bands without creating retinal breaks. Once the guarded needle is placed in the subretinal space, the sharp tip of the needle can be used to cut the subretinal band and separate it, effectively eliminating the traction. While it isn’t possible to remove the band in this fashion, once cut, the traction is released, and removal may not be necessary.
7. Draining a suprachoroidal hemorrhage
Suprachoroidal hemorrhage is a dreaded surgical complication and makes access to the vitreous cavity problematic for vitrectomy surgery. Our strategy for addressing a suprachoroidal hemorrhage is to use an external drainage needle to remove the blood as we’ve previously described (Video).9
8. Tractional retinal detachments
Tractional diabetic RDs are often challenging to repair. Retinal breaks, if present, may be difficult to localize, particularly in the setting of extensive fibrovascular proliferation and vitreous hemorrhage. Further, complete and careful removal of preretinal proliferative membranes is essential to success, although it can be challenging with a mobile retina without counter-traction.
As in the very bullous RD, external needle drainage in this setting creates a more controlled situation. Once the SRF is debulked, the retina lies in a more physiological position. This improves visualization and the ability to identify small occult retinal breaks, and it can facilitate safer and more complete dissection of preretinal membranes (Video).
 |
9. RD without a definitive break
A small portion of retinal detachments may present without a definite retinal break.10 One option is to create a posterior retinotomy to drain the subretinal fluid and reattach the retina.
In our experience, however, external needle drainage is a very valuable option in this setting because we can drain the subretinal fluid through the guarded needle, followed by air exchange with or without laser retinopexy of all suspicious areas of retinal break without inadvertently creating or enlarging any occult microbreaks during the air exchange (Video).
10. Exudative RD and subretinal biopsy
Exudative RDs are uncommon and can present challenging surgical scenarios. In select cases of exudative detachment, diagnostic or therapeutic drainage of SRF may be indicated or needed. Drainage retinotomy in this setting can be problematic given the absence of pre-existing retinal breaks and potentially elevated risk of PVR and redetachment. External needle drainage is an elegant solution in this setting to obtain SRF for diagnostic testing and to reattach the retina (Video).
Bottom line
Overall, we believe that external needle drainage is a valuable skill–with a short learning curve–in vitreoretinal surgery. It can be a useful approach in a variety of surgical scenarios including RRD cases (bullous detachments, and small and anterior breaks), when performing scleral buckle, preventing underfilling when using oil tamponade, addressing subretinal gas or air, lysing a subretinal band and draining a suprachoroidal hemorrhage, and for tractional RRDs, detachments with no definitive break and subretinal biopsy in exudative detachments. RS
REFERENCES
1. Charles ST. Controlled drainage of subretinal and choroidal fluid. Retina. 1985;5:233-234.
2. Jaffe GJ, Brownlow R, Hines J. Modified external needle drainage procedure for rhegmatogenous retinal detachment. Retina. 2003;23:80-85.
3. Belin PJ, Mundae R, Tzu JH, Chang E, Parke DW. External drainage of subretinal fluid during rhegmatogenous retinal detachment repair. Retina. 2021;41:1828-1832.
4. Kitchens JW. Modified external needle drainage of subretinal fluid in the management of rhegmatogenous retinal detachment using a “guarded needle” approach. Arch Ophthalmol. 2011;129:949-951.
5. Peng J, Zhang Q, Jin H, Fei P, Zhao P. A modified technique for the transconjunctival and sutureless external drainage of subretinal fluid in bullous exudative retinal detachment using a 24-G IV catheter. Ophthalmologica. 2017;238:179-185.
6. 7. Haug SJ, Jumper JM, Johnson RN, Mcdonald HR, Fu AD. Surgical technique chandelier-assisted external subretinal fluid drainage in primary scleral buckling for treatment of rhegmatogenous retinal detachment. Retina. 2016;36:203-205.
7. Seamone ME, Lewis DR, Almeida D, Choudhry N, Rishi Gupta § R. Massive subretinal gas after vitrectomy surgery: Mechanism and management. Retin Cases Brief Rep. 2019;13:266-268.
8. Lewis H, Aaberg TM, Abrams GW, McDonald HR, Williams GA, Mieler WF. Subretinal membranes in proliferative vitreoretinopathy. Ophthalmology. 1989;96:1403-1415.
9. Mandelcorn ED, Kitchens JW, Fijalkowski N, Moshfeghi DM. Active aspiration of suprachoroidal hemorrhage using a guarded needle. Ophthalmic Surg Lasers Imaging Retina. 2014;45:150-152.
10. Salicone A, Smiddy WE, Venkatraman A, Feuer W. Management of retinal detachment when no break is found. Ophthalmology. 2006;113:398-403.




