 |
|
Bios Dr. Felfeli is an Dr. Mandelcorn is an associate professor of ophthalmology at the University of Toronto. DISCLOSURES: The authors have no relevant financial disclosures. |
The eye, often referred to as a window to the soul, has become increasingly recognized as a window into the brain and its health. In this context, retinal imaging is emerging as a powerful tool to study the early signs of neurodegenerative diseases.
Probing into this frontier has the potential to reshape our understanding and potentially enhance the early detection and monitoring of disorders such as Alzheimer’s disease, Parkinson’s disease and multiple sclerosis.
The retina mirrors pathological processes in the central nervous system, presenting an opportunity for noninvasive imaging of neuronal and vascular structures. With advanced imaging techniques such as optical coherence tomography and OCT angiography, researchers have been able to detect early signs of neurodegenerative diseases.
A revolution for early intervention
Early detection of neurodegenerative diseases through retinal imaging could revolutionize the way we approach these conditions. Early intervention strategies can be designed based on retinal findings, potentially slowing the progression of these diseases and improving patients’ quality of life.
Technological innovations and collaborations across different disciplines are propelling the research in retinal imaging. With the integration of advancements such as machine learning algorithms for image analysis and more sophisticated imaging techniques, retinal imaging holds promise for providing even deeper insights into neurodegenerative diseases.
Despite the promise of retinal imaging, challenges exist for its use to diagnose neurodegenerative diseases. They include developing standardized protocols, understanding the complexity of retinal changes and establishing specificity of retinal changes for each disease. Moreover, ethical considerations surround early diagnosis and its potential psychological impact on patients.
Alzheimer’s disease
 |
|
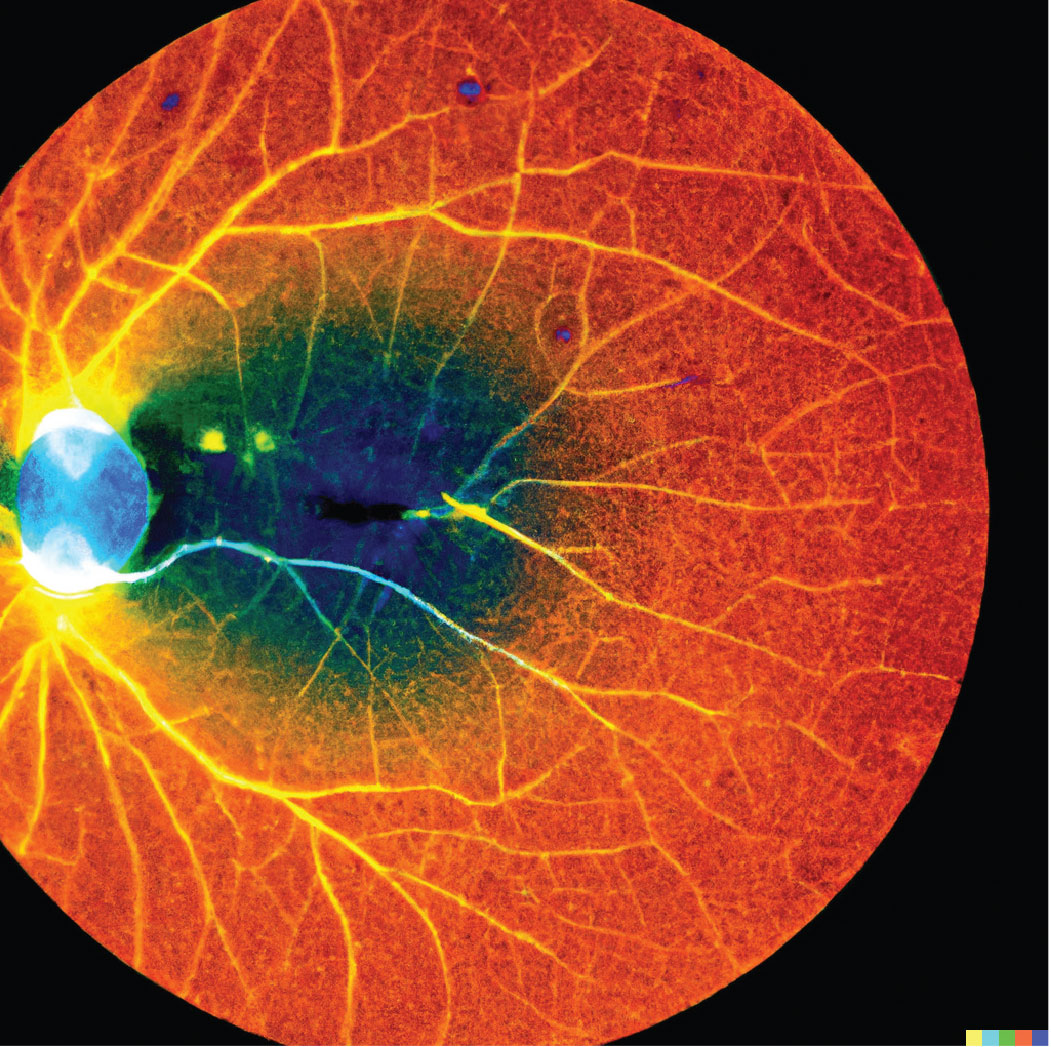
An OpenAI.DALL.E generated image based on the role of retinal imaging as a biomarker for neurodegenerative diseases. |
As the most common cause of dementia, Alzheimer’s disease presents a formidable challenge to clinicians and researchers alike due to its insidious onset, progressive course and absence of definitive diagnostic tests in the early stages. The disease is characterized pathologically by the accumulation of amyloid-beta plaques and neurofibrillary tangles in the brain. Intriguingly, these pathological hallmarks have been identified in the retinas of Alzheimer’s patients, making retinal imaging a potential noninvasive avenue for early detection.1,2
Retinal amyloid imaging can potentially detect Alzheimer’s disease before the onset of significant cognitive symptoms, enabling earlier intervention and monitoring.3 OCTA has revealed significant vascular alterations in the retinas of Alzheimer’s patients, further supporting the role of retinal imaging in early Alzheimer’s detection.4
Parkinson’s disease
Parkinson’s disease, a progressive neurodegenerative disorder primarily affecting the motor system, presents unique challenges for early diagnosis and monitoring due to its heterogeneous presentation and the absence of definitive diagnostic tests. Here again, the retina may offer valuable insights.
Retinal changes in Parkinson’s disease include reduction in retinal nerve fiber layer thickness, macular thinning and changes in foveal pit morphology, likely reflecting the broad neurodegenerative process of this disease.5-7
Imaging techniques focusing on retinal dopaminergic cells—particularly amacrine cells—could provide additional biomarkers for early detection and monitoring of disease progression.8-10
Multiple sclerosis
 |
MS, a chronic inflammatory and neurodegenerative disease marked by autoimmune-mediated demyelination of CNS neurons, represents another neurodegenerative condition for which retinal imaging has shown potential as a diagnostic and monitoring tool. The link between MS and ocular pathology, notably optic neuritis, has long been recognized. Now, with the availability of high-resolution retinal imaging, the relationship between the retina and broader neurodegenerative processes in MS is becoming clearer.
OCT has revealed RNFL thinning in MS patients, independent of optic neuritis, pointing toward a broader neurodegenerative process at play.11
Retinal changes observed with OCT have been correlated with MRI measures of brain atrophy and clinical disability in MS patients, bolstering the case for retinal imaging as a noninvasive surrogate for neurodegeneration in MS.12-14
Challenges and future prospects
The promise of retinal imaging as a biomarker for neurodegenerative diseases is indeed compelling, but as with any emerging field, it’s not without challenges and potential controversies. One critical hurdle is establishing standardized protocols for retinal imaging and interpretation, necessary for ensuring consistent and valid findings. This step is essential given the diversity of OCT devices and imaging techniques, without which inconsistencies could undermine the tool’s efficacy.15
A second challenge involves understanding the complex relationship between
retinal changes and neurodegenerative diseases. The role these changes play, whether causative, epiphenomenal or reflective of common neurodegenerative processes, requires further research. Similarly, establishing the sensitivity and specificity of retinal changes for each disease is needed, given the overlapping clinical features and risk factors in neurodegenerative diseases.
Retinal imaging biomarkers of neurodegenerative diseaseAlzheimer’s disease: Retinal amyloid imaging can detect disease before significant cognitive symptoms appear and optical coherence tomography angiography reveals associated retinal vascular alterations. Parkinson’s disease: Retinal changes include retinal nerve fiber layer thinning and macular changes, offering potential early indicators. Multiple sclerosis: OCT reveals RNFL thinning, which correlates with brain atrophy and clinical disability. |
Bottom line
Novel techniques, coupled with machine learning for image analysis, are providing more detailed retinal examinations and sophisticated data interpretation. This progress, however, should be tempered with ethical considerations related to early diagnosis, including potential psychological impacts on patients and treatment decision implications.
As we continue to navigate these challenges, the future of retinal imaging in neurodegenerative diseases looks promising. By viewing the retina not just as a window to the brain but as an integral part of the neurological landscape, we stand to gain invaluable insights into these complex diseases and develop innovative strategies to improve patient care. RS
REFERENCES
1. Lee S, Jiang K, McIlmoyle B, et al. Amyloid beta immunoreactivity in the retinal ganglion cell layer of the Alzheimer’s eye. Front Neurosci. 2020;14:758.
2. Snyder PJ, Johnson LN, Lim YY, Santos CY, Alber J, Maruff P, Fernández B. Nonvascular retinal imaging markers of preclinical Alzheimer’s disease. Alzheimers Dement (Amst). 2016;4:169-178.
3. Koronyo Y, Biggs D, Barron E, et al. Retinal amyloid pathology and proof-of-concept imaging trial in Alzheimer’s disease. JCI Insight. 2017;2:e93621.
4. Hui J, Zhao Y, Yu S, Liu J, Chiu K, Wang Y. Detection of retinal changes with optical coherence tomography angiography in mild cognitive impairment and Alzheimer’s disease patients: A meta-analysis. PLoS One. 2021;16:e0255362.
5. Huang L, Zhang D, Ji J, Wang Y, Zhang R. Central retina changes in Parkinson’s disease: A systematic review and meta-analysis. J Neurol. 2021;268:4646-4654.
6. Pilat A, McLean RJ, Proudlock FA, et al. In vivo morphology of the optic nerve and retina in patients with Parkinson’s disease. Invest Ophthalmol Vis Sci. 2016;57:4420-4427.
7. Satue M, Seral M, Otin S, et al. Retinal thinning and correlation with functional disability in patients with Parkinson’s disease. Br J Ophthalmol. 20141;98:350-355.
8. Ortuño-Lizarán I, Sánchez-Sáez X, Lax P, et al. Dopaminergic retinal cell loss and visual dysfunction in Parkinson disease. Ann Neurol. 2020;88:893-906.
9. Lee JY, Martin-Bastida A, Murueta-Goyena A, et al. Multimodal brain and retinal imaging of dopaminergic degeneration in Parkinson disease. Nat Rev Neurol. 2022;18:203-220.
10. Moons L, De Groef L. Multimodal retinal imaging to detect and understand Alzheimer’s and Parkinson’s disease. Curr Opin Neurobiol. 2022;72:1-7.
11. Frohman EM, Fujimoto JG, Frohman TC, Calabresi PA, Cutter G, Balcer LJ. Optical coherence tomography: A window into the mechanisms of multiple sclerosis. Nat Clin Prac Neurol. 2008;4:664-675.
12. Burkholder BM, Osborne B, Loguidice MJ, et al. Macular volume determined by optical coherence tomography as a measure of neuronal loss in multiple sclerosis. Arch Neurol. 2009;66:1366-1372.
13. Saidha S, Al-Louzi O, Ratchford JN, et al. Optical coherence tomography reflects brain atrophy in multiple sclerosis: A four-year study. Ann Neurol. 2015;78:801-813.
14. Martinez-Lapiscina EH, Arnow S, Wilson JA, et al. Retinal thickness measured with optical coherence tomography and risk of disability worsening in multiple sclerosis: A cohort study. Lancet Neurol. 2016;15:574-584.
15. Yanagihara RT, Lee CS, Ting DS, Lee AY. Methodological challenges of deep learning in optical coherence tomography for retinal diseases: Areview. Transl Vis Sci Technol. 2020;9:11.




