 |
Bios Dr. Tanaka is an ophthalmologist in the department of ophthalmology and micro-technology at Yokohama City University, Japan. Dr. Kadonosono is a professor and chair of the department of ophthalmology and micro-technology at Yokohama City University.
|
The intraretinal artery cannulation method for injecting tissue plasminogen activator into the central retinal artery may be indicated in cases with early presentation of central retinal artery occlusion.
Patient-level meta-analyses have suggested that early systemic thrombolysis with tissue plasminogen activator (tPA) may be beneficial for management of CRAO embolism or thrombosis when administered within 4.5 hours.1
Although the European Assessment Group for Lysis in the Eye (EAGLE) trial, which evaluated early intra-arterial delivery of fibrinolysis, didn’t demonstrate improved visual outcomes,2 others have suggested that conservative treatments are futile1 and that intra-arterial tPA may have some promise.3 A case series of 13 patients undergoing intraretinal artery cannulation reported no serious surgical complications, with the exception of one case of postoperative vitreous hemorrhage.4
Here, we share our approach to intraretinal artery cannulation for injection of tPA in cases of CRAO.
Patient selection and preoperative considerations
Ideal candidates for our approach to intraretinal artery cannulation are patients who have nonarteritic CRAO, visual acuity better than light perception but not exceeding 20/40 and an onset of symptoms within 48 hours before the initial consultation, preferably sooner.
Those not suitable for the procedure are patients with a history of stroke or head injury within the last three months, those with uncontrolled hypertension and systolic blood pressure >185 mmHg, have a bleeding disorder or have poor baseline visual acuity due to conditions including macular degeneration and proliferative diabetic retinopathy.
One of the most important factors in determining outcomes is likely the delay between symptom onset to reestablishment of perfusion. Because of this, patients should go to the operating room as soon as possible.
Given the risks associated with use of thrombolytic agents, all patients should be informed about the possibility of intracerebral hemorrhage in advance.5 Preoperative systolic blood pressure should be maintained in the 120-to-150-mmHg range or lower, so administering antihypertensive drugs may be indicated to minimize risk of intraoperative bleeding.
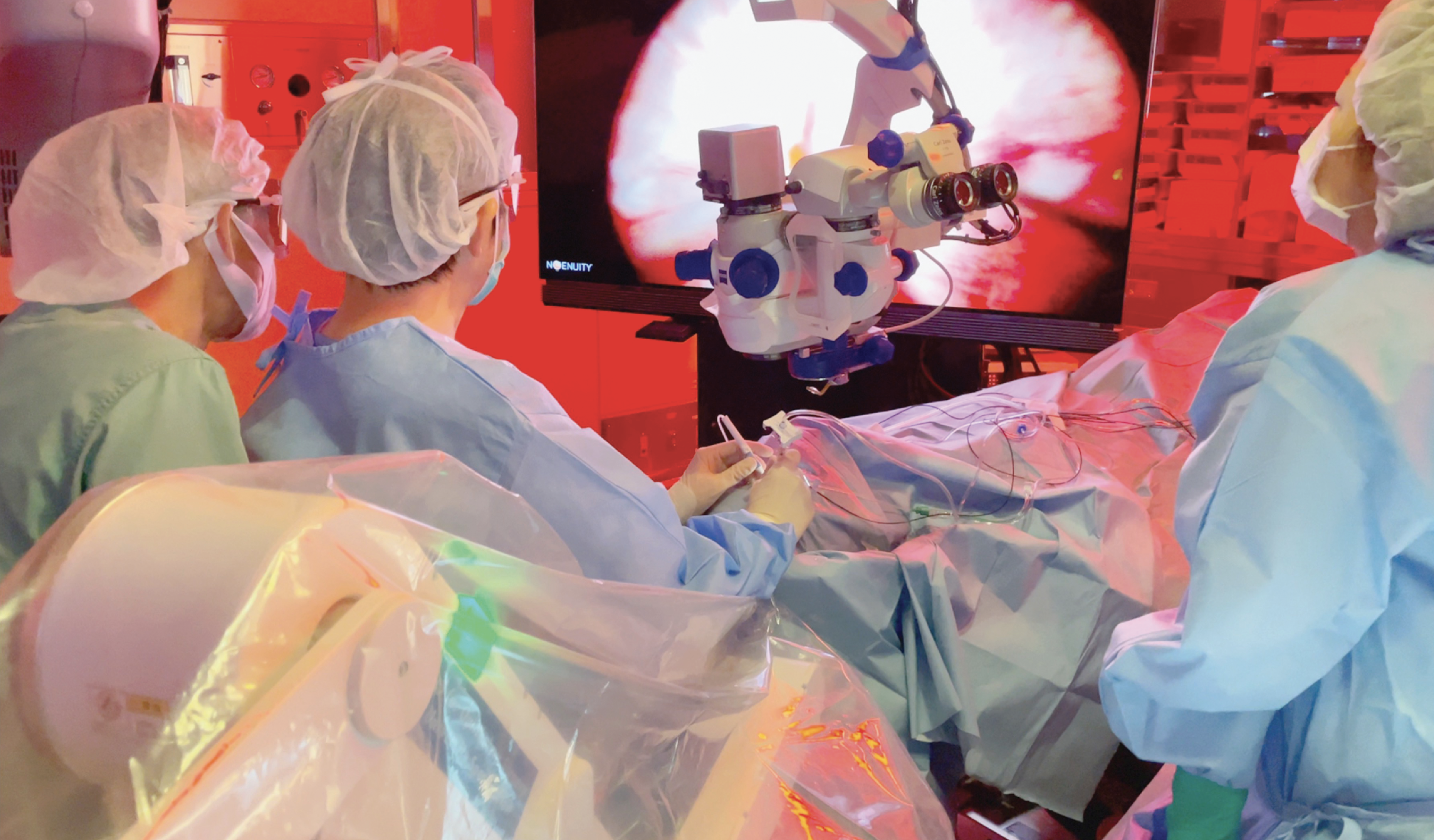 |
| Figure 1. Operating room layout of the three-dimensional heads-up microscope during pars plana vitrectomy for performing the intraretinal artery cannulation for injection of tissue plasminogen activator into the central retinal artery. |
Surgical approach
We use the three-dimensional heads-up microscope during pars plana vitrectomy (Figure 1). This technique is done using a 48-gauge microneedle (Nono cannula, MedOne Corp.) following a core vitrectomy (Figure 2A).2 During this procedure, the central retinal artery is punctured at the bifurcation where it enters the optic nerve (Figure 2B).
After puncture, 0.4 mL of tPA in a solution containing 50 μg/0.1 mL (200 μg total dose) is administered, and the perfusion is maintained for approximately three minutes. At our institution, we infuse the tPA at a pressure of up to 80 psi using the Constellation Viscous Fluid Control Pak syringe (Alcon).
Once the injection is completed, a color change of the vessels to white confirms the tPA has been successfully injected. Pay attention to achieve hemostasis (Figure 2C), which may be done using a soft-tipped cannula to aspirate any bleeding at the puncture site (Figure 2D).
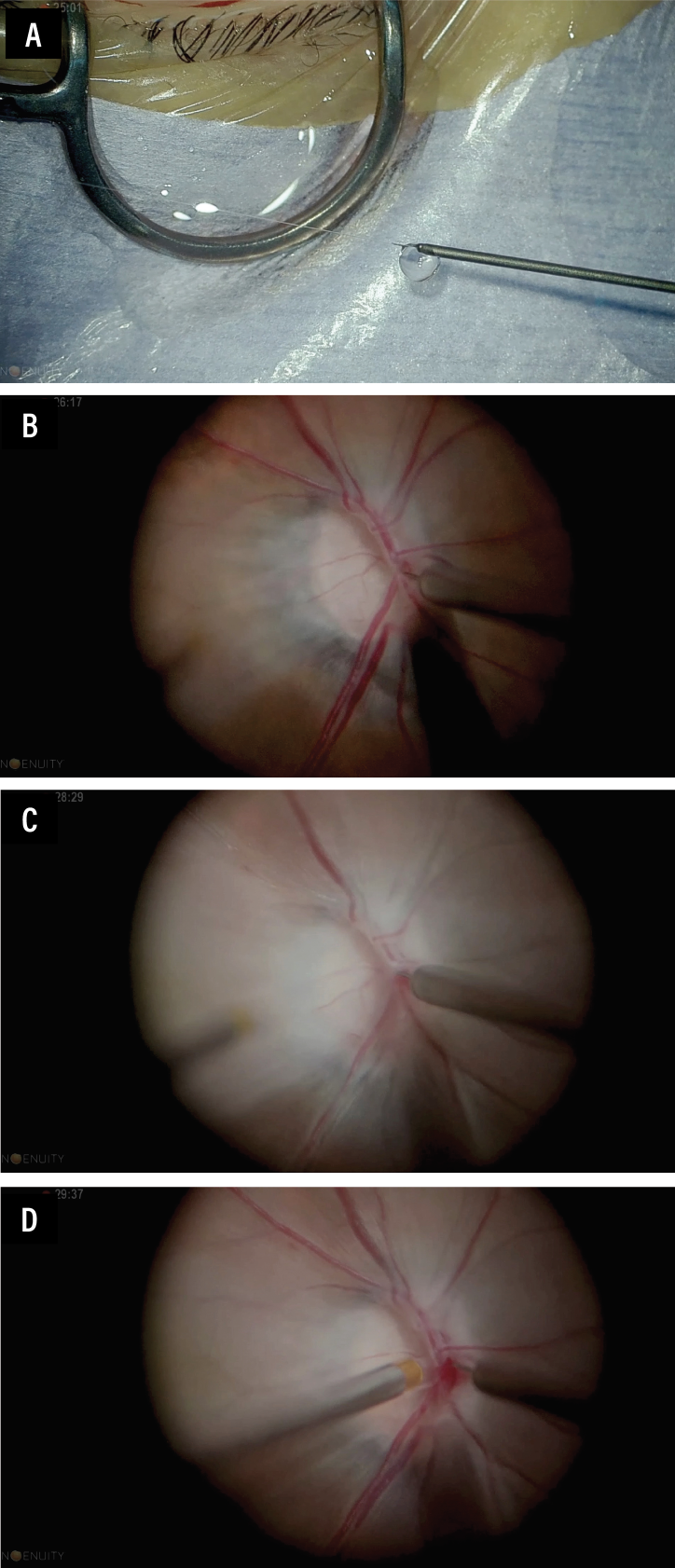 |
| Figure 2. Intraoperative views of our approach to intraretinal artery tissue plasminogen activator (tPA) injection. A) Using a 48-gauge microneedle, the tPA is visualized coming out of the cannula. B) The central retinal artery is punctured at the bifurcation where it enters the optic nerve. C) The vessels change color to white, confirming successful tPA injection. D) Once the injection is completed, any bleeding is aspirated using a soft-tipped cannula bimanually. |
If you don’t notice any improvement in retinal perfusion, you may inject tPA again. However, an increasing number of punctures will result in greater damage to the vessel wall, so achieving hemostasis may become more difficult.
A fluid-air exchange concludes the procedure. Figure 3 depicts the outcomes of a case.
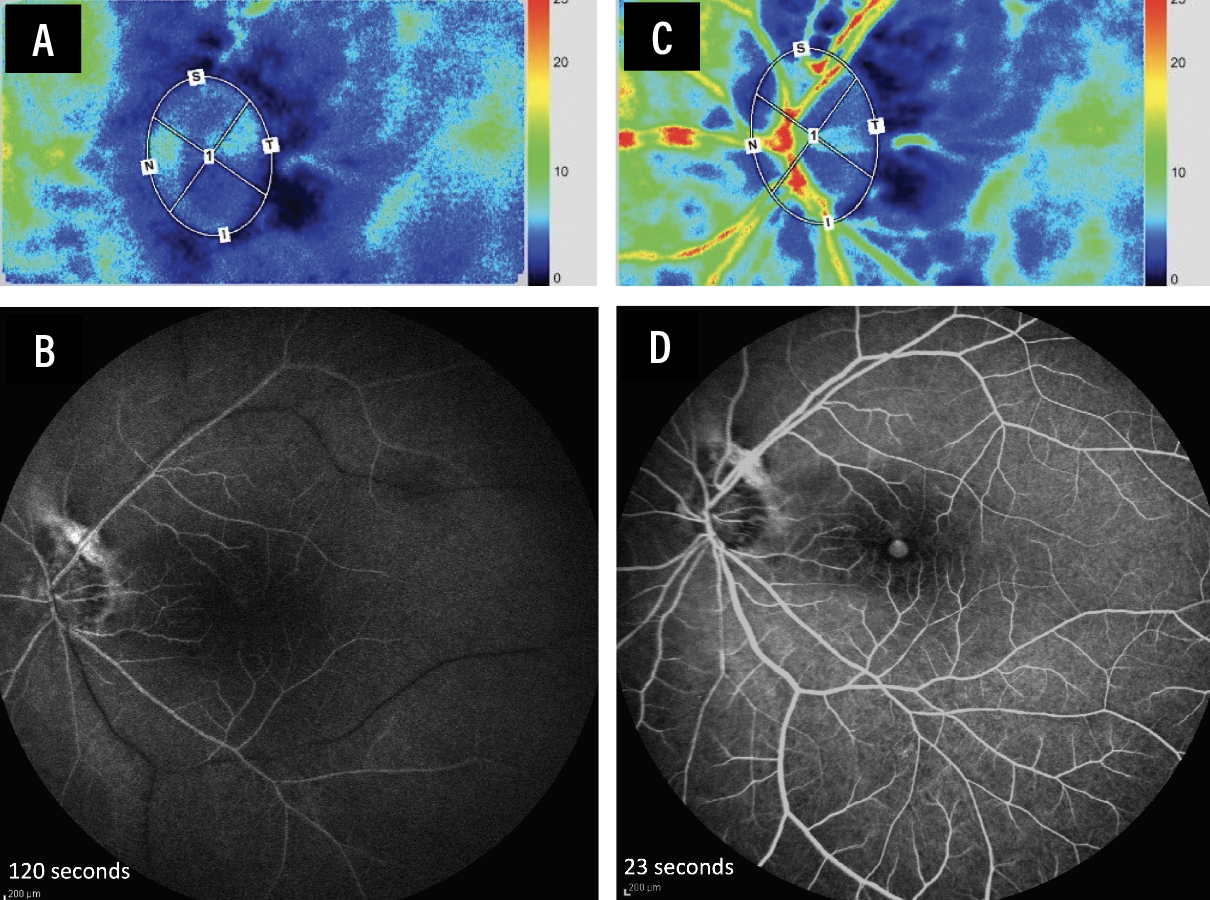 |
| Figure 3. Outcomes of a case of an 84-year-old male with central retinal artery occlusion presenting 48 hours following onset of symptoms. Laser speckle flowgraphy and fluorescein angiography from presentation (A, B) to one week following retinal arterial cannulation with tissue plasminogen activator (tPA, C, D) showed improved retinal perfusion. Mean blur rate of vessel tissue area improved from 2.9 to 14.9. Visual acuity improved from light perception to hand motion at one month. The limited visual improvement in this case likely was due to the retinal ischemic damage from the time elapsed since disease onset to presentation. |
Postoperative considerations
Instruct patients to remain prone overnight to prevent postoperative bleeding and to not to engage in strenuous activities. Maintaining blood pressure within a normal range postoperatively is an important consideration. Patients may also be prescribed aspirin (50 mg) daily for two weeks as an anti-platelet drug for reducing the risk of reocclusion.
Bottom line
Intraretinal-arterial cannulation may serve as an option for restoring microcirculation in eyes affected by CRAO. Important preoperative and postoperative considerations apply for this procedure. Selecting the appropriate patients is critical. Establishing a system that enables rapid surgery in the treatment of CRAO may also enhance patient outcomes. RS
REFERENCES
1. M. Schrag M, Youn T, Schindler J, Kirshner H, Greer D. Intravenous fibrinolytic therapy in central retinal artery occlusion. JAMA Neurol. 2015;72:1148-1154.
2. Schumacher M, Schmidt D, Jurklies B, et al, for the EAGLE-Study Group. Central retinal artery occlusion: local intra-arterial fibrinolysis versus conservative treatment, a multicenter randomized trial. Ophthalmology. 2010;117:1367-75.e1.
3. Sobol EK, Sakai Y, Wheelwright D, et al. Intra-arterial tissue plasminogen activator for central retinal artery occlusion. Clin Ophthalmol. 2021;15:601-608.
4. Kadonosono K, Yamane S, Inoue M, Yamakawa T, Uchio E. Intra-retinal arterial cannulation using a microneedle for central retinal artery occlusion. Sci Rep. 2018;8:1360.
5. Chernyshev OY, Martin-Schild S, Albright KC, Barreto A, Misra V, Acosta I, Grotta JC, Savitz SI. Safety of tPA in stroke mimics and neuroimaging-negative cerebral ischemia. Neurology. 2010;74:1340-1345




