 |
|
Bios
Dr. Rodriguez is a retina fellow at Wills Eye Hospital, Philadelphia. Dr. Hsu is codirector of retina research at Wills Eye Hospital, associate professor at Thomas Jefferson University and partner at Mid Atlantic Retinal DISCLOSURES: Dr. Rodriguez and Dr. Hsu have no relevant financial relationships to disclose. |
A 62-year-old man presented to our retina clinic with decreased vision in both eyes for the past few years. His medical history was pertinent for human immunodeficiency virus treated with multiple medications.
Work-up and imaging
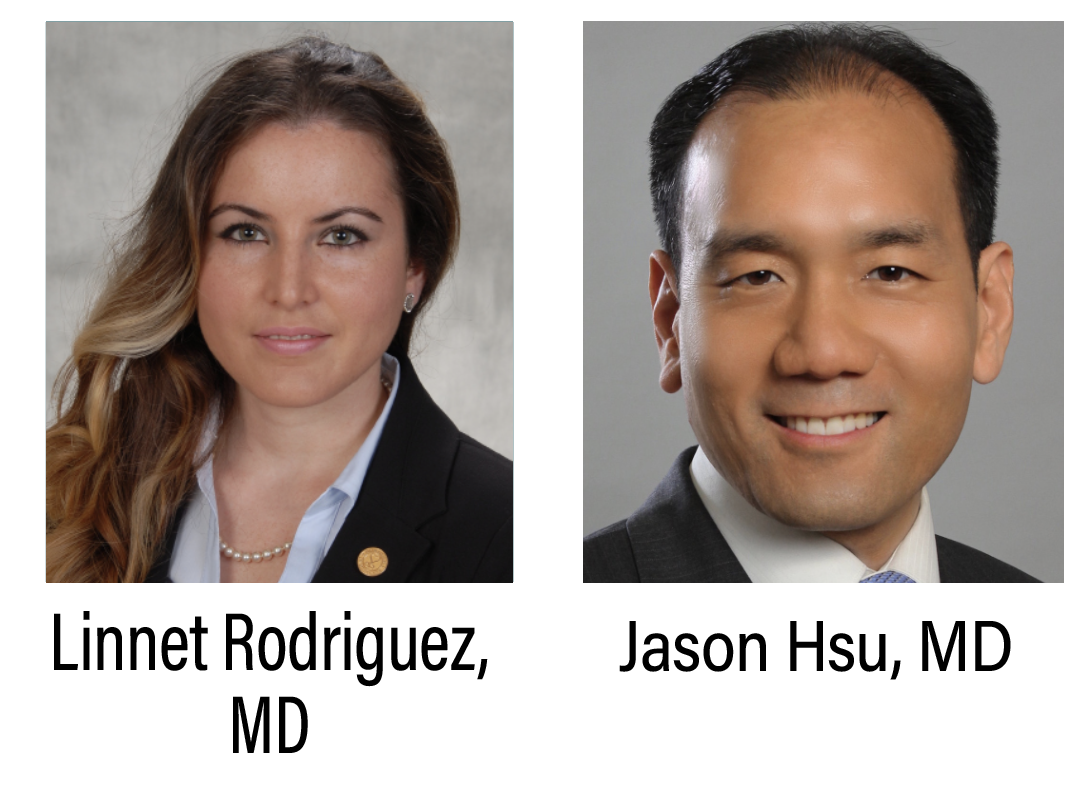
His visual acuity was 20/40 in both eyes. Intraocular pressures were within normal limits. Anterior segment examination was pertinent for 1+ nuclear sclerosis (NSC) in the right eye and 2+ NSC in the left eye. Fundus examination revealed extensive areas of circumferential and bilateral chorioretinal atrophy localized to the periphery, mostly sparing the macula. The left eye, however, did show a small area of hypopigmentation in the macula (Figure 1).
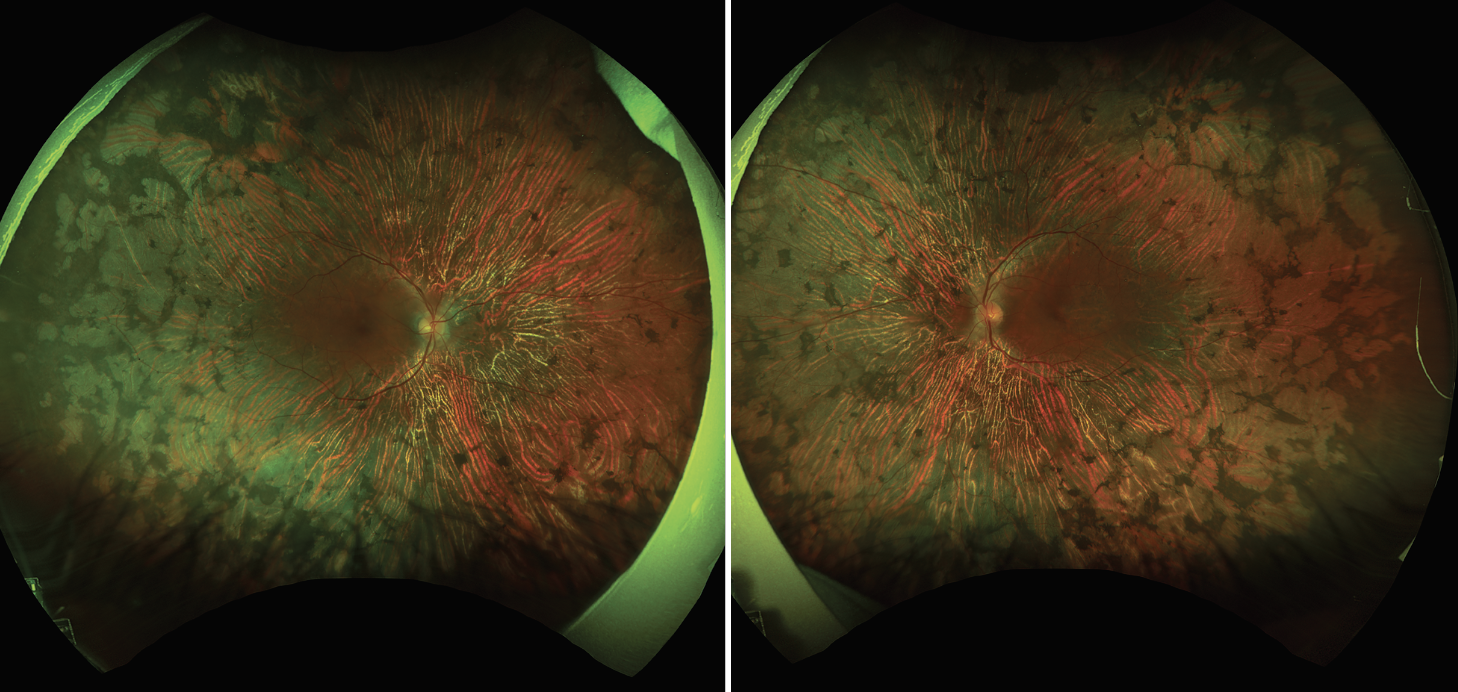
Optical coherence tomography of both eyes showed intact laminations of the retina with intraretinal cysts at the level of the inner nuclear layer. Both eyes showed attenuation of the ellipsoid and interdigitation zone, more pronounced in the left eye (Figure 2).
 |
| Figure 1. Ultra-widefield pseudocolor fundus images show chorioretinal atrophy and areas of stippled pigmentary clumps in the periphery, mostly sparing the macula. |
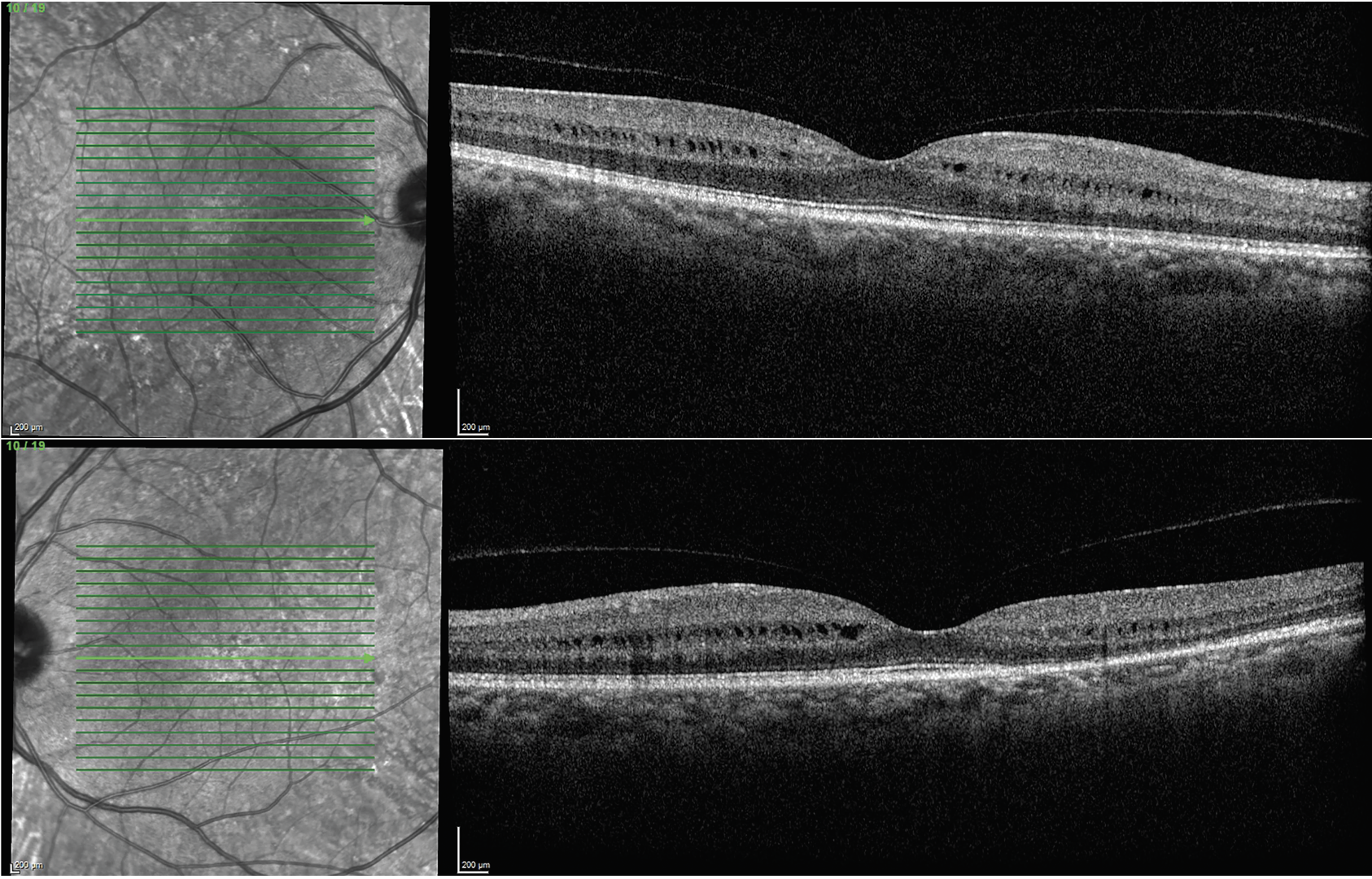
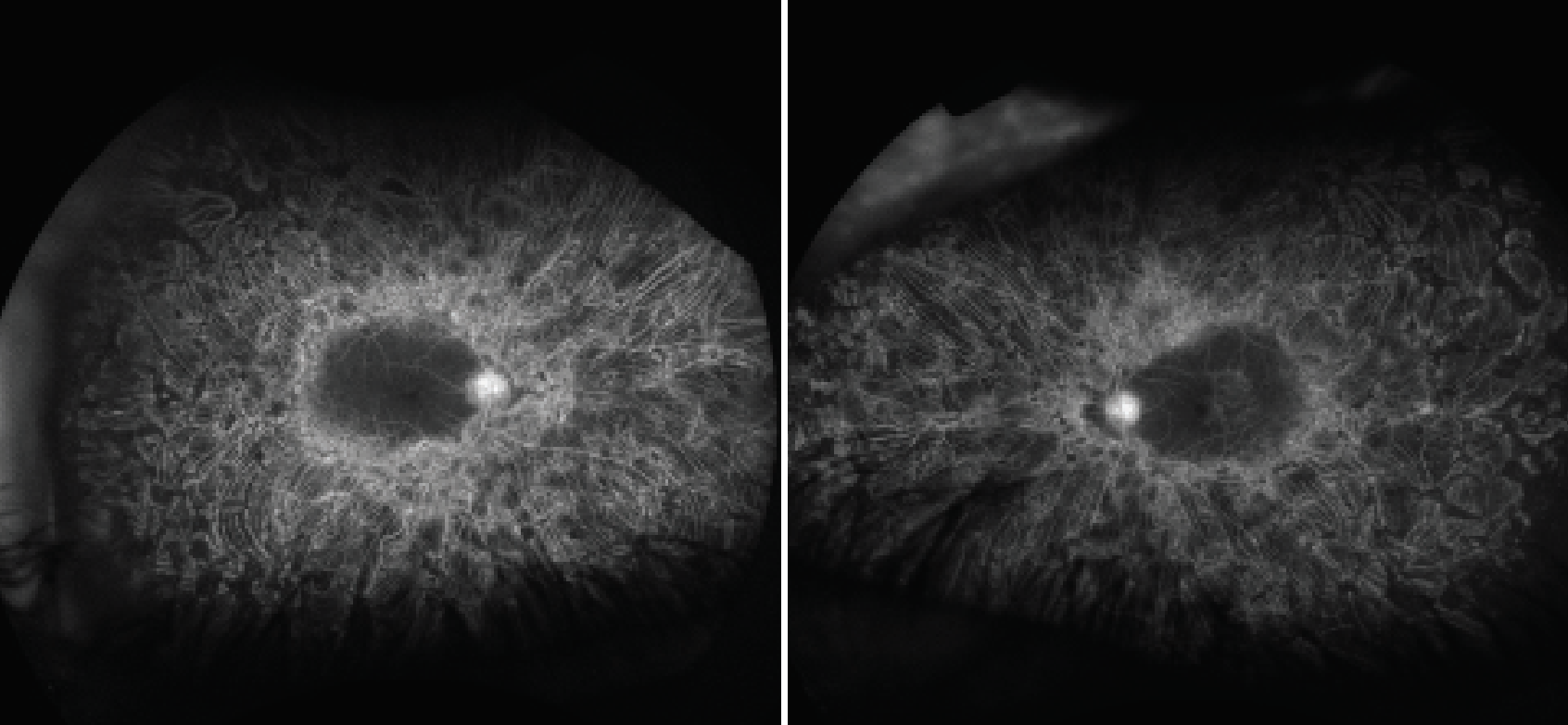
Fundus autofluorescence demonstrated extensive circular patches of hypoautofluorescence extending from the temporal arcades to the periphery in a circumferential pattern. These areas correlated with the chorioretinal atrophy seen on the fundus examination.
Pinpoint areas of hyper- and hypoautofluorescence also appeared along the temporal arcades in both eyes. The macula seemed to be spared in the right eye, but the left eye showed an irregular zone of hyperautofluorescense in the temporal parafoveal area (Figure 3).
 |
| Figure 2. Optical coherence tomography shows intraretinal cysts in the inner nuclear layer and attenuation of the ellipsoid and interdigitation zones, more pronounced in the left eye. |
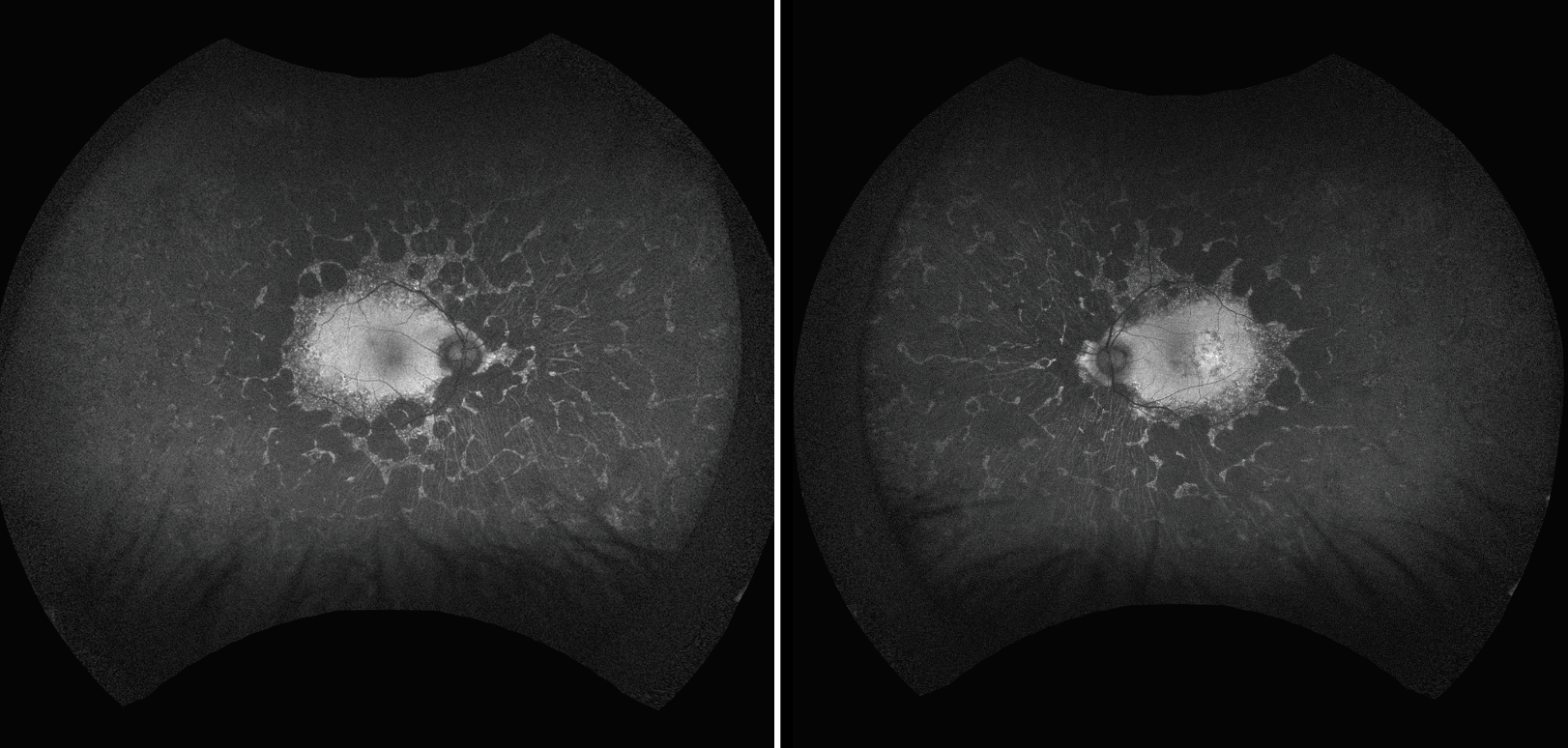
Fluorescein angiography revealed staining at the edges of the chorioretinal lesions as well as pinpoint areas along the arcades with relative sparing of the macula. The left eye exhibited a small area of staining in the temporal macula (Figure 4).
Additional history and diagnosis
The patient was diagnosed with HIV in 1990. He was initially treated with monotherapy with didanosine (Videx, Bristol
Myers Squibb) and later was transitioned to multiple combined regimens with medications, including various nucleoside/nucleotide reverse transcriptase inhibitors, protease inhibitors and integrase strand transfer inhibitors.
Laboratory testing was negative for tuberculosis. Syphilis titers were stable and, based on the infectious disease specialist’s recommendation, no repeated treatment was necessary at that point. His CD4 count was 400 with undetectable viral load. Genetic testing was negative for alternative diagnoses, including gyrate atrophy and choroideremia.
Given the patient’s medical history, testing and imaging findings, he was diagnosed with didanosine-associated retinal toxicity (DART). Given multiple treatments and macular findings in the left eye, however, a superimposed maculopathy from medications such as ritonavir could not be ruled out.1
 |
| Figure 3. Ultra-widefield fundus autofluorescence shows extensive areas of hypoautofluorescense from the temporal arcades to the periphery but sparing the macula. |
Follow-up
We treated the patient with topical dorzolamide t.i.d. in both eyes, which resulted in slight improvement of the bilateral intraretinal cysts. We advised him to continue HIV treatment with elvitegravir-cobicistat-emtricitabine-tenofovir combination therapy (Genvoya, Gilead Sciences) and to avoid didanosine, which he had discontinued years before. Because retinal toxicity due to didanosine can progress despite discontinuation and other antiretroviral medications can exacerbate it, we follow the patient regularly with FAF and fundus photography.
 |
| Figure 4. Late-phase ultra-widefield fluorescein angiography shows hyperfluorescence at the edge of the chorioretinal atrophy and along the arcades but sparing the macula. |
Characteristics of DART
Didanosine is a synthetic purine adenine nucleoside analogue in the nucleoside reverse transcriptase inhibitor (NRTIs) class. The Food and Drug Administration approved it in 1991 for treatment of HIV infection.2 It was initially used as monotherapy until newer drugs and combination regimens emerged after 1996.3
At the molecular level, didanosine has been proven to cause progressive loss of mitochondrial DNA by causing depletion of the DNA polymerase responsible for its synthesis. As a result, there is a shift away from oxidative phosphorylation toward aerobic glycolysis, leading to an increase in lactate secretion and impaired cellular function, which results in atrophy of the choriocapillaries and the outer retina.4
Patients can experience a gradual and bilateral decrease in peripheral vision as well as photopsia and nyctalopia.2 Fundus findings consist of irregular areas of sharply demarcated chorioretinal atrophy that may coalesce. These are usually bilateral and manifest in a circumferential pattern, mostly spanning from the mid-periphery to the ora serrata and sparing the macula. The optic nerve head is uninvolved.3
Imaging findings
FAF findings are pertinent for hypoautofluorescence matching the areas of chorioretinal atrophy. FA can show early window defects in the same areas with late staining at the concentric margins.5 OCT may demonstrate normal laminations of the macula with some intraretinal cysts. These cysts may represent Muller cell dysfunction or structural alterations due to outer retinal changes. OCT of the peripheral retina may show loss of the outer retina, RPE and choriocapillaris.6,7 Electroretinogram may reveal a bilateral decrease in rod and cone response.8
Treatment
There is no proven treatment for DART. Because of advances in highly active antiretroviral therapy, didanosine is rarely prescribed anymore. For patients still on this therapy, they should discontinue it.
Bottom line
Didanosine can cause bilateral circumferential mid peripheral chorioretinal atrophy with macula sparing. Despite medication discontinuation, toxicity may progress. Other antiretroviral drugs may also exacerbate the problem. Patients should be followed regularly with fundus images and FAF. They should also be referred to an infectious disease specialist, when appropriate, for changes in therapy. RS
REFERENCES
1. Bunod R, Miere A, Zambrowski O, Girard PM, Surgers L, Souied EH. Ritonavir associated maculopathy- multimodal imaging and electrophysiology findings. Am J Ophthalmol Case Rep. 2020;19:100783.
2. Gabrielian A, MacCumber MM, Kukuyev A, Mitsuyasu R, Holland GN, Sarraf D. Didanosine-associated retinal toxicity in adults infected with human immunodeficiency virus. JAMA Ophthalmol. 2013;131:255-259.
3. Haug SJ, Wong RW, Day S, et al. Didanosine retina toxicity. Retina. 2016;36 Suppl 1:S159-S167.
4. Hu X, Calton MA, Tang S, Vollrath D. Depletion of mitochondrial DNA in differentiated retinal pigment epithelial cells. Sci Rep. 2019;9:15355.
5. Corradetti G, Violanti S, Au A, et al. Wide field retinal imaging and the detection of drug associated retinal toxicity. Int J Retina Vitreous. 2019;5 (Suppl 1): 26.
6. Lopez JM, Miere A, Crincoli E, Souled EH. Didanosine retinal toxcity. Oftalmol ClinExp. 2022;15:3185-e197.
7. Faure C, Chassery M, Ores R, Audo I. Didanosine-induced retinopathy: New insights with long-term follow-up. Ocul Immunol Inflamm. 2022;30:1625-1632.
8. Fernando A, Anderson O, Holder G, et al. Didanosine-induced retinopathy in adults can be reversible. Eye (Lond.). 2006;20:1435–1437.




