A 59-year-old woman presented to the glaucoma service at our institution for glaucoma suspect evaluation. She was originally evaluated by an outside optometrist who documented intraocular pressures in the mid-30s and advanced optic nerve head cupping in both eyes. She had not been compliant with glaucoma treatment or follow-up for the prior 2.5 years.
Her glaucoma workup demonstrated end-stage angle-closure glaucoma, greater in the right eye than the left. She was also found to have macular retinoschisis and a serous retinal detachment in her right eye, a finding that has been described among glaucoma patients.
Examination Findings
On initial exam, pinhole visual acuity was 20/125 OD and 20/25 OS. IOPs were 39 mmHg OD and 32 mmHg OS. She had a relative afferent pupillary defect in the right eye. Gonioscopy revealed narrow angles in both eyes. Cup-to-disc ratio was 0.95 OD and 0.90 OS, with no optic nerve pit or coloboma. The
 |
fundus exam was limited because the patient could not be dilated safely due to her narrow angles. Retinal vessels appeared normal. She was a low myope of about -1 D. She had moderate nuclear sclerotic cataracts in both eyes.
Workup
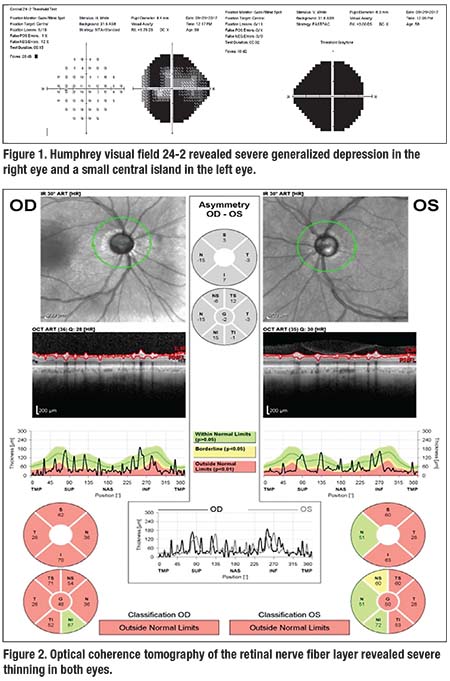
A 24-2 Humphrey visual field showed severe generalized depression in the right eye and a small central island in the left (Figure 1).
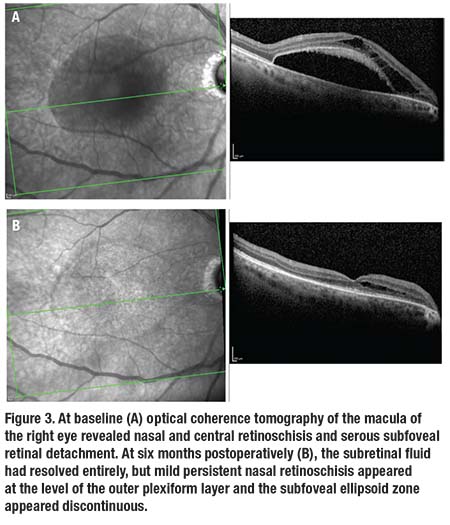
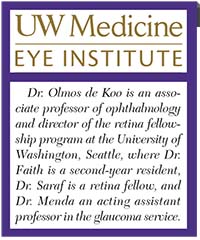
Optical coherence tomography of the retinal nerve fiber layer revealed severe thinning in both eyes (Figure 2). OCT of the macula of the right eye revealed retinoschisis at the level of the outer plexiform layer (OPL), extending from just temporal to the optic nerve to the fovea. A fovea-involving serous RD appeared deep to the retinoschisis (Figure 3A, page 12). OCT of the left eye was normal.
Diagnosis and Management
Given this patient’s advanced glaucoma, we decided to perform combined trabeculectomy and phacoemulsification with intraocular lens placement in both eyes. She had the procedure first in her right eye, then in the left eye five months later. She had an uncomplicated postoperative course, including laser suture lysis and subconjunctival 5-fluorouracil in both eyes. Overall, she experienced good reduction in IOP in both eyes.
Follow-up OCT of the right macula six months after surgery (Figure 3B) revealed reduced but persistent retinoschisis at the level of the OPL with complete resolution of the subretinal fluid. Outer retinal atrophy with disruption of the ellipsoid zone in the area of the resolved detachment was noted. Best corrected visual acuity was 20/70, presumed due to maculopathy from longstanding fluid.
Discussion
The combination of macular retinoschisis and serous detachment has been described in cases of optic disc pits, optic disc colobomas, vitreomacular traction, juvenile retinoschisis and pathologic myopia.
 |
More recently, this entity has been associated with glaucoma patients.
A large series described peripapillary retinoschisis in glaucoma patients.1 Of 372 patients evaluated, 25 areas of retinoschisis were identified in 22 patients (5.9 percent). The schisis most commonly involved the retinal nerve fiber layer with variable involvement of deeper retinal layers. This series reported no macular retinoschisis or RD.
Other studies have shown retinoschisis involving the macula. A series of patients with optic nerve cupping and macular schisis, some with serous RD, found that macular fluid resolved in one patient after filtering surgery for uncontrolled glaucoma, and two other patients underwent vitrectomy with intraocular gas with almost total resolution of macular fluid.2 Another report described two cases of peripapillary and macular schisis in narrow-angle patients.3 One patient had resolution of macular schisis with modestly reduced IOP after laser peripheral iridotomy. A case of macular schisis in a patient with primary open-angle glaucoma with postural IOP fluctuations, in which trabeculectomy resulted in resolution of the schisis changes, had also been reported.4
Although patients can have two different concomitant pathologies, the trend of finding serous RD associated with optic nerve cupping is illustrated by our report and others. Two similar cases had been described: a case of macular schisis and serous detachment in a patient with angle closure glaucoma, advanced cupping and an IOP of 52 mmHg;5 and a case of peripapillary retinal schisis and serous detachment in a patient with POAG and cupping that resulted in spontaneous resolution.6
A proposed mechanism for this entity is similar to the mechanism attributed to optic disc pit maculopathy. Liquefied vitreous tracks through a break in the thin tissue of the optic cup and into the retina that can lead to edema, schisis or even serous RD.2
The role of IOP is debatable. In the aforementioned case of macular schisis and detachment, a history of central scotoma that followed an IOP spike up to 52 mmHg supports that IOP may have played a role.5 This is further supported by cases where fluid resolved after IOP-lowering surgery.2,4 On the other hand, macular schisis has been reported in patients with normal-tension glaucoma, which argues against the role of elevated IOP.7
Management of this entity can vary. As seen in our case and others,2,4 surgery to address uncontrolled glaucoma can lead to resolution of fluid.
 |
Spontaneous resolution has also been reported, which makes observation a reasonable option.6 Pars plana vitrectomy with gas tamponade has also been employed successfully.2 RS
REFERENCES
1. Lee EJ, Kim TW, Kim M, Choi YJ. Peripapillary retinoschisis in glaucomatous eyes. PLoS One. 2014;9:e90129.
2. Zumbro DS, Jampol LM, Folk JC, Olivier MM, Anderson-Nelson S. Macular schisis and detachment associated with presumed acquired enlarged optic nerve head cups. Am J Ophthalmol. 2007;144: 70-74.
3. Kahook MY, Noecker RJ, Ishikawa H, et al. Peripapillary schisis in glaucoma patients with narrow angles and increased intraocular pressure. Am J Ophthalmol. 2007;143:697-699.
4. Woo R, Akil H, Koulisis N, Olmos de Koo LC, Tan JCH. Sustained resolution of macular retinoschisis after trabeculectomy in a patient with progressive glaucoma. J Glaucoma. 2017;26: e180-186.
5. Hollander DA, Barricks ME, Duncan JL, Irvine AR. Macular schisis detachment associated with angle-closure glaucoma. Arch Ophthalmol. 2005;123:270-272.
6. Farjad H, Besada E, Frauens BJ. Peripapillary schisis with serous detachment in advanced glaucoma. Optom Vis Sci. 2010;87:e205-217.
7. Zhao M, Li X. Macular retinoschisis associated with normal tension glaucoma. Graefes Arch Clin Exp Ophthalmol. 2011; 249:1255-1258.



