Retina specialists have long debated the timing for cataract surgery in patients with neovascular age-related macular degeneration. Now a team of researchers from Finland have weighed in with a small national study that adds more evidence in the “it doesn’t matter” column.
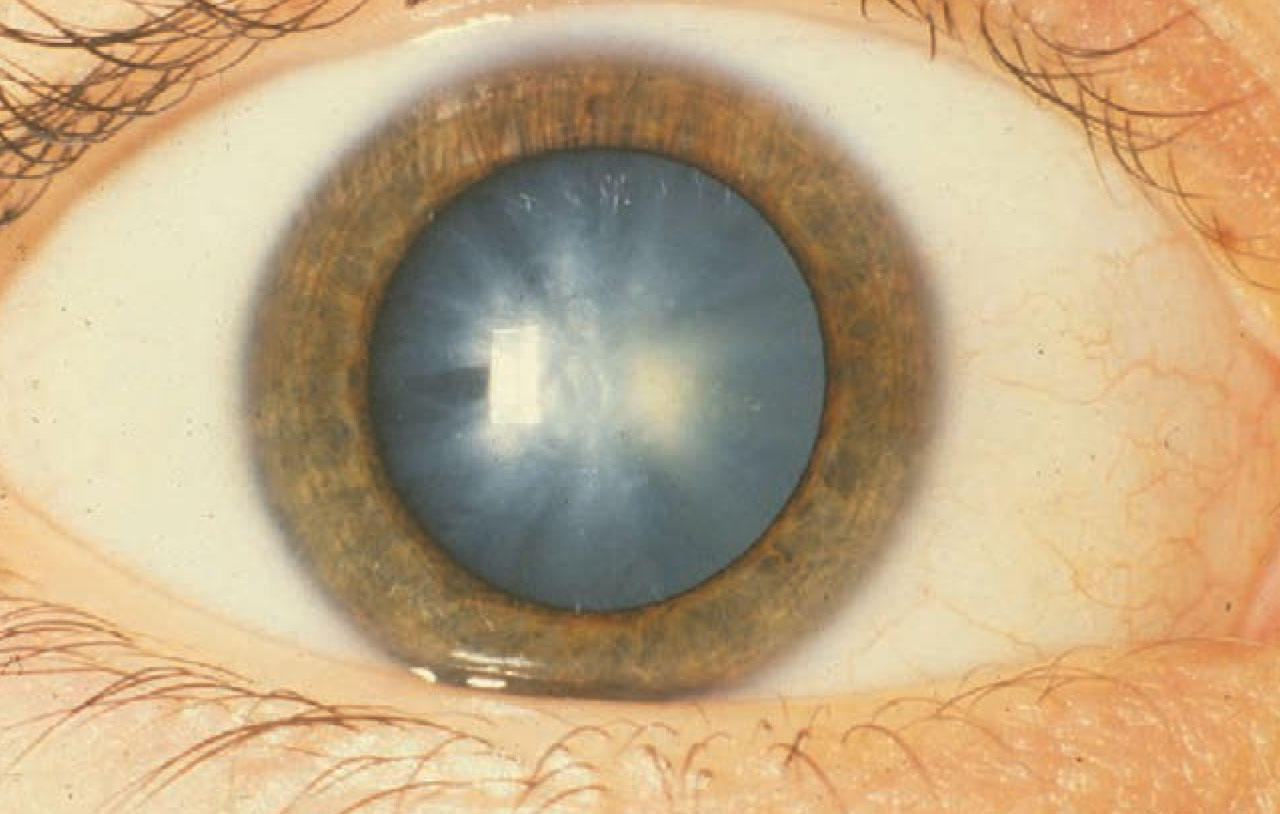 |
| Finnish researchers say age-related macular degeneration shouldn’t delay removing one of these. Click image to enlarge. |
“Our findings add data that cataract surgery should not be postponed due to fear of disease activation in wet AMD patients,” Petteri Karesvuo, MD, of the University of Helsinki, tells Retina Specialist. “Central subfield macular thickness (CSMT) decreased postoperatively and increased only in one of 111 patients.”
Dr. Karesvuo was the lead author of the study of patients with wet AMD who had cataract surgery at Helsinki University Hospital from 2014 to 2018.1 “Injection intervals did not increase after cataract surgery,” he adds.
“We found no justification to support delaying surgery until dry macula has been achieved,” Dr. Karesvuo and colleagues wrote.
CSMT, BCVA results
Their retrospective registry-based study evaluated best-corrected visual acuity and CSMT at three different intervals: at the time of nAMD diagnosis; the last time prior to cataract surgery; the first time after surgery; and at one year after surgery. They also documented the cumulative number of anti-VEGF injections at and after surgery, as well as systemic and topical medications.
In BriefThe Food and Drug Administration has accepted Genentech/ Roche’s Biologics License Application under priority review for the Port Delivery System with ranibizumab (PDS) for the treatment of neovascular age-related macular degeneration. The FDA is expected to make a decision on approval by October 23. Novartis has terminated three studies investigating Beovu (brolucizumab) for the treatment of nAMD: MERLIN, RAPTOR and RAVEN. The decision came after Novartis reported the first interpretable year-1 results of the Phase III MERLIN study that showed a higher rate of intraocular inflammation, including retinal vasculitis and retinal vein occlusion, than aflibercept. Novartis says it will pursue an update to the Beovu prescribing information globally. The FDA accepted the resubmitted New Drug Application from Bausch + Lomb and Clearside Biomedical for Xipere, the triamcinolone acetonide suprachoroidal injectable suspension. The FDA determined this is a Class 2 resubmission and assigned a Prescription Drug User Fee Act action date of October 30. The proposed indication is for macular edema associated with uveitis. The FDA granted fast-track designation to OPT-302, Opthea’s VEGFC/-D “trap” inhibitor in combination with anti-VEGF-A therapy for neovascular AMD. |
“Cataract surgery did not significantly influence the incidence of hemorrhages, pigment epithelial detachment, intraretinal fluid or subretinal fluid when comparing macular status at surgery to that at first postoperative visit and at one year,” the researchers wrote.
Among their key findings were:
- CSMT at the time of cataract surgery was 280.1 ±75 µm; CSMT postoperatively was 268.6 ±67.6 µm (p = 0.001); CSMT at one year was 265.9 ± 67.9 µm (p = 0.003).
- BCVA in logMAR units before surgery was 0.70 µm ±0.46 (Snellen equivalent median and intraquartile range [IQR]; 0.30, 0.125–0.40); postoperatively it was 0.39 ± 0.40 (Snellen equivalent median and IQR; 0.50, 0.32–0.80; p < 0.001); and at one year it was 0.33 ± 0.34 (Snellen equivalent median and IQR; 0.50, 0.32– 0.80; p<0.001).
- The anti-VEGF treatment interval before surgery was 6.53 ±2.08 weeks; 7.03 ± 2.23 weeks at one year (p = 0.246); and 7.05 ±2.57 weeks at the last documented visit (p = 0.035).
Dr. Karesvuo and colleagues found that postoperative CSMT change inversely correlated with the preoperative CSMT levels (p < 0.001), but not with the cumulative number of anti-VEGF injections before surgery (p = 0.691). “The CSMT change postoperatively or at one year did not correlate with patient age at surgery, nor with the preoperative BCVA,” they wrote.
The researchers repeated the multiple regression analysis to control for diabetes status and use of anti-inflammatory drugs, anticoagulants, calcium-channel blockers and statins.
The results remained consistent as only CSMT status before surgery was significantly correlated with postoperative CSMT change, while anti-VEGF treatment and presence of subretinal and intraretinal fluid were not.
 |
More research needed
Dr. Karesvuo acknowledges that this isn’t the final word on timing of cataract surgery in patients with wet AMD. “To get a better understanding of the cataract surgery in wet AMD patients, larger sample-sized studies would give more information,” he says. Additionally, future studies could evaluate the effect of cataract surgery in patients with newly diagnosed wet AMD, he notes. “In our study, the patients had a mean of 24.8 ±17.3 injections before surgery,” Dr. Karesvuo says. The researchers acknowledge that the small cohort size and short follow-up are limitations of their study, but note that one year of follow-up “is reasonably long enough to assess CSMT, visual acuity gain and anti-VEGF burden.” RS
Dr. Karesvuo and colleagues have no relevant disclosures.
FOR THE RECORD In the article “Will biosimilars fi nd their place in retina?” in the May/June 2021 issue, ONS-5010/Lytenava (Outlook Therapeutics) was misidentifi ed as a biosimilar of ranibizumab. It's a biosimilar of bevacizumab. |
REFERENCES
1. Karesvuo P, Elbaz U, Achiron A, Hecht I, Kaarniranta K, Tuuminen R. Effect of cataract surgery on wet age-related macular degeneration activity. Acta Ophthalmol. Published online April 10, 2021. doi: 10.1111/aos.14864.



