 |
 |
Over the past four decades we’ve witnessed unprecedented advances and innovation in vitreoretinal surgery.1 Current vitrectomy platforms have automated most parts of vitrectomy surgery, such that surgeons nowadays can perform steps such as fluid-air exchange, viscous fluid injection of silicone oil and laser retinopexy independently, efficiently and unassisted, with controls for all of these steps being at our fingertips (and toe tips).1,2
Yet, when it comes to peripheral vitrectomy, particularly vitreous base shaving, many surgeons still rely on skilled assistants to provide scleral indentation the same way we did when pars plana vitrectomy first started more than 40 years ago.
Here, I describe a technique that uses a scleral depressor-transilluminator to provide excellent visualization of the peripheral retina for unassisted peripheral vitrectomy.
In some settings, retina surgeons are surrounded by bright and eager assistants, surgical retina fellows and ophthalmology residents who can provide scleral depression, particularly in cases where good vitreous base shaving is desired, such as when performing a repair of a rhegmatogenous retinal detachment.
For many of us in private practice, where trainee surgeons aren’t readily available, the options include training scrub technicians to perform scleral depression or using an endoilluminating chandelier system. But while both of these approaches can be effective, each has its unique challenges and drawbacks.
 |
Limits of endoillumilnation
A number of commercially available chandelier systems are compatible across vitrectomy platforms.3-5 While endoillumination with these devices can be adequate in many cases,6 the illumination of the retina is far from uniform. With the chandelier, parts of the peripheral retina are well-illuminated while other parts remain in the dark, and peripheral vitrectomy with less-than-ideal illumination of the retina increases the risk of iatrogenic breaks.
In addition, glare can hamper vitrectomy within a few clock hours of the chandelier device. Chandelier depression in a phakic eye raises the risk of lens touch and iatrogenic cataract, which, although rare, would be a very unwelcome complication.
Lastly, the price of a chandelier system is not insignificant, particularly for surgeons operating at increasingly cost-conscious ambulatory surgical centers. Our surgical technicians can learn to perform scleral depression for vitrectomy that rivals that of ophthalmology residents and beginning retina fellows. Yet, most community hospitals and ASCs don’t have dedicated surgical eye teams, thus making access to trained assistants inconsistent at best.
It’s not uncommon for community retina surgeons to walk into the operating room and find that the assigned assistant for the day is a surgical tech with minimal or no ophthalmology and retina experience. Attempting to perform depressed vitrectomy with an inexperienced assistant in that setting is unsafe and ill-advised.
All these issues have created the need for a technique and device that would transfer the depressor for vitreous base shaving from the hands of an unskilled assistant to the hands of the surgeon. As such, this would not only enhance the surgeon’s satisfaction and independence, but also improve patient safety.
 |
Scleral transillumination
Scleral transillumination is not a novel technique. It has been and continues to be used in ocular oncology for localization of intraocular tumors and optimization of radioactive plaque placement. Yet, its use in intraocular surgery hasn’t gained traction.
We recently published a small pilot study evaluating the technique of using endo-
illumination light pipe in a scleral depressor-transilluminator in conjunction with Alcon’s NGenuity 3D system.7 We found that scleral depression-transillumination with the light pipe was safe and effective for performing peripheral vitrectomy in a majority of the patients with common vitreoretinal surgical indications (Video). Caucasian myopic eyes with thinner sclera and lightly pigmented fundi appeared to be the best candidates.
The advantage of using this technique with a digital microscope is the ability to enhance endogenous luminance, extend the depth of field and allow for manipulation of the color channels to potentially enhance the Tyndall effect and visualization of the peripheral vitreous gel.8
 |
 |
Alternative to digital microscope
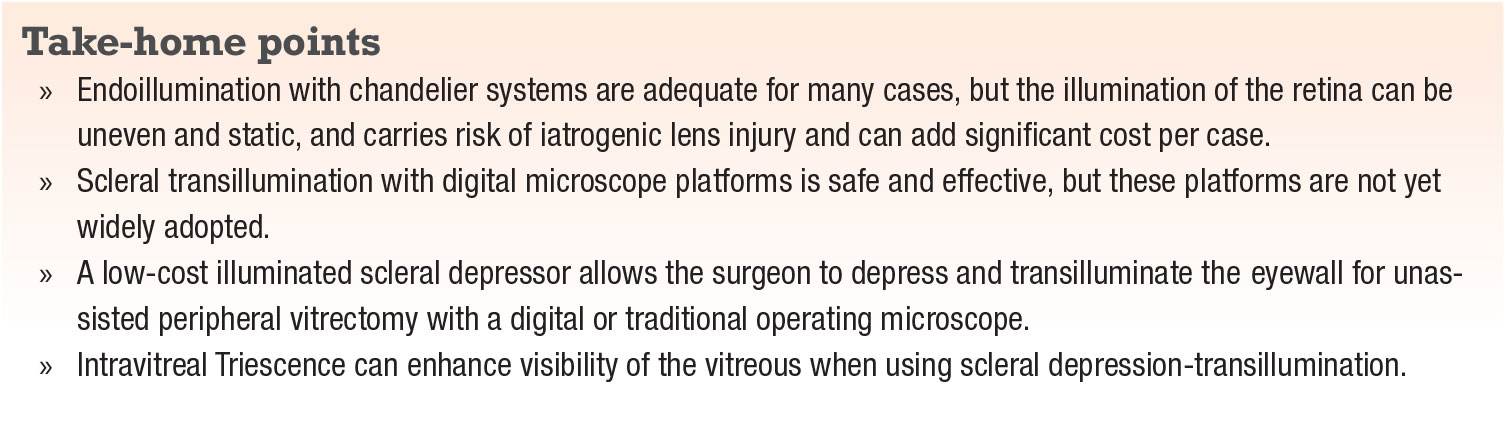
Considering that digital microscope platforms like NGenuity are still not widely available, particularly at community-based retina practices, we designed a device adapter for endoillumination light pipe that would allow conversion of any gauge light pipe into a scleral depressor-transilluminator and allow it to be used with any analogue operating microscope (Figure 1, page 21).
The device is made of inert polycarbonate molded into the shape of a traditional ball-point depressor. Its stiffness and feel approach that of a regular scleral depressor. To further enhance its stiffness and reduce light backscatter and glare, the shaft of the depressor is fortified with a 19-ga. hypodermic needle.
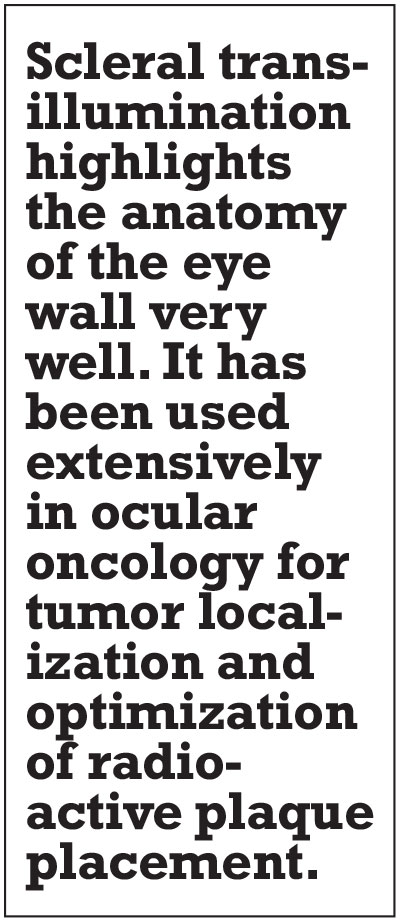
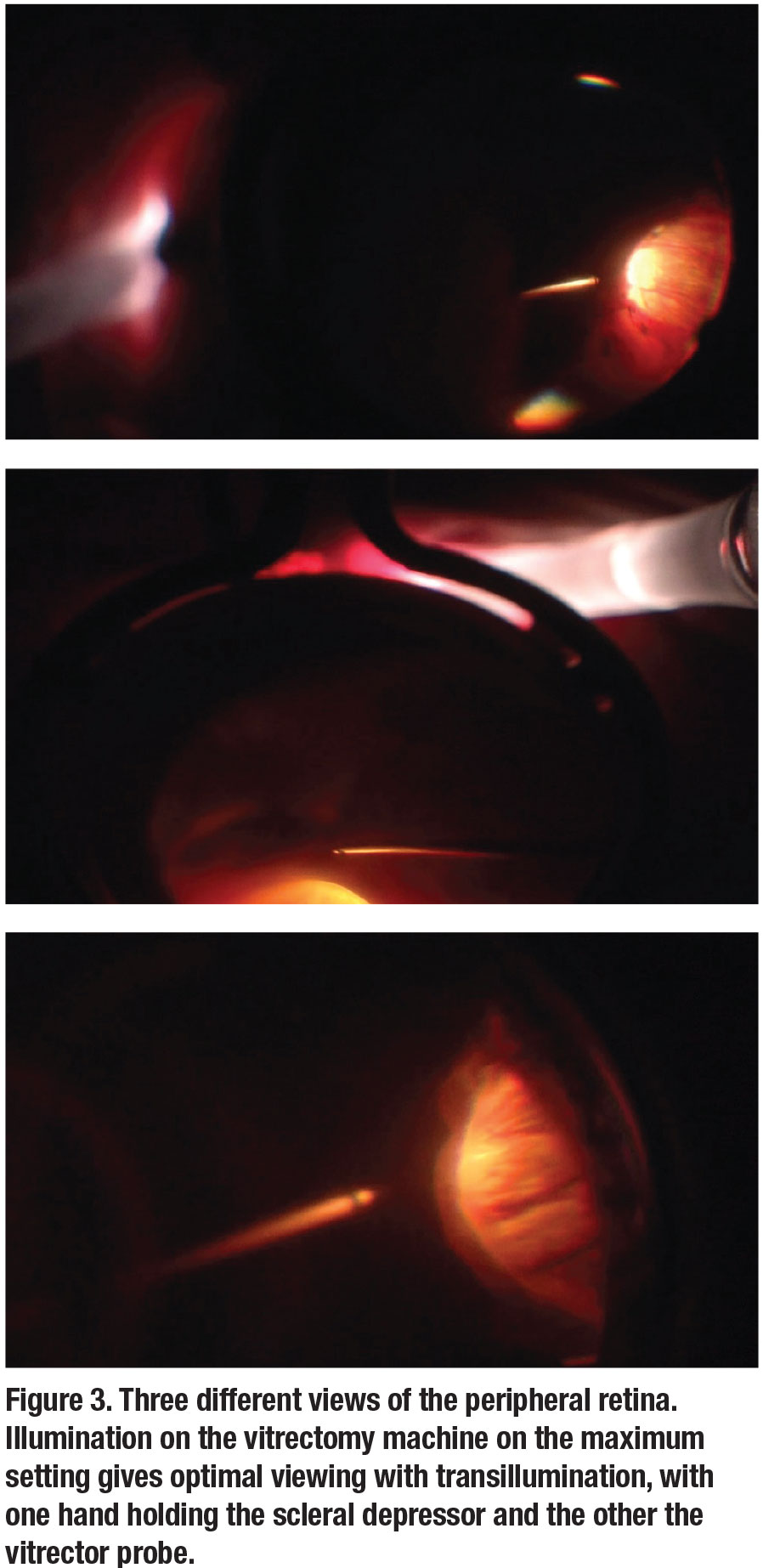
The light pipe is inserted into the a back end and glides into position where the tip of the light ends up at the inside of the distal depressor tip once it’s fully seated (Figures 1 and 2). For optimal viewing, the illumination on the vitrectomy machine is adjusted to the maximum setting. The depressor tip is machined to achieve maximum optical clarity while its polished ball tip glides seamlessly along the scleral surface, even for patients with tighter orbits. The surgeon performs unassisted vitrectomy with one hand while depressing and transilluminating simultaneously with the other (Video). The device I use is produced and marketed by Vortex Surgical. While the Vortex surgical device is designed to be used with the Alcon system, similar devices are available for other platforms, such as the DORC Eva system.
The chief advantage of this technique is that it gives the retina surgeon absolute control of the eye during peripheral vitrectomy, a surgical step that had traditionally required trained assistants. Use of the adapter device allows conversion of any gauge light pipe into a scleral depressor-transilluminator, providing the required stiffness and glare reduction, and eliminating the chance of scleral wall perforation—a risk if the light pipe alone were to be used. It achieves this at a fraction of the cost of a traditional chandelier.
 |
Navigate the learning curve
With this technique, the anatomy of the retina, retinal pigment epithelium and choroid is well-visualized, allowing for detection of even small retinal breaks. Like any new technique, there’s a learning curve of approximately five to 10 cases to get the “feel” for it and gain comfort with a view that’s different from traditional endoillumination. The view is best in thin-walled, blonde, myopic Caucasian eyes, but can be challenging in highly pigmented fundi.
Although the vitreous itself may be challenging to visualize directly, as with traditional endoilluminated depressed vitrectomy, adjuvants such as intravitreal Triescence can enhance visibility.
Methodical removal
You must be methodical when removing the vitreous, doing it one clock hour at a time, starting at the posterior edge of the vitreous base and moving anteriorly, ensuring complete vitreous removal before moving to the adjacent clock hour. This will ensure complete peripheral vitrectomy without skipping any areas, particularly in cases such as retinal detachment repair.
 |
Bottom line
Using a light pipe in conjunction with the illuminated scleral depressor allows for visualization of the peripheral retina with depression during vitrectomy without relying on an assistant. It allows unassisted vitrectomy with both digital and traditional microscopes. Cheaper than a chandelier system, the illuminated depressor promotes patient safety and the surgeon’s independence while also helping to reduce the cost of each case. RS
View the video below.
Illuminated scleral depression for peripheral vitrectomy.
REFERENCES
1. Fujii GY, De Juan E Jr, Humayun MS. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology. 2002;109:1807-1812.
2. Oshima Y. Choices of wide-angle viewing systems for modern vitreoretinal surgery: A semi-quantitative evaluation of the visual angle field and imaging contrast. Retina Today. 2012;5:37-42.
3. Eckardt C, Eckardt T, Eckardt U. 27-gauge Twinlight chandelier illumination system for bimanual transconjunctival vitrectomy. Retina. 2008;28:518-519.
4. Sakaguchi H, Oshima Y, Nishida K, Awh CC. A 29/30-gauge dual-chandelier illumination system for panoramic viewing during microincision vitrectomy surgery. Retina. 2011; 31:231-1233.
5. Oshima Y, Awh CC, Tano Y. Self-retaining 27-gauge transconjunctival chandelier endoillumination for panoramic viewing during vitreous surgery. Am J Ophthalmol. 2007;143:166-167.
6. Leiderman YI. Endoillumination without an assistant: A technique to perform peripheral vitreoretinal surgery with chandelier endoillumination independently. Retina Specialist. 2018:1:34-35.
7. Todorich B, Stem MS, Hassan TS, Williams GA, Faia LJ. Scerla trans-illumination with digital heads up display: A novel technique for visualization during vitrectomy surgery. Oph Surg Lasers Imag Retina. 2018;49:436-439.
8. Veckeneer M, Wong D. Visualising vitreous through modified trans-scleral illumination by maximising the Tyndall effect. Br J Ophthalmol. 2009;93:268-270.
9. Peyman GA, Canakis C, Livir-Rallatos C, Easley J. A new wide-angle endoillumination probe for use during vitrectomy. Retina. 2002;22:242.



