 |
 |
Taking on a diabetic tractional retinal detachment can be daunting for any vitreoretinal surgeon. But careful preoperative planning and meticulous surgery can achieve good outcomes for these complex cases.
Preoperatively, we like to perform panretinal photocoagulation to the attached retina a few weeks before surgery and routinely inject bevacizumab (Avastin, Roche/Genentech) two to four days before surgery. We have a low threshold for cataract extraction before vitrectomy and prefer to avoid combined lensectomy/pars plana vitrectomy procedures.
First step
To start the case, we place 50% dextrose and viscoelastic on the cornea, which helps to maintain a clear view. A hybrid 23-ga
approach with a 27-ga instrument allows for more versatility with instrumentation. Newer beveled high-speed cutters perform better than ever at segmenting fibrovascular membranes close to the retina.
However, we still find tremendous value in using a blunt spatula to delaminate and vertical pneumatic membrane peeler-cutter scissors to dissect in tight planes (Video). A high-magnification lens can be very helpful for visualization and for avoiding iatrogenic breaks posteriorly. We use triamcinolone early on and again toward the end of the case to address any residual hyaloid that can serve as a scaffold for membrane reproliferation.
Relieving traction
Patience and persistence are key to relieving the tractional forces on the retina during these cases. It’s OK to leave residual pegs of fibrovascular membrane, as long as you address the associated traction. Sometimes the membrane may be too fused and inseparable from the retina and may require a focal retinectomy. If there are large plaques around breaks combined with proliferative vitreoretinopathy and vitreous-base contraction, consider a large (90- to 180-degree) retinectomy and a scleral buckle to relieve traction successfully.
At the end of the case, whether or not we find a break, we use a long-acting gas tamponade (C3F8 14 to 16%) with two to three weeks of face-down positioning. We reserve silicone oil only for cases with a large inferior retinectomy. This avoids recurrent vitreous hemorrhage mixing with oil, and long-term oil complications.
 |
Bottom line
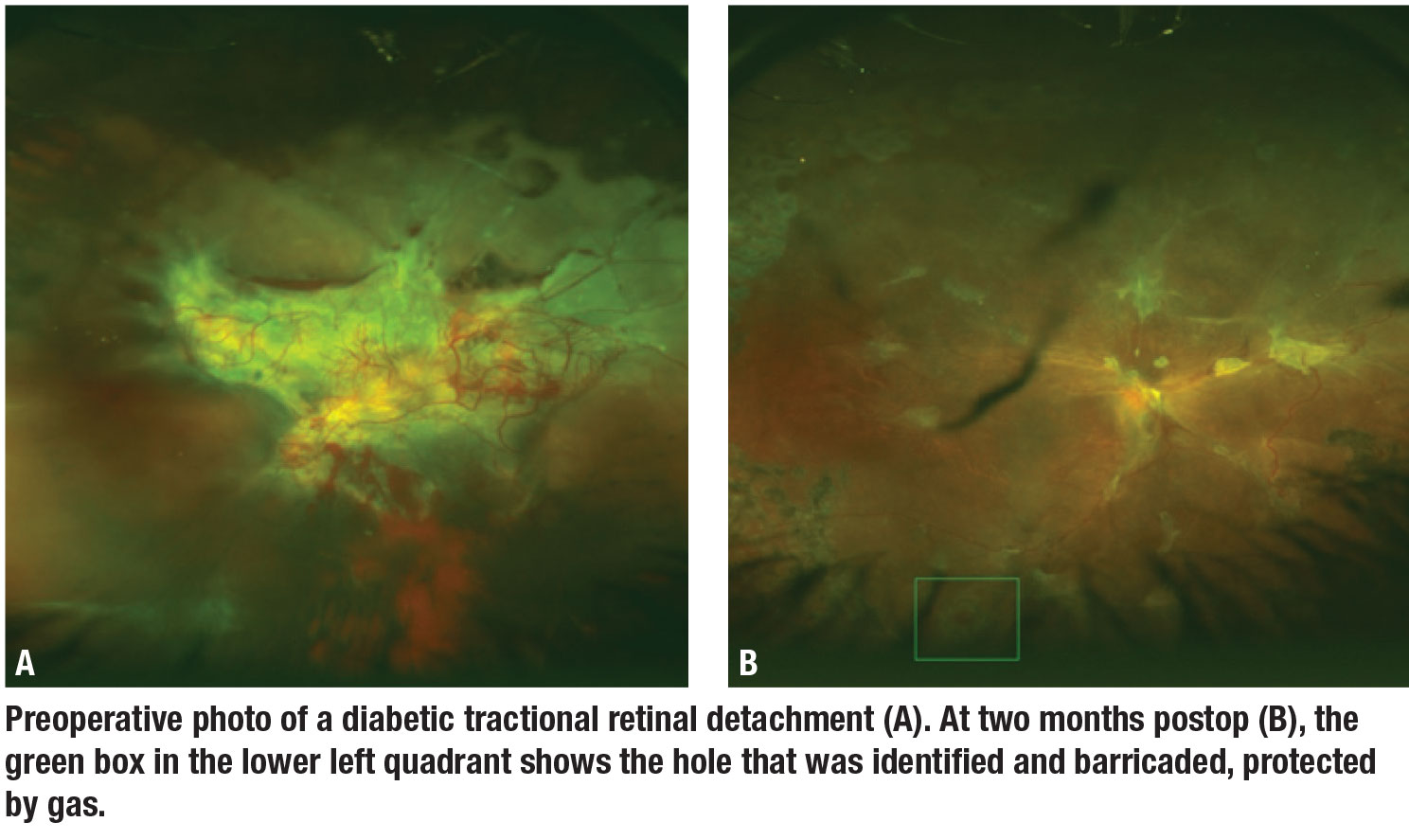
We’ve had excellent results with this approach, with a 98.6 percent single surgery reattachment rate in 69 consecutive diabetic TRD cases.1 The long-acting gas tamponade can protect from unseen breaks or those that develop from hot laser or stretching as residual membranes regress.
In one recent patient, we noted a new hole at postop week three as the C3F8 bubble was shrinking. The hole was located within the detached area and eluded notice intraoperatively. In this case, thankfully, the gas and positioning served to tamponade the new hole while subretinal fluid was reabsorbed in that area postoperatively. This helped to prevent any subretinal fluid around this inferior break which was subsequently easily barricaded in the office (Figure B, page 15). RS
REFERENCE
1. Sokol JT, Schechet SA, Rosen DT, Ferenchak K, Dawood S, Skondra D. Outcomes of vitrectomy for diabetic tractional retinal detachment in Chicago’s county health system. PLoS One. 2019 Aug 20;14:e0220726.




