In 2014 a physician could avoid a PQRS penalty by successfully reporting three measures. One year later, the Centers for Medicare & Medicaid Services (CMS) elevated the standard for successful reporting to nine different measures over three or more different National Quality Strategy (NQS) domains to avoid a penalty in 2017. Reporting options are:
• Claims.
• Registry.1
• Electronic health record (EHR).
• Measures group.
• Group practice reporting option Web Interface.2
Seven Measures for Ophthalmology
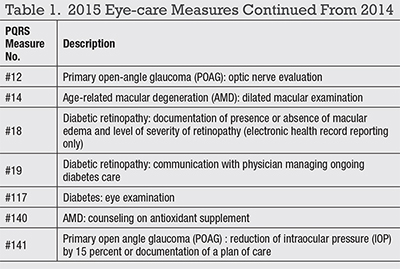
Hundreds of PQRS measures exist for all of medicine.3 From prior years, ophthalmology has seven measures (Table 1). Also, measure #18 changed in 2015 to direct reporting through an EHR; it is no longer available for claims-based or registry reporting.Further, CMS added a new requirement in 2015. Eligible professional (EPs) must report at least one cross-cutting measure (Table 2, page 42).4
For retina specialists, two new registry-based measures for rhegmatogenous retinal detachment repairs were added in 2015:
• #384 - Percentage of surgeries for primary rhegmatogenous retinal detachment where the retina remains attached after only one surgery.
• #385 - Percentage of rhegmatogenous retinal detachment cases achieving flat retinas six months post-surgery.
When submitting fewer than nine measures and/or fewer than three NQS domains, CMS uses the Measure-Applicability Validation (MAV) process5 to determine whether an EP should have reported quality data codes for additional measures and/or covered additional NQS domains.
Is it wise to allow CMS to determine if additional measures were applicable to your patient population? The most likely answer is “no” because MAV is an opaque process and CMS is doing the scoring.
How CMS Sets Penalties
The penalty for not successfully reporting PQRS in 2015 is a reduction of Medicare fee-for-service payment rates by 2 percent in 2017. Successful reporting for any solitary measure (not group) is achieved by reporting on at least 50 percent of the applicable Medicare Part B beneficiaries seen during the reporting period with the applicable diagnosis and CPT codes for each measure.6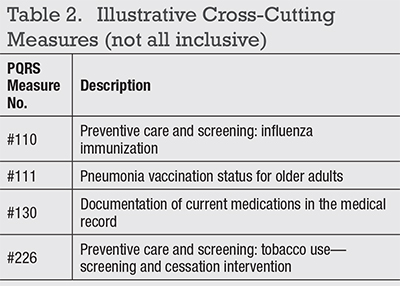
Making Sense of PQRS, VBPM
Unsuccessful reporting by large groups (10 or more EPs) with PQRS in 2014 results in a 2 percent PQRS penalty and a 2 percent VBPM penalty in 2016.Similarly, smaller groups that are unsuccessful with PQRS in 2015 could see 2 percent PQRS and 2 percent VBPM penalties in 2017. CMS is double dipping and using PQRS and VBPM to create a cumulative 4 percent penalty for failing PQRS.7
There is much more to describe about VBPM, and the next column will address that topic in greater detail. RS
Coming in November: Part 2: VBPM.
Mr. Mack is a senior consultant with Corcoran Consulting Group. He can be reached at (800) 399-6565 or at www.corcoranccg.com.
References
1. 2015 Physician Quality Reporting System Qualified Registries. Available at:https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/Downloads/2015QualifiedRegistries.pdf. Accessed August 7, 2015.
2. Physician Quality Reporting System Group Practice Reporting Option. Available at:
https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/Group_Practice_Reporting_Option.html. Accessed August 7, 2015.
3. 2015 Physician Quality Reporting Measure Codes. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/MeasuresCodes.html. Accessed August 7, 2015.
4. 2015 Cross-Cutting Measures List. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/downloads/2015_PQRS_CrosscuttingMeasures_12172014.pdf. Accessed August 7, 2015.
5. Physician Quality Reporting Analysis and Payment. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/AnalysisAndPayment.html. Accessed August 7, 2015.
6. Physician Quality Reporting System 2015 Implementation guide. Revised February 25, 2015. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/Downloads/2015_PQRS_ImplementationGuide.pdf. Accessed August 7, 2015.
7. Medicare FFS Feedback Program/Value Based Payment Modifier. Available at:
https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/valuebasedpaymentmodifier.html. Accessed August 7, 2015.



