 |
|
Bios Dr. Cruz-Pimentel is a vitreoretinal fellow at the University of Toronto. Dr. Mandelcorn is an associate professor of ophthalmology at the University of Toronto. DISCLOSURES: The authors have no relevant financial relationships to disclose. |
The term “adjuvant therapy,” derived from the Latin term adjuvāre, meaning “to help,” was first coined by Paul Carbone and his team at the National Cancer Institute in 1963.1 The use of preoperative adjuvant treatments in vitreoretinal surgery, such as for the use of anti-VEGF agents one to three days preoperatively in cases of advanced diabetic retinopathy, have been successfully applied.2
As retina specialists, one of the most common pathologies we face every day is rhegmatogenous retinal detachment. We recently introduced our approach to using preoperative gas for pars plana vitrectomy, or PGP technique, as an adjuvant therapy for PPV3 in the management of RRDs that are traditionally not considered to be candidates for pneumatic retinopexy.4 These include RRDs with multiple breaks in more than one quadrant, large breaks extending more than one clock hour and/or inferior breaks requiring PPV. The goal of PGP as an adjunct to PPV for repair of RRDs is to enhance the ease of surgery and improve functional and anatomical success.3
Our own experience
Our published case series included 109 eyes that underwent the PGP technique from 2016 to 2020,3 with a primary anatomical success rate of 95 percent and secondary anatomical success of 100 percent (including those with silicone oil tamponade removed) at last follow-up. Baseline visual acuity improved significantly at the last follow-up and most eyes (65 percent) achieved a final visual acuity of 20/50 or better. We noted preoperatively that PGP reduced the amount of peripheral subretinal fluid by at least 50 percent in bullous detachments.
In this article, we describe the PGP technique and highlight five major advantages and applications of the technique as an adjuvant in retinal detachment surgery.
Surgical technique
The PGP technique is performed starting with an anterior chamber paracentesis under topical anesthesia and sterile technique. Following this, we inject 0.6 mL sulfur hexafluoride (SF6) or 0.3mL perfluoropropane (C3F8) intravitreal gas into the superotemporal quadrant of the pars plana by placing the needle just internal to the scleral wall. We inject the gas away from the detached quadrant for very bullous RRDs to prevent subretinal gas migration.
Following gas injection, we advise patients to maintain a face-down position for four hours “to steamroll”5 the macular fluid to the periphery, and then in a position to tamponade the retinal break, usually flat on one side or the other. All of our patients underwent PPV within approximately one week following PGP.
Special considerations in the OR
|
Ideal candidates for preoperative gas for PPV
|
We advise taking special considerations in the operating room. The phakic eye is prepared and draped quickly to decrease any lens opacification that can develop while the patient is supine. Moreover, gas removal should be done right at the beginning of the surgery.
At the start of PPV, the preoperative gas bubble is removed through the trocar cannula as the blade is retracted through the valve of the superonasal or superotemporal trocar, with the eye tilted to its most superior position, as demonstrated in this video: www.aao.org/1-minute-video/tips-gas-removal-in-phakic-eye-after-pneumatic-ret.
Fluid-air exchange (FAX) using a backflush cannula is then done through the primary break without perfluorocarbon (PFO) liquid-assisted drainage. Retinal breaks are lasered in the attached retina prior to FAX, while breaks in the detached retina are lasered after the FAX. The vitreous cavity air is flushed with either SF6 or C3F8 gas. Patients are advised to maintain a side or face-down position immediately after PPV.
An illustration of the PGP technique and its applications can be found in the accompanying video.
The five major takeaways
1.PGP protects the macula in both macula-off and macula-on RRDs
The PGP approach in RRDs with combined inferior and superior breaks promotes reattachment of the macula in most cases. We believe that PGP is essential to ensure timely management of RRDs and faster restoration of central vision. The more rapid reattachment of the macula likely results in a better visual outcome.
 |
|
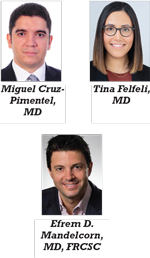
Figure 1. Representative case of a 66-year-old pseudophakic patient with a history of previous tears treated with cryotherapy. The patient had a Soemmering’s ring (A), which limited the view of the posterior segment during the examination and a macula-off rhegmatogenous retinal detachment (B). The patient underwent preoperative gas (PGP technique) during pars plana vitrectomy, and inferior holes were found and treated with laser. At two weeks postoperatively, color fundus photos (C) and autofluorescence image (D) demonstrated good anatomical outcomes. |
Studies have shown that repairing macula-off detachments within three days is critical for preserving vision.6,7 Presumably, this implies that rapid macular reattachment, especially in situations where operating room access is limited, can give patients the best chance at improved central vision postoperatively. In cases of macula-on detachments, PGP can protect the macula from going macula-off until OR access is available (Figure 1).
2. PGP reduces the amount of subretinal fluid that needs to be drained in vitrectomy
By making RRDs less bullous and less mobile, PGP allows the surgeon to perform a better shave of the vitreous prior to fluid-fluid exchange or FAX. The reduced amount of residual SRF at the conclusion of surgery can also reduce the amount of posterior migration of SRF into the macula during FAX. Reduced residual SRF can help mitigate the risk of developing retinal folds postoperatively.
A reduction in SRF prior to the PPV also has the benefit of decreasing the need for PFO liquids, with reduced surgical cost and morbidity associated with inadvertently retained PFO—such as postoperative inflammation, raised intraocular pressure and photoreceptor and retinal pigment epithelium atrophy.8
3. PGP reduces the risks associated with choroidal detachments
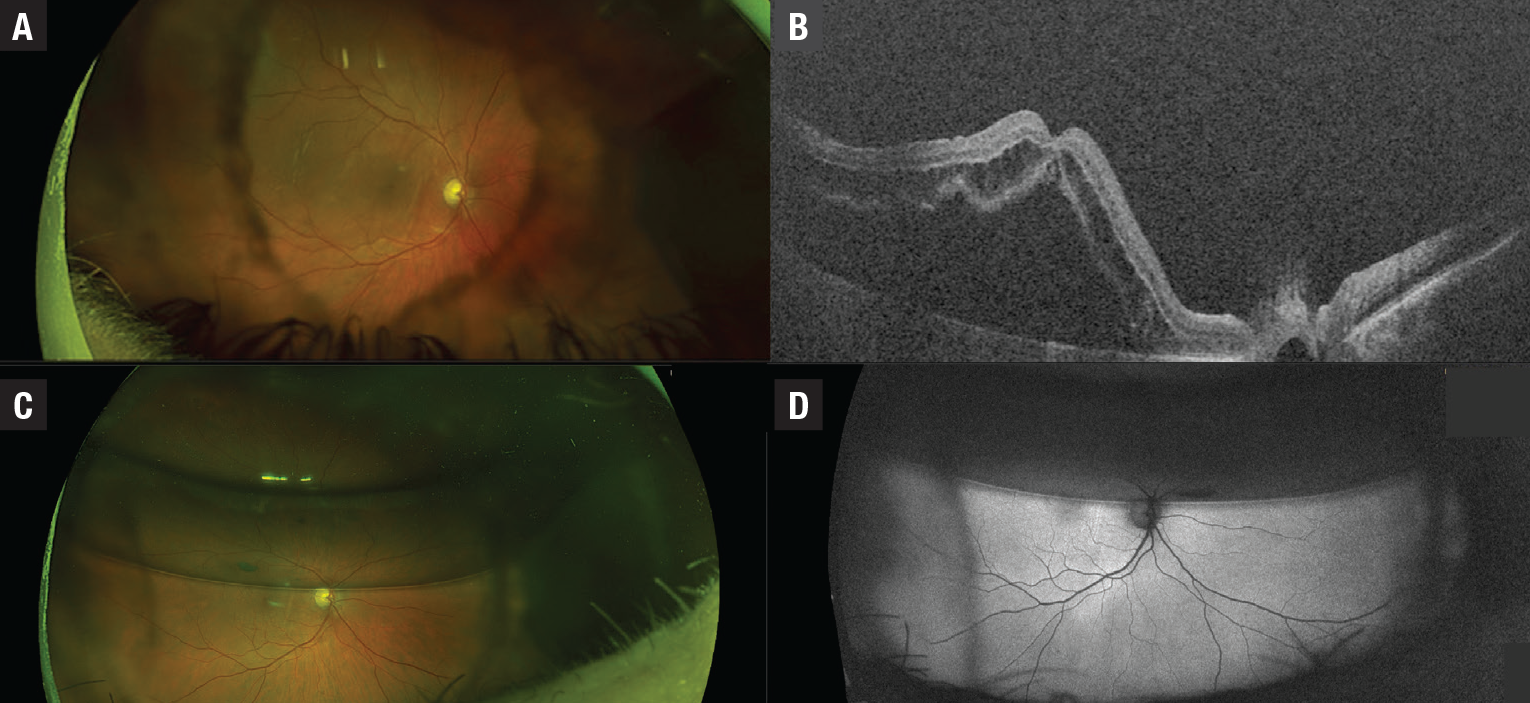
In patients with associated choroidal detachments, PGP can reduce or eliminate the detachment, which can lessen the risk of redetachment due to underfill when silicone oil is needed as a tamponade. Additionally, PGP can often partially resolve a choroidal detachment, which can diminish the likelihood of placing the trocars or infusion cannula in the suprachoroidal space (Figure 2).
 |
|
Figure 2. Representative case of a 65-year-old patient with a macula-off rhegmatogenous retinal detachment with an associated choroidal serous detachment and posterior vitreous detachment grade A with superior and inferior breaks (A and B). On day four following preoperative gas, the choroidal detachments resolved and the macula reattached with persistent fluid inferiorly due to inferior breaks and good laser barricade around the superior break (C and D). The patient underwent pars plana vitrectomy on day five following the initial presentation. |
4. PGP improves ease of repair for detachments associated with full-thickness macular holes
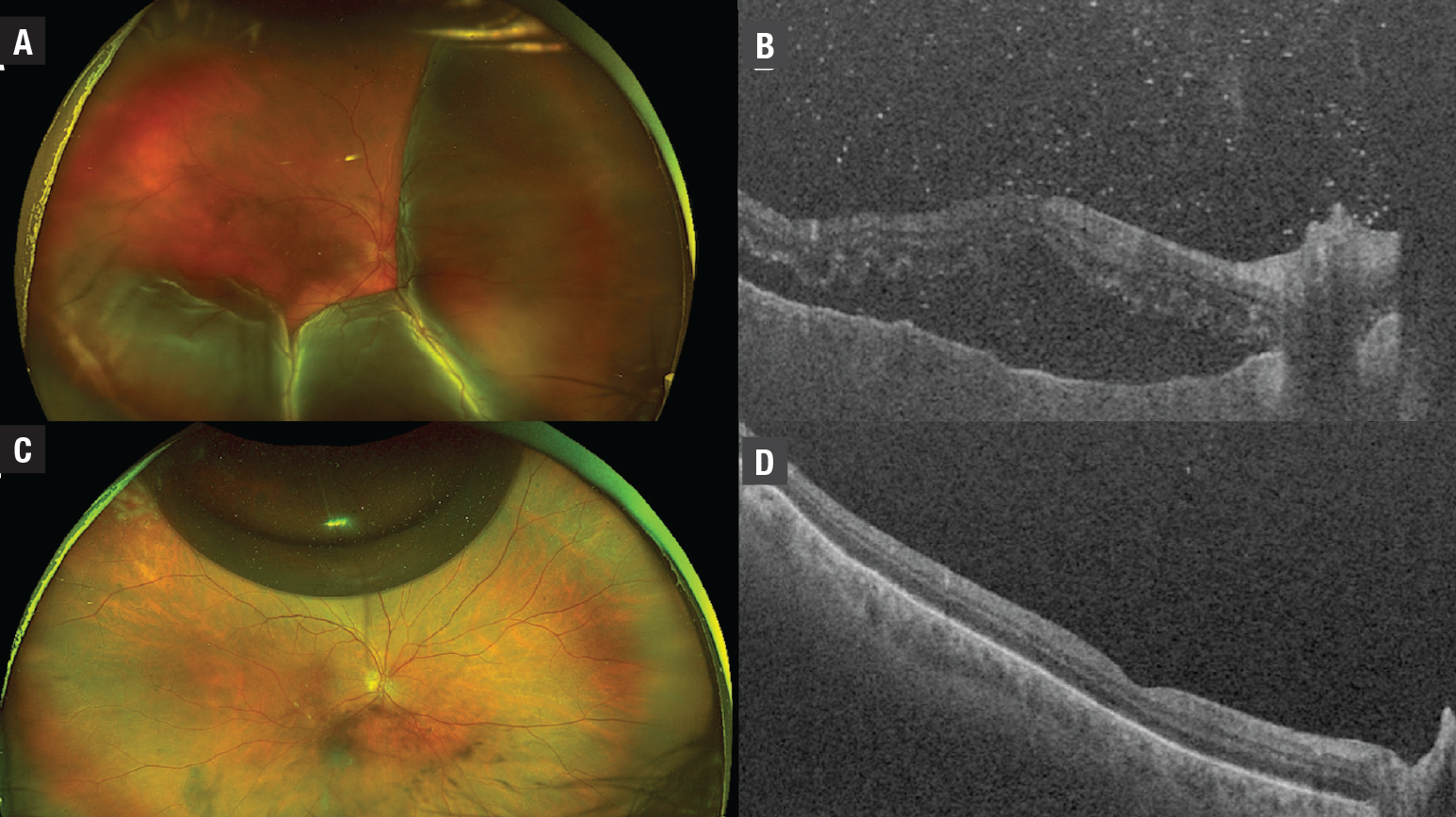
In cases of retinal detachment with an associated full-thickness macular hole (FTMH), PGP allows for macular (and macular hole) reattachment preoperatively, which can reduce the risk of subretinal injection of tissue-staining agents (indocyanine green or Brilliant Blue). It can also ease the peeling of the internal limiting membrane. In the case illustrated in Figure 3, macular reattachment is achieved with PGP, simplifying the ILM peel around the macular hole intraoperatively.
 |
|
Figure 3. Representative case of a 62-year-old patient with congenital deafness who presented with a rhegmatogenous retinal detachment with several breaks in the temporal quadrant and a full-thickness macular hole in the right eye (A and B). The preoperative gas (PGP technique) with pars plana vitrectomy technique was used, followed by laser retinopexy at 48 hours (C and D). The patient also underwent PPV with internal limiting membrane peel within one week. Postoperatively, this complex case had a good anatomical outcome (E and F). |
5. PGP is a timely and simple technique that can easily be incorporated into a retina surgeon’s practice
PGP is an office-based technique that’s a timely intervention in situations where the OR can’t be accessed immediately due to availability of resources. Moreover, PGP is easy for surgeons to incorporate into their practice, even if they have minimal experience with pneumatic retinopexy. For surgeons who often choose PPV as their primary RRD repair modality, PGP is an excellent option. PGP takes advantage of both the high anatomical success rates of PPV for RRD and the high functional success rates of pneumatic retinopexy. The PGP technique nicely marries these two options by optimizing both.
 |
Bottom line
Overall, the PGP technique may provide good anatomic and functional outcomes in cases in which pneumatic retinopexy isn’t suitable, including multiple large breaks in more than one quadrant, and/or inferior breaks, retinal detachments with associated macular holes, presence of large bullous choroidal detachments, unidentifiable breaks and media opacity due to vitreous hemorrhage.
The PGP technique with PPV for rhegmatogenous retinal detachments can easily be incorporated into the retina specialist’s routine surgical practice, based on the advantages that we’ve outlined here.
Surgeons from the United Kingdom, Max Davidson and Aman Chandra, who have successfully adapted this technique, have found that implementing PGP marries the anatomical and functional benefits of pneumatic retinopexy and PPV, achieving good results in both simple and complicated RRDs.9 RS
REFERENCES
1. The emperor of all maladies: A biography of cancer. Can Fam Physician. 2011;57:460.
2. Wang D, Zhao X, Zhang W, Meng L, Chen Y. Perioperative anti-vascular endothelial growth factor agents treatment in patients undergoing vitrectomy for complicated proliferative diabetic retinopathy: a network meta-analysis. Sci Rep. 2020;10:18880.
3. Felfeli T, Mandelcorn MS, Trussart R, Mandelcorn ED. Preoperative gas for pars plana vitrectomy: a surgical technique for repair of rhegmatogenous retinal detachments with multiple, large or inferior breaks. Retin Cases Brief Rep. Published online October 1, 2021. doi:10.1097/ICB.0000000000001197
4. Mandelcorn ED, Mandelcorn MS, Manusow JS. Update on pneumatic retinopexy. Curr Opin Ophthalmol. 2015;26:194-199.
5. Yanyali A, Horozoglu F, Bayrak YI, Celik E, Nohutcu AF. Steamroller versus basic technique in pneumatic retinopexy for primary rhegmatogenous retinal detachment. Retina. 2007;27:74-82.
6. Greven MA, Leng T, Silva RA, et al. Reductions in final visual acuity occur even within the first 3 days after a macula-off retinal detachment. Br J Ophthalmol. 2019;103(10):1503-1506.
7. Frings A, Markau N, Katz T, et al. Visual recovery after retinal detachment with macula-off: Is surgery within the first 72h better than after? Br J Ophthalmol. 2016;100:1466-1469.
8. Elsing SH, Fekrat S, Green WR, Chang S, Wajer SD, Haller JA. Clinicopathologic findings in eyes with retained perfluoro-n-octane liquid. Ophthalmology. 2001;108:45-48.
9. Davidson M, Chandra A. Temporising pneumatics for the initial management of rhegmatogenous retinal detachment. Eye (Lond). 2022 Jan 13. doi: 10.1038/s41433-021-01927-x. Epub ahead of print. PMID: 35027709.




