Evaluation and Preparation
Patients with intraocular fishhook injuries will often not tolerate adequate in-office examination. Imaging studies including X-ray and/or CT scanning may be useful to localize the foreign body. Keep these patients NPO and arrange for emergent evaluation under anesthesia in the operating room and initiate a typical ruptured globe protocol. Administer systemic and intraocular antibiotics and tetanus (if not up to date), and avoid unnecessary manipulation of the eyelids and globe.
Surgery
When planning for removal of a fishhook from an eye, consider these situations in advance:
• Is the hook barbed? Barbed hooks may preclude safe removal from the original entry wound, because retrograde removal of the barb will significantly damage the wound architecture.
• Is there an exit site? With a
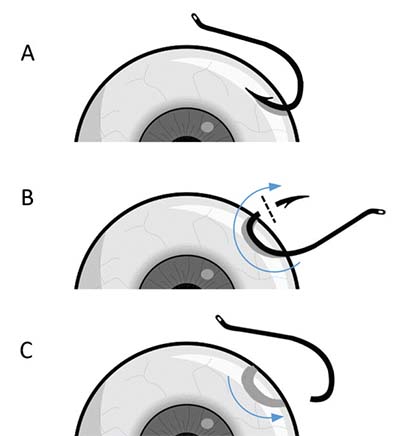 |
| Figure. In the advance and cut maneuver the fishhook is advanced through an exit wound (A), the barb is cut (B), and the fishhook is retracted through the original entry wound. Courtesy Louis Cai, BS, and Justin Ma, BS |
• How thick are the hook and barb? Often the patient or family members and friends will have an identical hook or a picture to show you. Even without this useful information, plan for the worst and be prepared with the appropriate tools. Most ophthalmology instruments will not be able to cut even small-gauge hooks. Ask the operating room staff to obtain sterile large-gauge wire cutters or rod cutters that may be available in otolaryngology, neurosurgery or orthopedic surgical trays. Having these available at the start of the case will help avoid unnecessary delays (and sweating on the part of the surgeon) if one’s first option fails to cut the barb.
As always, surgical planning is the key to success. While penetrating or perforating ocular injuries are often associated with a poor prognosis, this advance-and-cut technique can help elegantly remove a barbed fishhook to maximize visual outcomes. We hope not to see this, but should be prepared if we do! RS
Dr. Hahn is an associate at New Jersey Retina in Teaneck. Dr. Sridhar is assistant professor of ophthalmology at Bascom Palmer Eye Institute, Miami, and formerly a fellow at Wills Eye Hospital, Philadelphia. Mr. Cai is a medical student at the University of Miami Miller School of Medicine. Dr. Flynn holds the J. Donald M. Gass Distinguished Chair in Ophthalmology at Bascom Palmer. Dr. Sivalingam is with Mid Atlantic Retina and fellowship director of the retina service at Wills Eye Hospital, Philadelphia.
REFERENCES
1. Chao DL, Erickson BP, Rachitskaya AV. Penetrating ocular fishhook injury. JAMA Ophthalmol. 2015;133:347-348.
2. Aiello LP, Iwamoto M, Taylor HR. Perforating ocular fishhook injury. Arch Ophthalmol. 1992;110:1316-1317.




