The patient was hospitalized with a fractured femur and fat emboli to the lungs bilaterally. He’d reported normal vision until the day after the fall, when he developed photopsias for several hours and subsequent bilateral central scotomas with reduced visual acuity.
The patient’s ocular history included bilateral cataracts with baseline vision of 20/50 OD and 20/30 OS, attributed to prior use of systemic corticosteroids. He had never had ocular surgery or taken any ocular medications. Aside from restricted mobility related to his Duchenne muscular dystrophy (DMD), his medical history was otherwise unremarkable.
Examination
Best-corrected visual acuity was 20/60 and 20/40 with intraocular pressures of 16 mm Hg and 24 mm Hg in the right and left eyes, respectively. No afferent pupillary defect was present, visual fields were full to confrontation and ocular motility was normal in both eyes. The anterior segment was normal with exception of bilateral 3+ central posterior subcapsular cataracts and cortical lenticular opacities.
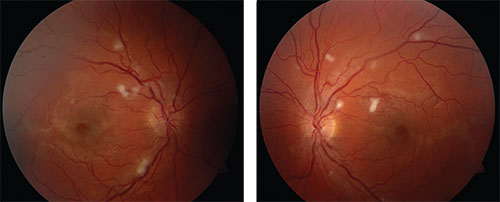 |
| Figure 1. Color fundus photographs show bilateral cotton wool spots near the vascular arcades in both eyes as well as loss of the foveal light reflex and grayish opacification of the retina near the fovea. |
The vitreous was normal bilaterally. Fundus examination of the right eye revealed cotton wool spots (CWS) located primarily along the superior and inferior arcades adjacent to but not overlying the retinal arterioles. A few small CWS along the vascular arcades were evident nasally. Additionally, the fovea had a grayish opaque appearance with loss of the normal foveal light reflex. The dilated fundus exam of the left eye showed a similar appearance (Figure 1). No hemorrhages or optic nerve head edema were noted.
Workup, Diagnosis And Management
Because the patient could not sit for a desktop optical coherence tomography (OCT) test due to his injuries, we performed a handheld OCT that demonstrated no gross intraretinal or subretinal fluid but did show hyper-reflective intraretinal lesions (Figure 2). We deferred further workup given the strong clinical suspicion for fat embolism to the retinal microvasculature leading to a Purtscher-like retinopathy.
After his hospital discharge, we evaluated the patient at the University of Washington Eye Institute clinic, where we documented fewer and smaller CWS since discharge as well as improved visual acuity. We did not obtain fluorescein angiography due to patient positioning restrictions and strong clinical suspicion. We arranged for monitoring with clinical exams at one, two and six months post-injury per the published recommendations for patients with this condition.1
Discussion
Purtscher-like retinopathy is a rare occlusive vasculopathy. The classical manifestations are bilateral white retinal lesions, CWS and posterior-pole hemorrhage.
Differentiated from Purtscher’s retinopathy, originally described as following compressive trauma to the head or chest, Purtscher-like retinopathy can arise from other systemic insults. These include acute pancreatitis, fat embolism syndrome, chronic renal failure, amniotic fluid embolism from childbirth, connective tissue disorders, cryoglobulinemia, weightlifting, shaken-baby syndrome, retrobulbar anesthesia and orbital steroid injection, among other causes.2
Cl
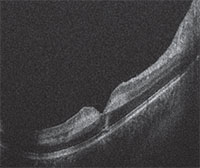 |
| Figure 2. Handheld optical coherence tomography imaging of the macula (right eye shown here) demonstrated foveal contour preservation with alteration of the normal retinal architecture. Imaging showed a hyper-reflective lesion of the inner nuclear and outer plexiform layers, but no gross intraretinal or subretinal fluid. |
The etiology of Purtscher’s and Purtscher-like retinopathy is not well understood, but is likely secondary to embolic occlusion of arterioles. However, authors have proposed numerous etiologies, including vasculitis, raised intrathoracic pressure or, as Otmar Purtscher originally postulated, raised intracranial pressure and extravasation of lymphatic material from the retinal vessels.3
The physical examination of these patients typically features bilateral, multiple peripapillary CWS and superficial hemorrhages adjacent to the retinal arterioles. Purtscher flecken are polygonal shaped superficial retinal white lesions with a clear zone adjacent to vessels and are considered pathognomonic, but only occur in approximately 50 percent of cases.1,4
Less common findings include optic disc swelling, serous macular detachment, dilated tortuous vessels, hard exudates, optic disc edema and relative afferent pupillary defects.
Findings typically lag behind the inciting event by 24 to 48 hours, similar to the onset of symptoms. The CWS of Purtscher-like retinopathy due to fat embolism, as in this case, are generally smaller and located more peripherally in the retina than in classic Purtscher’s retinopathy.5
Imaging and Systemic Workup
Fluorescein angiography demonstrates nonperfusion of the small retinal capillaries in the regions corresponding to the retinal whitening, and, in some patients, delayed filling of vessels, late leakage and peripapillary leakage.1 OCT may demonstrate hyper-reflectivity at the inner plexiform layer and inner nuclear layer, as it did in our case.6
In cases without trauma but with a characteristic fundus appearance, the systemic workup should include a detailed history and physical exam in addition to a basic metabolic panel, amylase, lipase, complete blood count and imaging as indicated. Purtscher’s and Purtscher-like retinopathy are clinical diagnoses, thus, a working differential is in order.
Other conditions with a similar fundus appearance include central retinal vein occlusion, central retinal artery occlusion and commotio retinae. Supportive care with treatment of the underlying condition is the only recommended management. While some authors have reported treatment with systemic steroids, controlled studies are lacking and retrospective reports have not shown statistically significant improvement in vision.1,3
Retinal lesions generally resolve spontaneously within one to three months, replaced with attenuation of vessels, temporal disc pallor or mottling of the retinal pigment epithelium.2 Visual acuity recovery is variable, but returns to baseline in at least 50 percent of patients, with a better prognosis for patients without associated macular edema.1
A variety of retinal findings have been reported in patients with DMD. One report described a vascular retinopathy, which may include capillary dropout, saccular venular aneurysms, neovascularization and vitreous hemorrhage.7
Additionally, patients with DMD have been found to have electroretinogram (ERG) abnormalities, including a reduced ß-wave or even a negative waveform, similar to congenital stationary night blindness.
 |
Patients with DMD, however, do not report nyctalopia.5 This ERG response is believed to arise from abnormal neurotransmission between photoreceptors and optic nerve-bipolar cells due to the localization of dystrophin to the outer plexiform layer and its presumed role in neurotransmission.8
Some patients with DMD have also exhibited a pigmentary retinopathy, but there is debate in the literature whether these conditions are associated. Prior to his injury, our patient was reportedly free of any overt retinal disease, and we do not believe that his DMD predisposed him to the Purtscher-like retinopathy he developed. RS
REFERENCES
1. Miguel AI, Henriques F, Azevedo LF, et al. Systematic review of Purtscher’s and Purtscher-like retinopathies. Eye (Lond). 2013;27:1-13.
2. Agrawal A, McKibbin MA. Purtscher’s and Purtscher-like retinopathies: a review. Surv Ophthalmol. 2006;51:129-136.
3. Agrawal A, McKibbin M. Purtscher’s retinopathy: epidemiology, clinical features and outcome. Br J Ophthalmol. 2007;91:1456-1459.
4. Proença Pina J, Ssi-Yan-Kai K, de Monchy I, et al. [Purtscher-like retinopathy: case report and review of the literature]. J Fr Ophtalmol. 2008;31:609-613.
5. McCannel CA e. 2015-2016 Basic and Clinical Science Course (BCSC), Section 12: Retina and Vitreous. San Francisco, CA: American Academy of Ophthalmology;2015.
6. Coady PA, Cunningham ET, Vora RA, et al. Spectral domain optical coherence tomography findings in eyes with acute ischaemic retinal whitening. Br J Ophthalmol. 2015;99:586-592.
7. Hahn P, Lin P, Fekrat S. Ultra-widefield imaging of Duchenne muscular dystrophy-associated proliferative retinal vasculopathy improved with panretinal laser photocoagulation alone. Ophthalmic Surg Lasers Imaging Retin. 2013;44:293-295.
8. Pillers DA. Dystrophin and the retina. Mol Genet Metab. 1999;68:304-309.



