 |
The management of primary rhegmatogenous retinal detachment is at the heart of surgical retina practice. Yet, retinal detachment repair remains the subject of significant controversy, with various eminent surgeons strongly advocating one approach over another.
The management of routine RRD can vary widely, from pneumatic retinopexy to combined vitrectomy plus scleral buckle as the standard of care from one academic institution to the next. Part of the reason for the lack of consensus has been the limited evidence base surrounding retinal detachment repair. Only a handful of randomized trials have demonstrated the benefits of one procedure over another for certain morphologies of RD.
Besides the intrinsic difficulties of performing a randomized controlled trial for an emergency surgical procedure, interpretation of the results can be challenging, because they are really only applicable to the specific inclusion and exclusion criteria of the study in question. For a randomized trial to be useful, the results must be generalizable to a significant proportion of patients with RD.
 |
Purpose of PIVOT
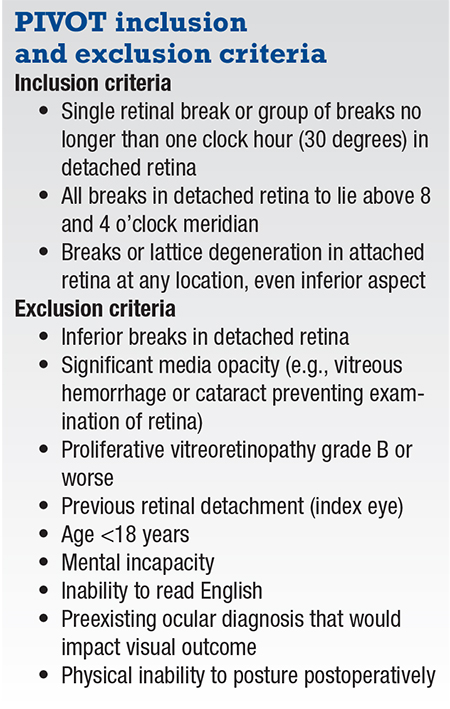
With this in mind, we designed the PIVOT study, a randomized controlled trial that compared pneumatic retinopexy to pars plana vitrectomy, specifically for patients with retinal detachments with one or more breaks in detached retina within one clock hour, in the superior eight clock hours.1 These inclusion criteria were intended to replicate the inclusion criteria of the Pneumatic Retinopexy Trial performed almost 30 years ago that demonstrated favorable visual acuity results for pneumatic retinopexy compared to scleral buckle.2
However, to make the results more generalizable, we included patients with any number, location and size of breaks or lattice degeneration in attached retina. We estimate that inclusion of these features makes the results of the PIVOT trial applicable to approximately one-third of RD patients.
Another key aspect of the trial design was to minimize sources of bias. Specifically, we were careful to perform vitrectomies as fast as possible. Because pneumatic retinopexy is an in-office procedure, we sought to avoid comparing pneumatic retinopexy performed immediately vs. vitrectomy performed a week later. The protocol required macula-on cases to be done within 24 hours and macula-off patients within 72 hours.
It turned out that the mean time to surgery was eight hours for macula-on patients and 22 hours for macula-off cases, which we believe exceeded current standard practice.
Managing cataract formation
Another major issue with any trial involving vitrectomy is the development of cataract. We went to great lengths to identify and treat visually significant cataracts as soon as they occurred. This led to 65 percent of phakic patients in the vitrectomy arm undergoing cataract surgery during the study. Of course, a minority of patients with lens opacity opted not to proceed with cataract surgery—a reality of everyday surgical retina practice.
In the end, we believe that our endeavors to remove clinically significant cataracts from the vitrectomized patients likely biased the visual outcomes in favor of the vitrectomy arm, as evidenced by the overall higher cataract grading scores in the pneumatic retinopexy arm at one year.
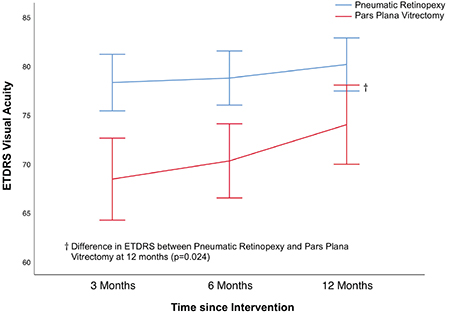 |
| Figure. Graph shows pneumatic retinopexy was superior to pars plana vitrectomy in terms of Early Treatment Diabetic Retinopathy Study visual acuity in intention- to-treat groups at three, six and 12 months of follow-up. (Used with permission Elsevier Science and Technology Journals. Hillier RJ, Felfeli T, Berger AR, et al. Ophthalmology. 2018 Nov 22. Epub ahead of print.) |
Pneumatic retinopexy superior
PIVOT demonstrated superior visual acuity results for pneumatic retinopexy compared to pars plana vitrectomy at every time point, and by 4.9 Early Treatment Diabetic Retinopathy Study letters at one year (p=0.024, Figure). The proportion of patients who had better than 70 ETDRS letters (20/40) visual acuity was 90.3 percent in the pneumatic retinopexy group vs. 75.3 percent in the vitrectomy group.
Scores for the 25-item National Eye Institute Visual Function Questionnaire were superior for pneumatic retinopexy compared to vitrectomy at three and six months, with no significant difference at one year. There were no significant differences in the proportion of patients who required additional vitrectomy for macular pucker, macular hole or vitreous debris.
Primary anatomical reattachment rates were 80.8 percent for pneumatic retinopexy vs. 93.2 percent for vitrectomy (p<0.045). We anticipated this difference in reattachment rates. It was important to see that patients with a failed pneumatic retinopexy still had very good visual acuity outcomes following PPV (average 20/40 visual acuity). In other words a failed pneumatic retinopexy didn’t jeopardize final visual acuity outcome. Specifically, secondary reattachment rates were 99 percent in both groups.
What was most interesting was that objectively measured vertical distortion was significantly less following pneumatic retinopexy compared to vitrectomy. The reduced vertical distortion with pneumatic retinopexy suggests differences in the mechanism and quality of the retinal reattachment.
 |
At the American Society of Retina Specialists and EURETINA meetings in 2018, we demonstrated that patients who underwent pneumatic retinopexy had significantly less disruption of the interdigitation zone, ellipsoid zone and the external limiting membrane on optical coherence tomography imaging compared to PPV.3,4
After carefully interpreting the results of the trial, we believe the superiority of pneumatic retinopexy over vitrectomy is likely multifactorial and related to more than the disparity in cataract formation.
Pneumatic retinopexy benefit
The ability to perform pneumatic retinopexy swiftly—potentially in the office, with the need for minimal specialist equipment—and thus reattach the macula within a couple of hours, quickly reestablishing the integrity of the retina-RPE interaction, is likely an advantage.
Furthermore, distortion and optical coherence tomography results suggest that pneumatic retinopexy is associated with a superior quality of retinal reattachment. We believe that the more natural reabsorption of the subretinal fluid by the RPE pump in pneumatic retinopexy likely provides an advantage over the forced drainage that occurs during vitrectomy. Multimodal imaging studies by our group are currently underway which will provide clarity on these differences in the near future.
PIVOT has helped fill a gap in our current knowledge regarding the differences between pneumatic retinopexy and PPV for routine primary RRD. The superior visual acuity and distortion results suggest a definite advantage for pneumatic retinopexy.
The bottom line
An often-cited drawback of pneumatic retinopexy is the lower primary anatomical reattachment rate. The difference for patients in this trial was 12 percent. This yields a number needed to treat of 8.33. In other words, proponents of a vitrectomy-first approach on the basis of reattachment rates would be advocating for approximately eight patients to undergo vitrectomy surgery rather than pneumatic retinopexy, to save one patient from incurring a failed pneumatic retinopexy, thereby subjecting the remaining seven patients to potentially avoidable cataract surgery and inferior functional outcomes. This despite the knowledge that a patient with a failed pneumatic retinopexy is likely to achieve a final visual acuity outcome similar to a patient having undergone vitrectomy from the outset.
As with everything in life, RD outcomes ought not to be only about the quantity, but quality. The majority of our patients value their final visual outcomes above anything, and that is what we should strive to optimize.
REFERENCES
1. Hillier RJ, Felfeli T, Berger AR, et al. The Pneumatic Retinopexy vs. Vitrectomy for the management of Primary Rhegmatogenous Retinal Detachment Outcomes Randomized Trial (PIVOT). Ophthalmology. 2018 Nov 22. Epub ahead of print.
2. Tornambe PE, Hilton GF. Pneumatic retinopexy. A multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. The Retinal Detachment Study Group. Ophthalmology. 1989;96:772–783; discussion 784.
3. Muni R. Difference in metamorphopsia and OCT changes after retinal detachment repair: RCT comparing pneumatic retinopexy to vitrectomy at 1 year. Paper presented at American Society of Retina Specialists; Vancouver, BC: July 25, 2018.
4. Hillier R, Felfeli T, Juncal V, Lampert Monte Francisconi C, Mak M, Muni R. Metamorphopsia and OCT changes following retinal detachment repair: Pneumatic retinopexy versus vitrectomy (“PIVOT” 1-year data). Paper Presented at EURETINA: Vienna, Austria; September 21, 2018.




