Briefly, this technique involves creating sclerotomies at 12 and 6 o’clock to externalize the haptics of a three-piece IOL, then passing the haptics through and securing them in an adjacent scleral tunnel (Video). I have always had difficulty with this technique as originally described. I found the approach to be technically challenging, and I often discovered IOL decentration in the immediate postoperative period.
In this article, I have the opportunity to share pearls from these two surgeons, who have each taken slightly different approaches to address these difficulties.
Safely Externalize Haptics
One technical challenge is safe externalization of the haptics. Drs. Feiner and Prenner emphasize the need for a generous sclerotomy length. During externalization, Dr. Feiner uses internal limiting membrane-style forceps to “lasso” the haptic rather than directly grasping it to minimize damage.
If it is necessary to directly grab the haptic, Dr. Prenner will use a “handshake” technique to grasp the haptic tip directly with end-grasping forceps. Both feel that three-piece IOLs that have been in longer than five years have a significantly higher risk of haptic-optic separation. They prefer to exchange rather than rescue these lenses.
 |
Pass Haptics Through Tunnels
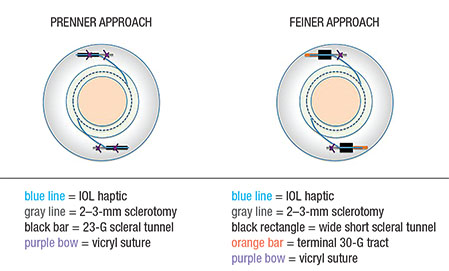
Another technical challenge is safely passing the haptics through the tunnels. Dr. Prenner now uses Scharioth forceps (Dutch Ophthalmic USA) that have a longitudinal groove along their grasping end. When the forceps are closed, the tip is buried in the groove, and the closed forceps form a bullet-shaped end that minimizes the risk of engaging scleral fibers in the tunnel, for smooth passing.
Dr. Feiner has modified his approach and now instead creates 1.5-mm long scleral tunnels using an angled Beaver blade (Beaver-Visitec), as with tunnels for scleral buckling. The additional space in this wider and shorter tunnel makes passing of the haptics easy. These are placed prior to sclerotomy creation, in contrast to Dr. Prenner’s 3-mm, 23-G tunnels, which are placed after.
Unexpected IOL Decentration
A final difficulty is unexpected IOL decentration or tilt in the immediate postoperative period.
| Watch the Video Jonathan Prenner, MD, describes important pearls to complete difficult steps in sutureless scleral fixation in a video available at: https://player.vimeo.com/video/168847970 |
To prevent this, Dr. Prenner now places a 7-0 vicryl suture in the middle of the 23-G scleral tunnel around the haptic to secure it while the sclera fibroses in.
In contrast, Dr. Feiner passes his externalized haptics (once passed through his wide but shorter scleral tunnels) through a 30-G needle tract that he creates as the last step. He directs the needle path based on haptic position once the IOL is centered to allow the haptics to sit naturally, as he believes committing to haptic positioning prior to placing the IOL is more likely to result in malpositioning.
Sutureless scleral IOL fixation is an important technique to maintain in a vitreoretinal surgeon’s armamentarium. In addition to the approaches outlined here, a conjunctiva-sparing cannula-based approach and many others have been reported.2 I encourage surgeons to try these various approaches. Read the literature, talk to surgeons who have performed them and make your own modifications to make this technique work for you. RS
Dr. Hahn is an associate at New Jersey Retina in Teaneck, where Drs. Prenner and Feiner are partners. Dr. Prenner is also an associate clinical professor at Rutgers New Jersey Medical School, Newark.
Disclosures: Dr. Hahn serves as a consultant for Second Sight Medical Products and Bausch + Lomb.
REFERENCES
1. Prenner JL, Feiner L, Wheatley HM, Connors D. A novel approach for posterior chamber intraocular lens placement or rescue via a sutureless scleral fixation technique. Retina. 2012;32:853-855.
2. Abbey AM, Hussain RM, Shah AR, Faia LJ, Wolfe JD, Williams GA. Sutureless scleral fixation of intraocular lenses: outcomes of two approaches. The 2014 Yasuo Tano Memorial Lecture. Graefes Arch Clin Exp Ophthalmol. 2015;253:1-5.




